Fig. 14.1
Anatomy of internal thoracic artery
The ITA, opposite to the origin of the vertebral artery from the subclavian artery, diverges in almost a straight line vertically downward. The ITA courses with the phrenic nerve and then reaches the upper edge of the first rib. At this level, the ITA crosses the phrenic nerve and descends along with two accompanying veins in the space between the intercostal muscle and endothoracic fascia and rib in the posterior surface of the anterior chest wall approximately 1 cm distal to the sternal edge. However, the two accompanying veins merge at the cephalic site from the first intercostal space, and the single vein usually runs distally from the ITA. The brachiocephalic vein extends to the cephalic and lateral sites from the upper edge of the first rib. This vein is located between the medial side (laterally) and the anterior side (frontally) of the ITA. On the other side, since the transversus thoracis muscle often develops in the caudal site from the level of the fourth intercostal space and the fifth rib, the continuity of the transversus thoracis muscle makes the endothoracic fascia unclear. The ITA divides into the superior epigastric artery and musculophrenic artery at the level of the sixth rib and intercostal space.
There are three main branches of the ITA, which diverge into three different directions: (1) the sternal branch which courses to the median side (dorsum of the sternum), (2) the perforating branch which penetrates through the sternal edge, and (3) the anterior intercostal branch which courses laterally. They exit according to the number of the rib. These are the ones which must be dissected in branch trimming. Additionally, one or two branches (thymic branch and rami mediastinales) which course to the mediastinum at the upper ITA (near the first rib and first intercostal space), except the branches which supply the thoracic wall, should be dissected carefully. A relatively thick branch, which is divided superiorly and laterally from the first rib, can sometimes be seen. Trimming this branch allows the course of the ITA to be more linear, and this contributes to the extension of the effective length.
14.1.3 Internal Thoracic Artery Conventional Harvest Technique
A median sternotomy was performed. After dissecting the reflection of the mediastinal pleura from the endothoracic fascia, the ITA and both satellite veins were visualized. The endothoracic fascia was longitudinally incised several millimeters medial to one of the satellite veins using electrocautery. The incision extended along the most of the length of the vessel down to the sixth intercostal space. Retraction of the pedicle visualizes the accompanying vessels and the ITA itself. With the pedicle gently retracted downward and with gentle blunt dissection, the perforating and anterior intercostal arteries are occluded with small metal clips and divided with electrocautery close to the chest wall to avoid damaging the ITA. The pedicle is dissected up to the level of the second or first rib. With variable relation of phrenic nerve with ITA, careful dissection is needed on either side to avoid phrenic nerve injury causing paralysis of the diaphragm which results in delayed postoperative recovery. All the branches of ITA must be clipped to ensure a long-term patency. Inadequate harvest of ITA can result in steal of blood.
14.1.4 Skeletonization of the Internal Thoracic Artery with an Ultrasonic Scalpel
The right and left internal thoracic arteries possess suitable properties (quality and diameter) for grafting. Long-term graft patency of the bilateral ITA is also better. However, the conventional pedicle harvesting of bilateral ITA is now applied less commonly because of concerns about not only the length and blood flow but also the development of mediastinitis caused by a decline in blood flow to the sternum.
In contrast, ultrasonic complete skeletonization (UCS), the procedure invented by the author in 1998, [1–3] is a useful and safe graft harvest technique which alters our view on the use of ITA. The UCS can make in situ grafting using bilateral ITA easier (Fig. 14.2). In this section, the essence on ITA harvesting by UCS is described in detail.
Fig. 14.2
Ultrasonic complete skeletonization of the internal thoracic artery
Prior to harvesting, the endothoracic fascia is exposed by dissecting the pleura from the dorsum of the sternum. The endothoracic fascia around the third rib, approximately one centimeter near the median from the course of the ITA, is incised. An endothoracic fascia incision must be made near the median (in an upside visual field) from the internal thoracic vein, which travels with the ITA. It prevents not only unnecessary venous injury but also the knack of effective ITA dissection (Fig. 14.3). The internal thoracic vein can be visualized by a quick touch of the loose adipose and connective tissues with an ultrasonic scalpel (Harmonic Scalpel DH105; Ethicon). “Quick touch” is named for the safe and quick removal procedure of the tissues surrounding the ITA by using a cavitation phenomenon that an ultrasonic scalpel creates. The key points to use the “Quick touch” are as follows: within 0.2 s. of ITA contact time and no several contacts of the same area. When the internal thoracic vein can be clearly and proximally visualized, it should be pulled away to the superior visual field by using the Quick touch. In harvesting of the ITA, it is important for the UCS to separate the vein from the beginning of the procedure and not to cause bleeding.
