We aimed to determine late functional health status of the growing adult population with repaired tetralogy of Fallot (TOF). We studied all 840 patients with TOF born from 1927 through 1984 who survived to adulthood (>18 years of age). Clinical follow-up was by chart review, telephone interview (n = 706), and echocardiographic reports (n = 339). Functional health status was assessed using Short Form-36 (SF-36) surveys (n = 396) indexed to normative data. Risk of reoperation was low (≈1%/year) but increased beyond age 40 years. At latest follow-up moderate or severe pulmonary regurgitation was common (54%) and right ventricular outflow tract stenosis presented in 1/3. Consequently, evidence of right ventricular dilatation and dysfunction and tricuspid regurgitation was typical. Left-sided abnormalities were also common: hypertrophy (p <0.0001) and outflow tract dilation (p <0.0001) with at least mild aortic regurgitation in >50%. Cardiorespiratory symptoms were reported in 45% (palpitations 27%, dyspnea 21%, chest pain 17%). SF-36 scores were significantly below normal for 4 physical domains (p <0.001). Decrements in physical functioning were associated particularly with older age at follow-up (p <0.0001), associated syndromes/lesions, reoperations, ventricular dysfunction, tricuspid regurgitation, residual septal defects, and cardiorespiratory symptomatology. Echocardiographic abnormalities were more common in older patients (p <0.0001). All 3 SF-36 domains specific to psychosocial well-being were normal. In conclusion, despite excellent survival prospects, physical compromise is common in adults with repaired TOF. Greater decrements in older patients may reflect late deterioration with advancing age or cohort effects related to historical management. Efforts to limit ventricular and outflow tract dysfunction may translate into improved late functional status.
In the current era approximately 90% of infants born with tetralogy of Fallot (TOF) are expected to live beyond 40 years of age. In contrast, early operative mortality exceeded 25% in the early 1960s. Despite these dramatic decreases in childhood attrition, little is understood about the long-term functional outcomes for the burgeoning population of adults with repaired TOF. To understand the late functional health profile (and its modulators) of adults with repaired TOF, we investigated patients known to have survived to adulthood at our institution since records began in 1927. We used Short Form-36 (SF-36) functional health status surveys to quantify physical and psychosocial well-being and explored patient-specific features associated with functional health indexes.
Methods
In this study we investigated all patients known to have survived to adulthood (>18 years of age) at our institution with a diagnosis of TOF. The study was conceived in 2002; therefore, patients were eligible for inclusion if born before 1984. Patients were excluded if they died or were lost to follow-up before reaching 18 years of age. The study was undertaken with full institutional ethics board approval.
Extant patient charts recording a primary diagnosis of TOF range as far back as 1927 at our institution. Since that time, 1,693 children received a diagnosis of TOF during the study period (before a 1984 year of birth). Of these 1,693, corrective repair was undertaken in 1,181 and 840 patients are known to have survived to 18 years of age and are the focus of this investigation. In 37 patients corrective surgery was undertaken in adulthood (after undergoing childhood systemic pulmonary artery shunts) and these 37 are included. Follow-up was undertaken from 2002 through 2004 to a median age of 29.5 years (range 18 to 64.9). Medical charts were retrieved on all 840, from which morphologic, surgical, and clinical histories were abstracted. Medical charts were the only source of data in 134 patients (16%). The remaining 706 (84%) were successfully traced to their last known place of contact and participated in brief telephone interviews on clinical history and symptomatology. Additional participation in functional and clinical assessments was requested at this point. At the time of follow-up, 18% of the study cohort were not under routine follow-up with a cardiology department.
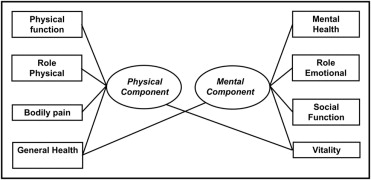
The SF-36 functional health survey is a multipurpose questionnaire involving 36 questions whose answers yield a profile of functional health and well-being. These resulting scores are categorized in 8 separate domains relating to individual aspects of physical functional health or otherwise psychosocial well-being ( Figure 1 ). The SF-36 functional health survey is a generic (rather than age- or disease-specific) tool and has been validated across populations and diseases. Normative data are available on 9,423 normal adult Canadians. Functional health assessment using the SF-36 health survey was successfully completed in 396 patients (47%). Scores were analyzed according to published guidelines. The domain score for each patient was then standardized to age- and gender-matched normal values and expressed as a z score.
