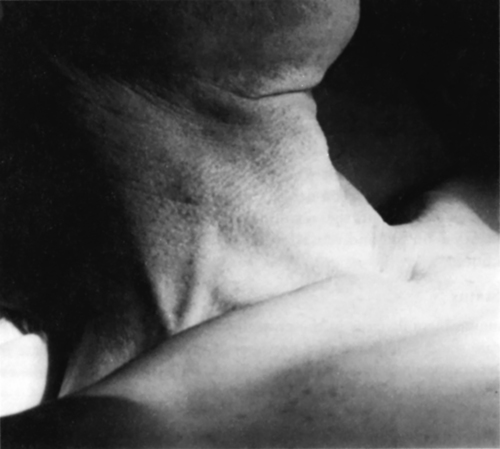
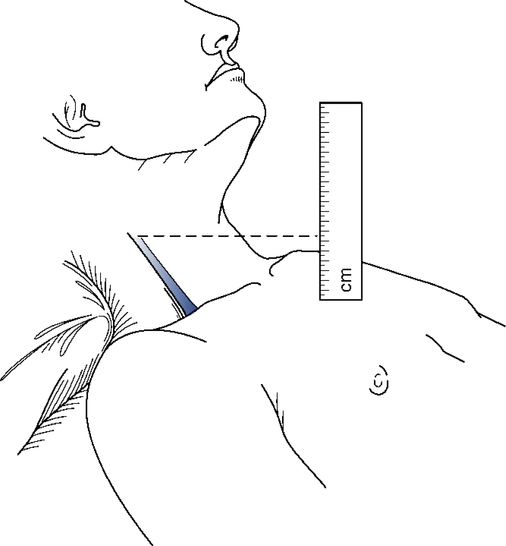
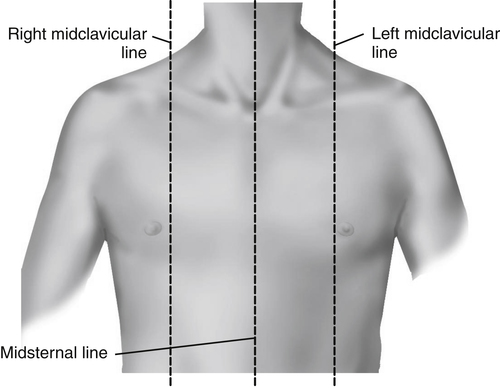
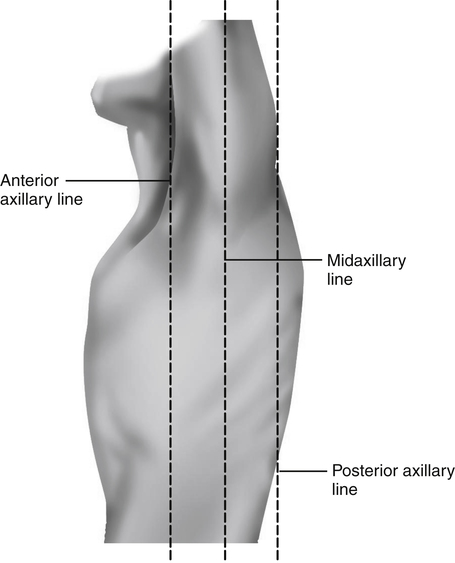
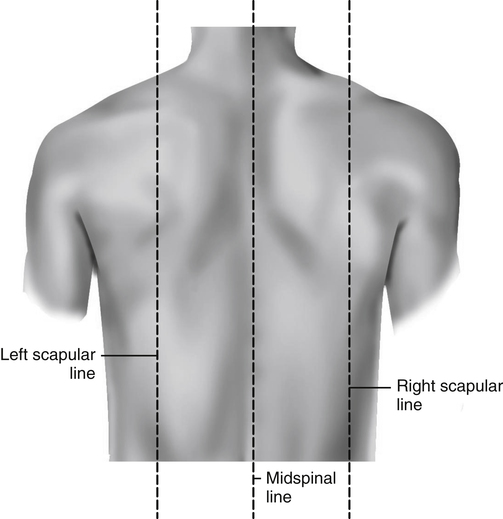
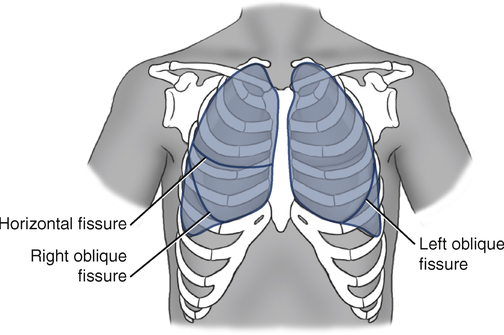
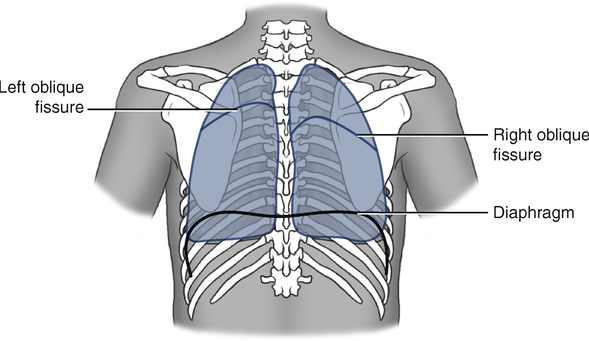
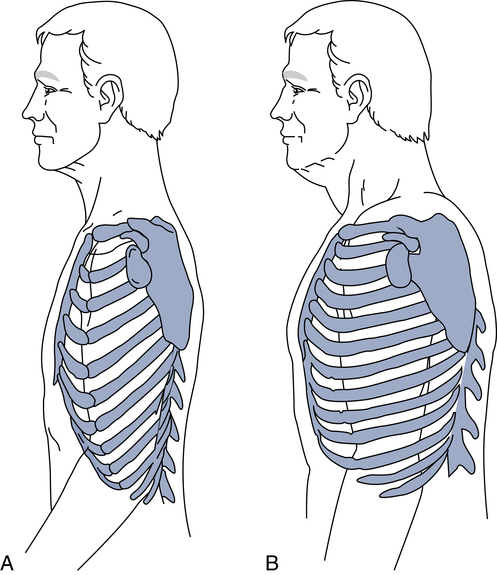
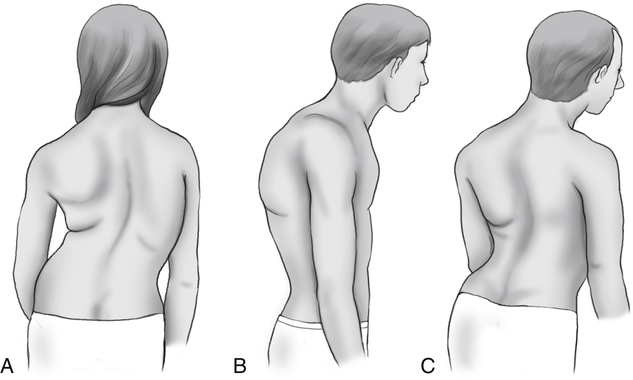
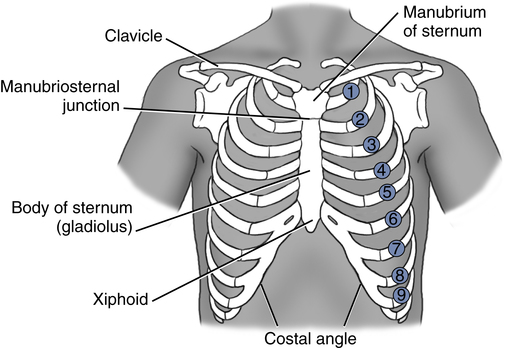
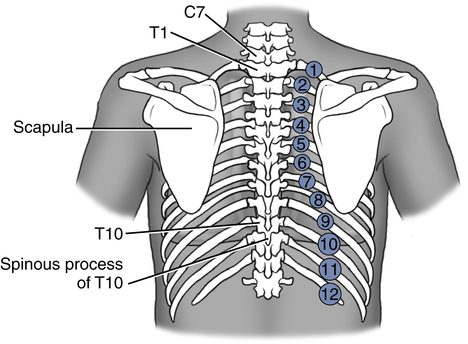
After reading this chapter, you will be able to: 1. Describe the four components of the physical examination. 2. Explain the importance of reviewing the history of present illness before performing a physical examination. 3. Describe the significance of the following during examination of the head and neck: e. Changes in pupillary size in response to light 4. Identify the correct method for measuring jugular venous pressure and expected normal findings. 5. Locate the topographic position of the following: a. Thoracic cage landmarks (suprasternal notch, sternal angle [angle of Louis], vertebral spinous processes [C7 and T1]) b. Lung fissures (oblique [major] and horizontal [minor]) c. Tracheal bifurcation anteriorly and posteriorly d. Right and left diaphragm anteriorly and posteriorly 6. Define the following terms used to classify thoracic configuration during inspection of the chest: 7. Define the following terms used to describe breathing pattern during inspection of the chest: 8. Describe the breathing patterns associated with restrictive and obstructive lung disease. 9. Identify the muscles of inspiration. 10. Describe the clinical significance of accessory muscle use and retractions and bulging. 11. Define the following terms and state their significance: 12. Describe the clinical significance of peripheral versus central cyanosis. 13. List causes of increased and decreased tactile fremitus. 14. List causes of decreased thoracic expansion as assessed during chest palpation. 15. Describe subcutaneous emphysema and its clinical significance. 16. List causes of increased and decreased resonance during percussion of the lung. 17. Identify the four basic parts of a stethoscope and their uses. 18. Describe the proper technique for auscultation of the lungs. 19. Identify the four characteristics of breath sounds that should be evaluated during auscultation. 20. Define the following terms used to describe lung sounds and the mechanisms responsible for producing the sounds: 21. Define the following terms used to describe abnormal lung sounds and the mechanisms responsible for producing the sounds: 22. Use qualifying adjectives to describe lung sounds and explain the importance of using these qualifying adjectives. 23. Describe the significance of the following auscultatory findings: g. Inspiratory and expiratory crackles 24. Define bronchophony and its cause. 