Grafts
I. HEMODIALYSIS GRAFTS
A. Anatomy
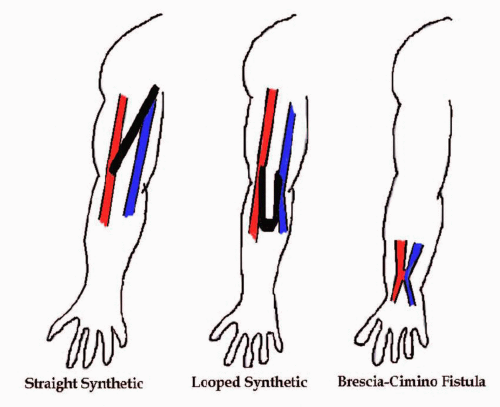
1. Dialysis grafts are placed in the arm to allow easy access for dialysis. The types are:
a. Brachial artery to axillary vein (most common)
b. Brachial artery to antecubital vein (next most common)
c. Radial artery to cephalic vein (Brescia-Cimino graft) (least common)
B. Pathology
The most common problem with dialysis grafts is that the venous anastomosis site or outflow vein becomes stenotic and thrombus forms due to the increased arterial pressure. Stenosis in the venous side of the graft happens in more than 80% of cases (Figs. 4.3 and 4.4). This can produce endothelial damage or intimal hyperplasia. Other problems with dialysis grafts include pseudoaneurysms developing at the dialysis site (Figs. 4.5 and 4.6); the possibility of the arterial anastomosis becoming stenotic; or hematomas developing since the graft is frequently pierced. If the arterial flow is greater than 400 cm/s, then the graft most likely has a 75% diameter reduction. Due to the increased venous return from the dialysis graft, congestive heart failure can develop.
C. History: Questions to Ask the Patient
Feel for a “thrill” (vibration) and listen for a bruit over the graft. This is a normal finding for a patent dialysis graft, but can also be produced by a graft stenosis. Ask:
1. Are you having any pain in your arm over the graft?
2. Are you having problems with your dialysis access?
3. Has the “thrill” in your graft disappeared?
D. Diagnostic Examination
1. Begin with the patient in a supine position with the head and torso slightly raised. Bring the arm out laterally away from the patient’s body with the palm facing up.
2. Using a 7.0- or 10.0-MHz linear-array transducer, follow the graft from each native vessel and anastomosis site. Most grafts are fairly easy to scan, as they are usually quite superficial.
3. Obtain color images and Doppler signals with peak systolic velocity measurements of the following areas:
a. Native artery
b. Arterial anastomosis
c. Arterial end of graft
d. Midgraft
e. Venous end of graft
f. Venous anastomosis
g. Native vein
E. Diagnostic Analysis
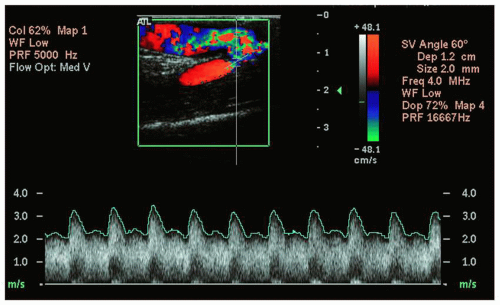
1. Peak systolic velocities in well-functioning dialysis grafts are typically between 100 and 200 cm/s. The velocity tends to be higher in the first 6 months after the placement of the graft (Fig. 4.2).