Reports of echocardiograms were sought within 3 years of the point of last follow-up and were successfully obtained from patients’ follow-up institutions in 339 (40%). Original studies were not obtained and therefore functional and morphologic indexes were abstracted from the reports as described by the echocardiologist who performed the examination at a patient’s institution. Measurements of dimension were standardized and expressed as z scores based on published normative data. Qualitative variables were categorized as normal, mild, moderate, or severe as indicated by the report. Time-related parametric models were constructed using techniques incorporating multiple hazard domains. For analysis of surgical reoperation, competing risks censoring was used to account for patients who died before undergoing reoperation (and therefore are no longer “at risk”). Associations between patient-specific predictors and continuous dependent variables were explored using multiple linear regression. Variable selection for time-related regression and multiple linear regression was by automated forward stepwise techniques. Continuous variables were tested beforehand for possible transformations that improved linear calibration. Final variable selection for time-related outcomes and linear regression models was guided by bootstrap resampling (n = 1,000) as an indicator of reliability of the p value. Variables included in >50% resamples or clusters thereof were considered reliable. Statistical analysis was undertaken using SAS 9.0 (SAS Institute, Cary, North Carolina). Statistical significance was considered a p value ≤0.05.
Results
The present investigation relates to the 840 patients with TOF who are known to have survived to adulthood (>18 years of age). Baseline morphologic (at time of diagnosis), demographic, and clinical details are listed in Table 1 . Median age at corrective repair was 6.9 years and 58% had received a systemic pulmonary artery shunt. The actuarial likelihood of surviving to adulthood was 85 ± 1% of all 1,181 patients who underwent corrective surgery at our institution for TOF during the study period. Despite the high mortality associated with a historical repair of TOF, once adulthood was reached, long-term outcomes were good thereafter: only 68 of those surviving to adulthood have since died, a rate of attrition <1% per year such that ≈85% patients who reach adulthood were alive at 50 years of age (93 ± 1%, 88 ± 1%, and 83 ± 2% at 30, 40, and 50 years of age).
| Variable | No. | Missing | Frequency |
|---|---|---|---|
| Follow-up | |||
| Dead | 68 | 0 | 8 |
| Median survival from birth (years) | 29.5 | 0 | 18–64.9 |
| Telephone interview | 706 | 0 | 84 |
| Short Form-36 functional health questionnaire | 396 | 0 | 47 |
| Clinic consultation | 351 | 0 | 42 |
| Echocardiogram at latest follow-up | 339 | 0 | 40 |
| Noncardiovascular demographics | |||
| Men | 511 | 0 | 61 |
| Noncardiovascular syndrome | 105 | 4 | 13 |
| Down syndrome | 32 | 4 | 4 |
| DiGeorge syndrome | 22 | 4 | 26 |
| Developmental delay | 27 | 4 | 32 |
| Morphologic characteristics | |||
| “Classic” tetralogy of Fallot | 754 | 5 | 90 |
| Pulmonary atresia variant | 71 | 5 | 9 |
| Absent pulmonary valve variant | 10 | 5 | 1 |
| Atrial septal defect | 288 | 50 | 36 |
| Patent ductus arteriosus | 70 | 36 | 9 |
| Atrioseptal canal defect | 16 | 50 | 2 |
| Double-outlet right ventricle | 33 | 35 | 4 |
| Branch pulmonary artery hypoplasia | 166 | 82 | 22 |
| Discontinuous branch pulmonary arteries | 6 | 44 | 1 |
| Right aortic arch | 294 | 41 | 37 |
| Aberrant right subclavian artery | 17 | 39 | 2 |
| Major aortopulmonary collaterals | 54 | 62 | 7 |
| Anomalous coronary arteries | 61 | 62 | 8 |
| Left superior vena cava | 9 | 36 | 1 |
| Initial management | |||
| Median age at palliative surgery (years) | 1.94 | 24 | 1 d–19.4 yr |
| Systemic pulmonary artery shunt | 484 | 0 | 58 |
| Blalock-Taussig/modified Blalock-Taussig shunt | 409 | 3 | 85 |
| Waterston shunt | 58 | 3 | 12 |
| Potts shunt | 14 | 3 | 3 |
| Corrective surgery | |||
| Median age at corrective surgery (years) | 6.9 | 55 | 2 wk–55.6 yr |
| “No-patch” repair | 204 | 106 | 28 |
| Transannular patch | 239 | 106 | 33 |
| Patch elsewhere to right ventricular outflow tract | 254 | 106 | 35 |
| Conduit implantation | 37 | 106 | 50 |
| Reoperations as adults | 122 | — | 19 |
| Pulmonary valve replacement | 82 | 5 | 70 |
| Pulmonary artery augmentation | 47 | 5 | 40 |
| Right ventricular outflow tract augmentation | 39 | 5 | 33 |
| Right ventricular outflow tract conduit replacement | 13 | 5 | 11 |
| Tricuspid valve repair/replacement | 24 | 5 | 21 |
| Aortic valve replacement | 6 | 5 | 5 |
| Antiarrhythmic surgery | 6 | 5 | 5 |
| Transcatheter interventions as adults | |||
| Transcatheter intervention | 199 | 43 | 25 |
| Pulmonary artery balloon dilatation | 23 | — | 12 |
| Pulmonary artery stent | 6 | — | 3 |
| Pacemaker implantation | 12 | — | 6 |
| Implantable defibrillator | 11 | — | 6 |
| Radiofrequency ablation | 11 | — | 6 |
Surgical reoperations during adulthood were performed in 122 of these patients ( Table 1 ). After reaching 18 years of age, freedom from reintervention was 90 ± 1%, 79 ± 2%, and 62 ± 4% at 30, 40, and 50 years of age ( Figure 2 ). This risk of undergoing reoperation was a low constant hazard until approximately 40 years of age when a late hazard become increasingly predominant. Operative details at time of original corrective surgery were most strongly associated with risk of reoperation as an adult: use of a conduit (p = 0.006) or a patch to the right ventricular outflow tract that was not transannular (p = 0.008) and longer cardiopulmonary bypass duration (p = 0.01). However, it is likely these operative variables are surrogates for the type and complexity of the underlying lesion. The only baseline morphologic feature independently associated with adult reoperation was the presence of a right aortic arch (p = 0.05), which was a risk factor only for the increasing late hazard phase. The clinical significance of a right aortic arch is obscure because its presence did not correlate with other morphologic variables.
Available echocardiographic reports revealed that at latest follow-up at least mild right ventricular outflow tract stenosis was present in 1/3 and moderate or severe regurgitation in >50% ( Table 2 ). Consequently, some degree of right ventricular dysfunction and dilatation was present in ≈75% and at least mild tricuspid regurgitation in 90% ( Table 2 ). Important abnormalities were also present in the systemic ventricular performance. Median left ventricular wall thickness was significantly increased (indicating hypertrophy) and the left ventricular cavity was smaller than normal during systole and diastole. Also of interest were the large indexed dimensions of the left ventricular outflow tract. Median diameter of the ascending aorta at the level of the sinus of Valsalva was 3 SDs above normal ( Table 2 ). Although moderate-severe aortic regurgitation was rare, mild regurgitation was present in 1/2. Overall, echocardiographic parameters indicated that patients frequently had residual right ventricular outflow tract stenosis and regurgitation, leading to right ventricular dysfunction and dilatation and tricuspid regurgitation. On the left side, ventricular hypertrophy was seen in combination with dilated, mildly regurgitant outflow tracts. These features were particularly prominent in older patients ( Table 3 ).
| Variable | None | Mild | At Least Moderate |
|---|---|---|---|
| Left ventricular dysfunction | 288 (85%) | 36 (11%) | 13 (4%) |
| Left ventricular dilatation | 324 (96%) | 12 (4%) | 2 (1%) |
| Right ventricular dysfunction | 98 (29%) | 172 (51%) | 67 (20%) |
| Right ventricular dilatation | 74 (22%) | 126 (37%) | 137 (40%) |
| Right ventricular aneurysmal dilatation | 270 (80%) | 41 (12%) | 26 (8%) |
| Pulmonary regurgitation | 67 (20%) | 87 (26%) | 183 (54%) |
| Right ventricular outflow tract stenosis | 326 (96%) | 7 (2%) | 4 (1%) |
| Pulmonary valvar stenosis | 215 (63%) | 97 (29%) | 25 (7%) |
| Conduit stenosis | 323 (95%) | 5 (1%) | 9 (3%) |
| Branch pulmonary artery stenosis | 306 (90%) | 25 (7%) | 6 (2%) |
| Tricuspid valve regurgitation | 18 (5%) | 279 (82%) | 40 (12%) |
| Aortic valve regurgitation | 163 (48%) | 169 (50%) | 5 (1%) |
| Aortic root dilatation | 273 (8%) | 61 (18%) | 3 (1%) |
| Residual ventricular septal defect | 304 (90%) | 28 (8%) | 5 (1%) |
| Residual atrial septal defect | 323 (95%) | 14 (4%) | 0 (0%) |
| Right atrial dilatation | 302 (89%) | 24 (7%) | 10 (3%) |
| Left atrial dilatation | 284 (84%) | 46 (14%) | 6 (2%) |
| Dimensions and Doppler Gradients | Median | Missing | Range | p Value |
|---|---|---|---|---|
| Pulmonary valve peak gradient (mm Hg) | 18 | 88 | 4–60 | — |
| Right ventricular peak systolic pressure (mm Hg) | 39 | 52 | 19–145 | — |
| Left ventricular end-diastolic dimension z score | −2.3 | 22 | −8.5 to +2.5 | <0.0001 |
| Left ventricular end-systolic dimension z score | −1.0 | 23 | −9.5 to +4.6 | <0.0001 |
| Left ventricular posterior wall thickness z score | +0.9 | 130 | −2.1 to +22 | <0.0001 |
| Aortic annulus diameter z score | +3.7 | 308 | −2.3 to +9.7 | <0.0001 |
| Sinus of Valsalva z score | +3.1 | 49 | −4.4 to +10.3 | <0.0001 |
| Sinotubular junction z score | +5.4 | 319 | 0 to +9.6 | <0.0001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