25. Identify the topographic location of the apex and base of the heart during examination of the precordium. 26. Identify the point of maximal impulse, its normal location, and the factors that may cause it to shift to the right or left. 27. Describe the best location for auscultating sounds produced by the aortic, pulmonic, mitral, and tricuspid valves. 28. Describe what produces the first (S1) and second (S2) heart sounds, which are normal, as well as the third (S3) and fourth (S4) heart sounds, which are typically not normal. 29. Describe what is meant by a gallop rhythm and what it signifies. 30. List the factors that increase or decrease the intensity of the heart sounds. 31. Describe the clinical significance of a loud P2 heard during auscultation of the heart. 32. Describe the factors that cause systolic and diastolic heart murmurs. 33. Define the term hepatomegaly and its significance in the cardiopulmonary patient. 34. Define the following terms and their significance during examination of the extremities: This chapter emphasizes the techniques of examination used in assessment of the patient with cardiopulmonary disease. Because cardiopulmonary disease may indirectly alter other body systems, examination of the whole patient is important. The techniques used in examination of the thorax and other body systems for the abnormalities often associated with respiratory disease are reviewed. The typical order in which the initial physical examination is performed and recorded is presented in Box 5-1. See Chapter 4 for a complete discussion of the initial impression and assessment of the vital signs. The pupillary reflexes are evaluated as part of the neurologic examination. Cranial nerves II and III must be intact for normal pupillary reflexes to be present. If the pupils are equal in size, round, and reactive to light and accommodation, the physician may simply write PERRLA (pupils equal, round, reactive to light and accommodation) in the patient’s chart. Head trauma, tumors, central nervous system disease, and certain medications can cause abnormal findings. Brain death, catecholamines, and atropine can cause the pupils to become dilated and fixed (mydriasis). Atropine is a common medication used during cardiopulmonary resuscitation, and its administration minimizes the use of assessing pupillary reflexes as a measure of the patient’s neurologic status. Parasympathetic stimulants and opiates can cause pinpoint pupils (miosis). Examination of the pupillary reflexes is also discussed in Chapter 6. In the supine position, the neck veins of a healthy person are full. When the head of the bed is elevated gradually to a 45-degree angle from horizontal, the level of the column of blood descends to a point