2. High-grade stenosis is probably present with a velocity elevation of 100% (velocity ratios of 2 or greater).
3. High-grade stenosis is also consistent with velocities of 50 cm/s or less.
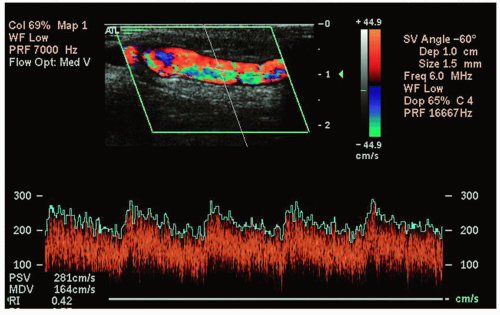 FIGURE 4.2. Doppler tracing of a normal dialysis graft within the first 6 months of placement. (Image courtesy of Philips Medical Systems.) |
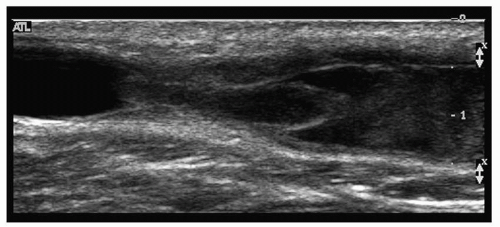 FIGURE 4.4. Gray-scale image of a thrombosed dialysis graft. (Image courtesy of Philips Medical Systems.) |
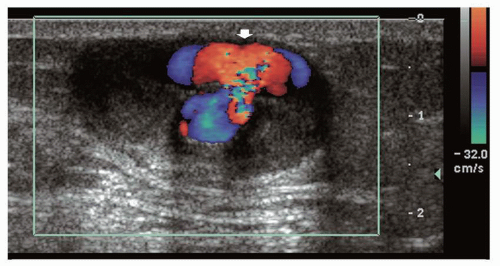 FIGURE 4.5. Color flow image of a dialysis graft with a pseudoaneurysm (arrow). (Image courtesy of Philips Medical Systems.) |
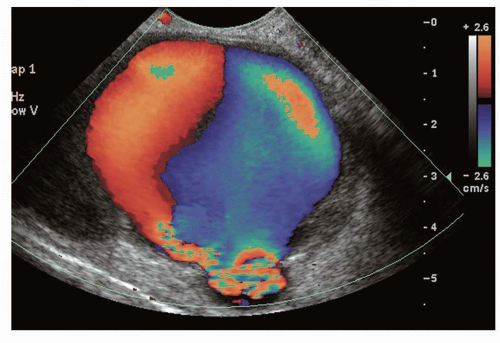 FIGURE 4.6. Color flow image of a dialysis graft with a large pseudoaneurysm. (Image courtesy of Philips Medical Systems.) |
II. BYPASS GRAFTS
A. Anatomy
1. When arterial disease is extremely severe, only surgical intervention can save the limb.
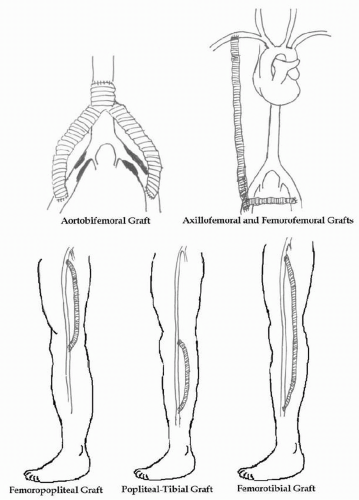
2. Types of arterial bypass grafts (Fig. 4.7):
a. Aorto-bifemoral
b. Aortofemoral
c. Femoropopliteal
d. Axillofemoral
e. Axillofemoral/femorofemoral
f. Femorotibial
g. Femorofemoral
3. What grafts are made of:
a. Synthetic grafts (Gore-Tex) (Fig. 4.8)
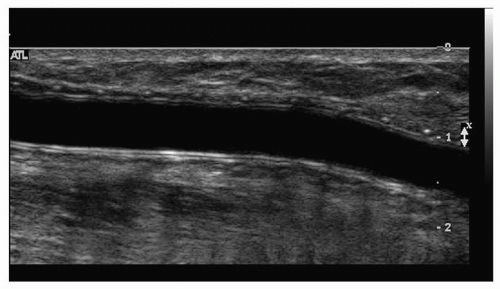
b. Synthetic grafts (Dacron)—generally used if the bypass graft involves the aorta. It has a corregated outline on ultrasound and is more echogenic than Gore-Tex (Fig. 4.9).
c. Autologous vein grafts:
(1) Reversed vein grafts (or harvesting vein graft). After surgical removal of the saphenous vein and ligation of all its branches, the vein is reversed and anastomosed to the artery. The small end of the vein is connected to the proximal segment of the artery, and the larger end of the vein is connected to the distal end of the artery. The venous valves are not disrupted because the arterial flow forces them to stay open. This must be mapped before surgery.
(2) In situ vein grafts. The greater saphenous vein is left in place with the proximal and distal ends anastomosed to the artery. The valves of the saphenous vein are surgically removed with a valvotome and the branches are ligated (Fig. 4.10).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree