Fig. 10.1
Massive hematemesis, complication of a pancreatic adenocarcinoma. Upper endoscopy showed an active bleeding of the second duodenum: an arteriography has been performed in emergency. (a) Aortography: modal anatomical arterial pattern of the splanchnic arteries; no evident blush. (b) Selective catheterization of the CT and then of the common hepatic artery. The injection near the ostium of the gastroduodenal artery shows a massive extravasation in the second duodenum, meaning a severe arterial erosion. (c) Control opacification after coils occlusion of the gastroduodenal A, just upstream of the extravasation. (d) Injection of the SMA to verify that there is not any “back door” reinjection via the duodeno-pancreatic arcades
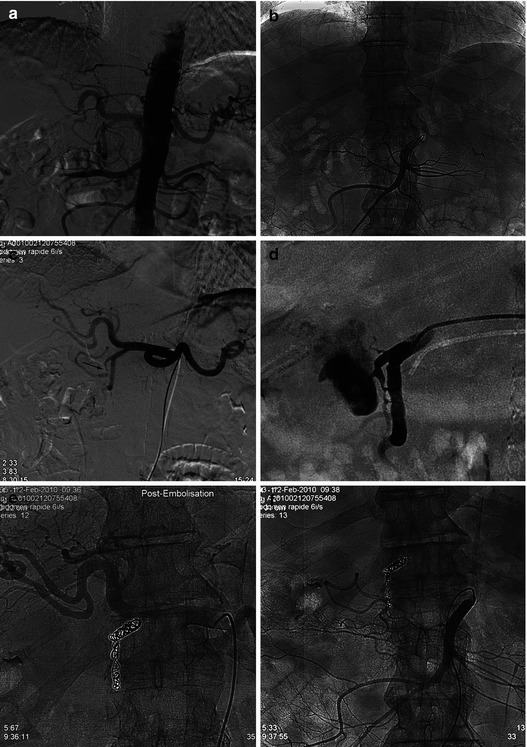
Fig. 10.2
78 years old M, GI tract hemorrhage considered as the consequence of a duodenal bulb ulcer. Hemodynamic shock and general status led in emergency to an arteriography, in order to embolize if possible an arterial bleeding. (a) Aortography: normal anatomy of the splanchnic arteries; diffuse atheroma. (b) Selective injection of the SMA: no extravasation. (c) Selective injection of the CT: note the variation of diameter of the superior and posterior duodeno-pancreatic arcades (arrow). (d) Hyperselective gastroduodenal A injection: massive duodenal extravasation from the previous noted abnormal segment, corresponding to an arterial erosion by the bulbar ulcer. (e) CT control opacification after coils exclusion of this abnormal artery and of the upstream gastroduodenal artery. (f) Last SMA control injection to be sure of no “back door” reinjection
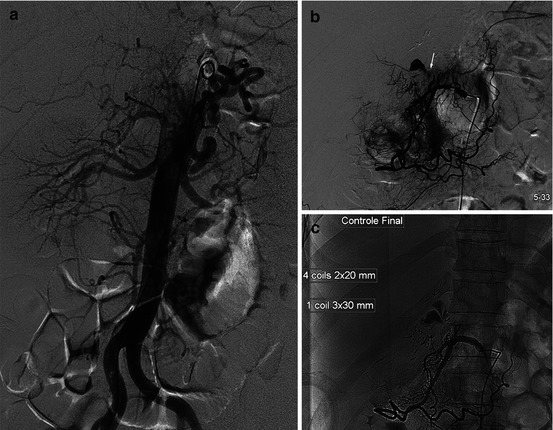