no more than a few centimeters above the clavicle with normal venous pressure. With elevated venous pressure, the neck veins may be distended as high as the angle of the jaw, even when the patient is sitting upright (Fig. 5-1). The degree of venous distention can be estimated by measuring the distance the veins are distended above the sternal angle. The sternal angle has been chosen universally because its distance above the right atrium remains nearly constant (approximately 5 cm) in all positions. With the head of the bed elevated to a 45-degree angle, venous distention greater than 3 to 4 cm above the sternal angle is abnormal (Fig. 5-2). The strength of the pulse at any location is described on a scale of 0 to 4, as follows: On the anterior chest, the midsternal line divides the chest into two equal halves. The left and right midclavicular lines parallel the midsternal line and are drawn through the midpoints of the left and right clavicles, respectively (Fig. 5-3). The midaxillary line divides the lateral chest into two equal halves. The anterior axillary line parallels the midaxillary line and is situated along the anterolateral chest. The posterior axillary line is also parallel to the midaxillary line and is located in the posterolateral chest (Fig. 5-4). Three imaginary vertical lines are drawn on the posterior chest. The midspinal line divides the posterior chest into two equal halves. The left and right midscapular lines parallel the midspinal line and pass through the inferior angles of the scapulae in the relaxed upright patient (Fig. 5-5). On the anterior chest, the suprasternal notch is located at the top of the manubrium and can be located by palpation of the depression at the base of the neck. Directly below this notch is the sternal angle, which is also called the angle of Louis. The sternal angle can be identified by palpating down from the suprasternal notch until the ridge between the gladiolus and the manubrium is identified. This important landmark is visible in most persons. The second rib articulates with the top of the gladiolus at this point (Fig. 5-6). Rib identification on the anterior chest can now be accomplished with this as a reference point. It is recommended that ribs be counted to the side of the sternum because individual costal cartilages that attach the ribs to the sternum are not identified as easily near the sternum. On the posterior chest, the spinous processes of the vertebrae are useful landmarks (Fig. 5-7). The spinous process of the seventh cervical vertebra (C7) usually can be identified by having the patient extend the head and neck forward and slightly down. At the base of the neck, the most prominent spinous process that can be visualized and palpated is C7. The spinous process just below C7 belongs to