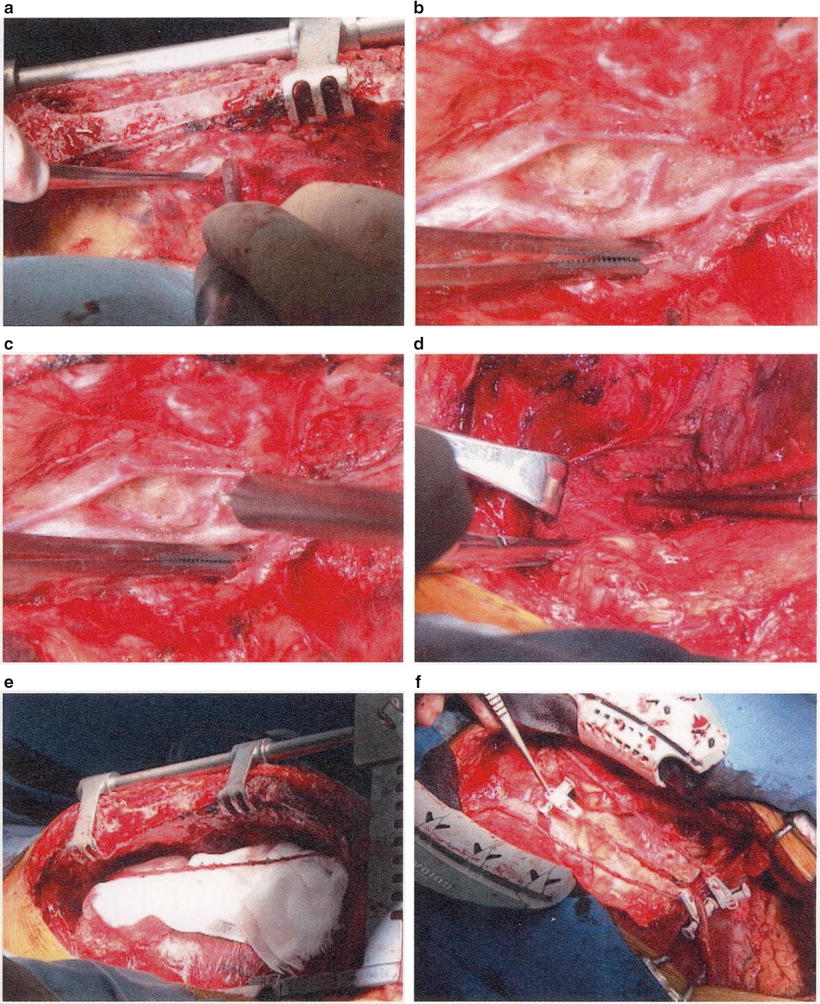
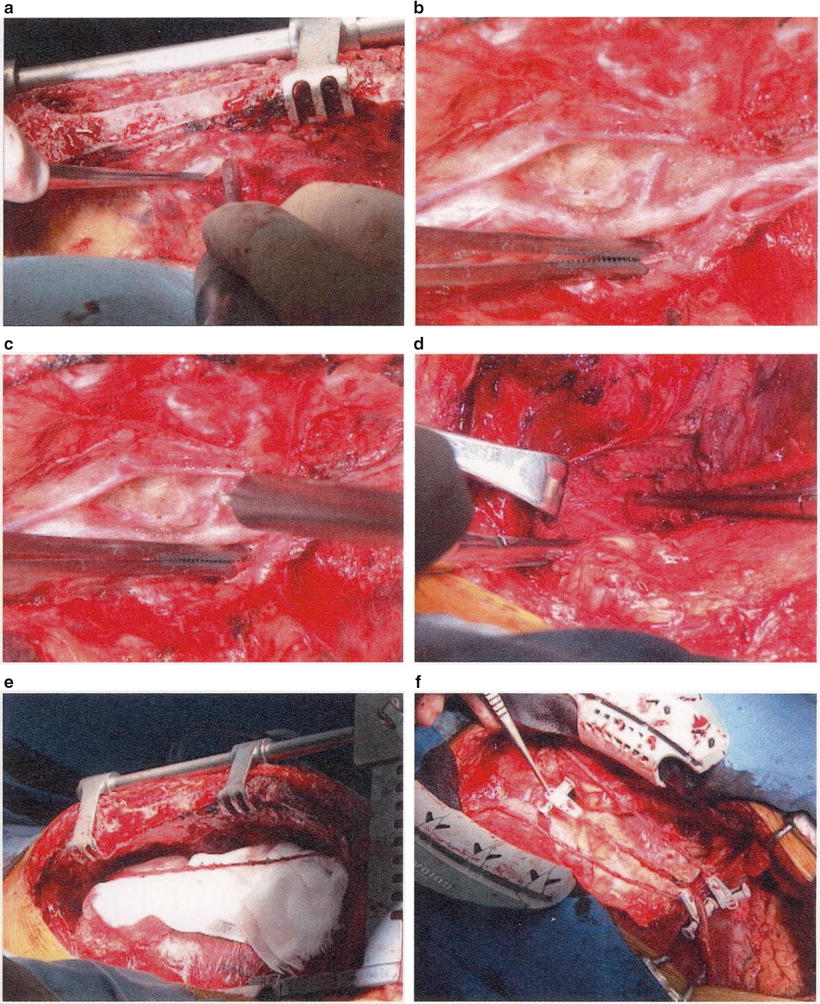
Fig. 14.3
Intraoperative view of ultrasonic complete skeletonization of the internal thoracic artery
The basics of ITA exposure are as follows. First is to use the “Quick touch” technique only to the superior region of the visualized ITA. Next is to leave untouched the area inferior to the ITA, that is, the margin connected to the endothoracic fascia. Final point is to rotate the ITA toward and inferiorly by pulling down the fascia. In branch dissection, start with the “Melting cut” of the sternal branch, which is visualized frontally, by grasping the endothoracic fascia with forceps using the left hand and pulling it toward and inferiorly. “Melting cut” is named for the procedure of protein coagulation of the branches by the Harmonic Scalpel. First, it is crucial to keep the probe tip of the Harmonic Scalpel 1 mm away from the main trunk and make a three-dimensional right angle, that is, to square up the main trunk, branch, and probe. Next, rotate the ITA proximally at an angle of 90° by pulling the endothoracic fascia inferior distally. Use the “Melting cut” procedure to the perforating branch visualized in front. Furthermore, rotate the artery at an angle of 90° to use the “Melting cut” procedure to the “anterior-coastal branch” in the frontal visual field. Finally, detach the ITA from the endothoracic fascia. Complete skeletonization of the region is done. In many cases, it is adequate that the distal end of the ITA is stripped up to the bifurcation of the superior epigastric artery and musculophrenic artery. The ITA of distal bifurcation has clearly different macroscopical and histological characteristics. Thus, it is not suitable as a regular graft.
In the proximal side, particularly in the proximal part of first to second intercostal spaces where the endothoracic fascia becomes unclear, harvesting is slightly different. First, the ITA is stripped bluntly using Tuppels by pushing it up from the pleural side to the sternal side, and then the course of the ITA is confirmed. After trimming the branches toward the mediastinal side, the branches toward the thoracic wall are trimmed with the Melting cut by rotating the ITA from the proximal visual field to the mediastinal side. Finally, the phrenic nerve is confirmed and stripped up to the site of the intersection with the ITA. At this time, it is crucial to use an ultrasonic scalpel from the viewpoint of avoiding injury to the phrenic nerve after visualizing the courses of the ITA and phrenic nerve.
After dissection of the ITA, a gauze soaked in warm papaverine hydrochloride 10 % is applied on the stripped ITA. This can solve adequately the spasm caused by irritation from the pull or rotation with forceps during ITA harvesting. After systemic heparinization, the bifurcation of the last peripheral branch is dissected, and then free flow is confirmed. The final free flow of ITA is usually more than 100 ml/min. In the event that the free flow is less than 50 mL/min, ITA damage should be considered. The main causes of ITA damage are local hematoma because of branch-out, lumen pressure because of intimal dissection, and thermal damage to the media and adventitia from defect or failure of the Quick touch.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