Fig. 10.3
Immediate follow-up after an hepatic segmentectomy with a bilio-digestive anastomosis to treat an ischemic choledochal stenosis, 3 years after a left hepatectomy (metastasis resection). Fibroscopies didn’t conclude to precise the site of a low flow bleeding. (a) Aortography: sinuous splenic artery; not any hypervascularization or blush. (b) Selective common hepatic A injection: initial variation of the lumen diameter (black arrow): spasm, irregular thin segment (white arrow), and extravasation from the duodeno-pancreatic arcade. (c) Control angio after exclusion by coils
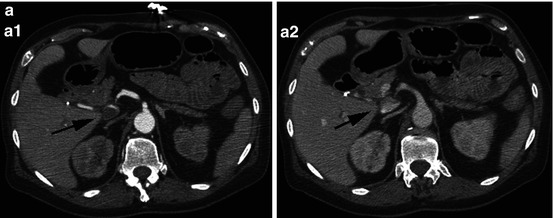
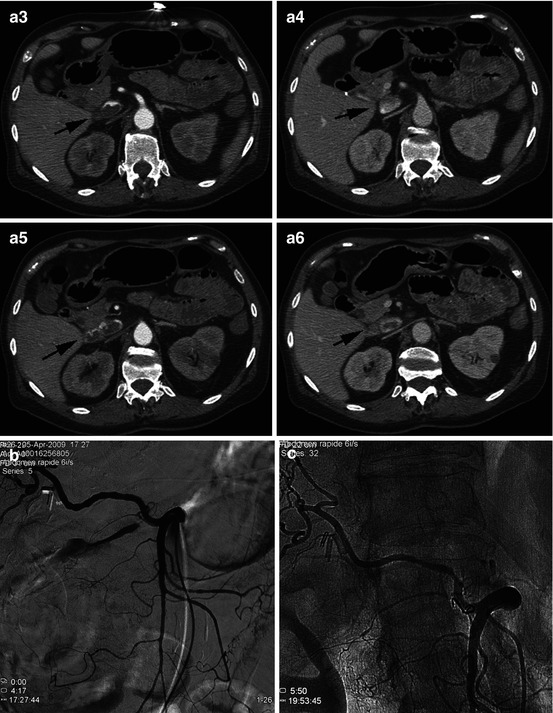
Fig. 10.4
71 years old M, chronic lymphoid leukemia, upper and lower GI tract bleeding. (a) Blush at the level of the dilated third duodenum; note the collapsed vena cava. (b) Massive bleeding from a thin proximal branch of the right hepatic A, collateral of the SMA. (c) Control angio after exclusion by coils
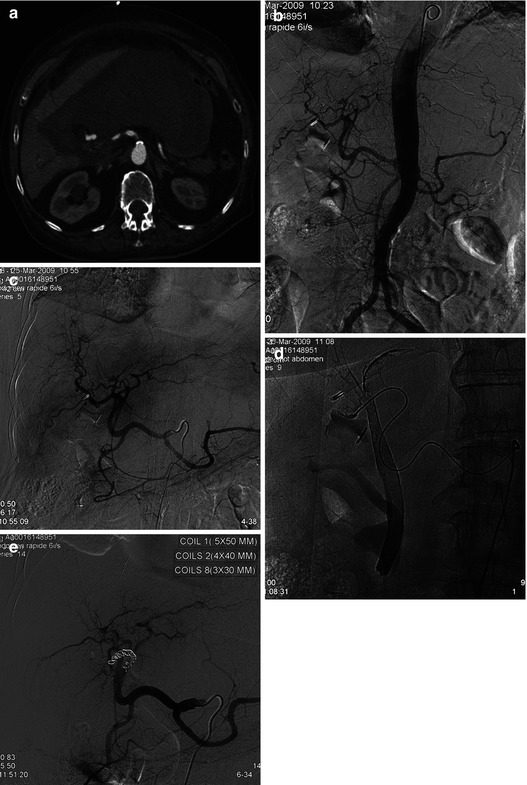
Fig. 10.5




78 years old, cholecystectomy, and then surgical redux at D7 because of a gallbladder space hematoma. But the day after, hemorrhagic shock again. (a) CT in emergency: very large gallbladder space hematoma. (b) Aortography: normal arterial anatomy; stretching of the splenic artery, consequence of this voluminous hematoma; diffuse atheroma. (c) Selective injection of the CT: note a variation of the right hepatic A lumen (arrow). (d) Right hepatic artery injection: opacification of the biliary duct, consequence of an arterio-biliary fistula. (e) Coils upstream of the arterial lesion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