the first thoracic vertebra (T1). The scapular borders also can be useful landmarks on the posterior chest. With the patient’s arms raised above the head, the inferior border of the scapula lies almost directly over the oblique fissure that separates the upper from the lower lobes on the posterior chest. Between the lobes of the lungs are the interlobar fissures. Both lungs have an oblique fissure that begins on the anterior chest at approximately the sixth rib at the midclavicular line. This fissure extends laterally and upward until it crosses the fifth rib on the lateral chest in the midaxillary line and continues on the posterior chest to approximately T3 (Figs. 5-8 and 5-9). Superiorly on the anterior chest, the lungs extend 2 to 4 cm above the medial third of the clavicles. The inferior borders on the anterior chest extend to approximately the sixth rib at the midclavicular line and to the eighth rib on the lateral chest wall. On the posterior chest, the superior border extends to T1, and the inferior border varies with ventilation between approximately T9 and T12 (see Fig. 5-9). The normal adult thorax has an anteroposterior diameter less than the transverse (side-to-side) diameter. The anteroposterior diameter normally increases gradually with age and prematurely increases in patients with COPD. This abnormal increase in anteroposterior diameter is called a barrel chest and is commonly seen in patients with emphysema due to hypertrophy of the accessory muscles of breathing and chronic hyperinflation of the lungs. When the anteroposterior diameter increases, the ribs lose their normal 45-degree angle of slope in relation to the spine and become horizontal (Fig. 5-10). Other abnormalities of the thoracic configuration include the following: Pectus carinatum: outward sternal protrusion anteriorly Pectus excavatum: depression of part or all of the sternum Kyphosis: spinal deformity in which the spine has an abnormal anteroposterior curvature (Fig. 5-11) Scoliosis: spinal deformity in which the spine has a lateral curvature (see Fig. 5-11) Kyphoscoliosis: combination of kyphosis and scoliosis (see Fig. 5-11) The healthy adult at rest has a consistent rate and rhythm of ventilation. The diaphragm and the intercostal muscles are the primary muscles of ventilation, actively working to increase the thoracic cavity dimension during normal inspiratory effort. During normal breathing at rest, the diaphragm performs the majority of the work of breathing. The effort of breathing is minimum on inhalation and passive on exhalation. Men typically breathe with the diaphragm, causing the stomach to move slightly outward during inhalation. Women tend to use a combination of intercostal muscles and the diaphragm, producing more chest wall movement than men. Table 5-1 describes the abnormal patterns of breathing. See Chapter 4, Table 4-4 for further descriptions of terms commonly used to describe breathing rates associated with patterns of breathing. TABLE 5-1 Additional muscles of ventilation, called accessory muscles, are also slightly active during normal, resting breathing. When ventilatory demands increase, these accessory muscles become more active in assisting the primary muscles of ventilation in the work of breathing. The predominant accessory muscles include the intercostal, scalene, sternocleidomastoid, pectoral, trapezius, and abdominal wall muscles. The accessory muscles of inspiration specifically include the external intercostals, scalene, sternocleidomastoids, trapezius, pectoralis minor, and pectoralis major. Changes in the patient’s breathing pattern can provide important clues to the type of respiratory problem present. Patients with restrictive lung disease (reduced lung volumes) typically breathe with a rapid (tachypnea) and shallow (hypopnea) pattern (see Chapter 4, Table 4-4 for further discussion of breathing rate and pattern terminology). The more lung volume lost, the greater increase in the respiratory rate. Acute obstruction of intrathoracic airways, as occurs with asthma, results in a prolonged exhalation time. The approximate I:E ratio can be determined by timing the two phases of breathing. Normal I:E ratio is approximately 1:2. With more severe cases of airway obstruction, the I:E ratio may be 1:3, 1:4, or even longer at 1:5 or greater. Acute upper airway obstruction, as occurs with croup or epiglottitis, often results in a prolonged inspiratory time.
Fundamentals of Physical Examination
Examination of the Head and Neck
Head and Face
Eyes
Neck
Lung Topography
Imaginary Lines
Thoracic Cage Landmarks
Lung Fissures
Lung Borders
Examination of the Thorax
Inspection
Thoracic Configuration
Breathing Pattern and Effort
Pattern
Characteristics
Causes
Tachypnea
Rapid rate of breathing
Loss of lung volume, arterial hypoxemia, metabolic acidosis
Apnea
No breathing
Cardiac arrest
Biot
Irregular breathing with long periods of apnea
Increased intracranial pressure
Cheyne-Stokes
Irregular type of breathing; breaths increase and decrease in depth and rate with periods of apnea
Diseases of central nervous system, congestive heart failure
Kussmaul
Deep and fast
Metabolic acidosis
Apneustic
Prolonged inhalation
Brain damage
Paradoxical
Injured portion of chest wall area moves in the opposite direction to the rest of the chest
Chest trauma
Abdominal paradox
Contraction of accessory muscles to aid inspiratory effort; diaphragm is pulled upward and abdomen sinks inward during inspiration
Fatigue of diaphragm, paralysis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Fundamentals of Physical Examination