The purpose of the present report was to determine the frequency of a congenitally bicuspid aortic valve in patients ≥80 years of age old with aortic stenosis (AS) severe enough to warrant aortic valve replacement. Transcatheter aortic valve implantation (TAVI) has traditionally been reserved for patients ≥80 years of age with severe AS involving a 3-cuspid aortic valve. Traditionally, AS involving a 2-cuspid aortic valve has been a contraindication to TAVI. We examined operatively excised stenotic aortic valves in 364 patients aged ≥80 years to determine the frequency of an underlying congenitally bicuspid aortic valve. Of the 347 octogenarians and 17 nonagenarians, 78 (22%) and 3 (18%) had stenotic congenitally bicuspid aortic valves, respectively. In conclusion, because the results of TAVI are less favorable in patients with stenotic congenitally bicuspid valves than in patients with stenotic tricuspid aortic valves, proper identification of the underlying aortic valve structure is important when considering TAVI as a therapeutic procedure for AS in older patients.
It is generally believed that older patients with isolated aortic stenosis (AS) (with or without aortic regurgitation [AR]) infrequently have congenitally bicuspid aortic valves, the presence of which has been considered in most institutions to be a contraindication for transcatheter aortic valve implantation (TAVI) without replacement. Most patients undergoing TAVI are ≥80 years of age, and most, of course, do not have a bicuspid aortic valve. Our purpose was to describe the frequency of congenitally bicuspid aortic valves in patients ≥80 years of age having had aortic valve replacement (AVR) for AS at Baylor University Medical Center (BUMC), Dallas, in the past 2 decades and to examine their survival in relation to valve structure.
Methods
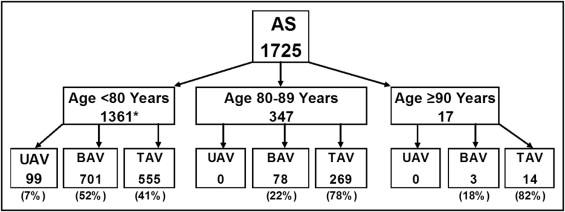
From March 2, 1993 to July 8, 2011, a total of 1,725 operatively excised native stenotic aortic valves (with or without AR) in patients aged >20 years having isolated AVR (with or without coronary artery bypass grafting [CABG]) were received in the surgical pathology department at BUMC. The excised valve was weighed beginning in 1998. Its structure in all cases was determined by one of us (W.C.R.) during the week that the valve was excised. Of the 1,725 patients, 364 (21%) were ≥80 years of age at the time of AVR. These 364 patients were the subject of the present report ( Figure 1 ) . Any patient undergoing replacement of a cardiac valve other than the aortic valve, any patient with previous aortic valvulotomy or replacement, and any patient with mitral stenosis were excluded from the study. The AVR in the patients included was their first cardiac operation.
That the patients had AS (with or without AR) was confirmed by examination of their preoperative cardiac catheterization and/or echocardiographic reports, which were available from the Baylor Physician Portal, BUMC electronic medical records, and/or the cardiovascular computer database (Apollo Advance C/S, version 4.2.13, LUMEDX, Oakland, California). The patients were considered to have AS if the peak systolic transvalvular gradient was >10 mm Hg. The aortic valve gradients and valve areas were obtained from the cardiac catheterization reports.
Cardiac catheterization data were available to us in most patients: peak transvalvular pressure gradients in 198 patients (57%), mean transvalvular pressure gradients for 193 (56%), aortic valve areas in 204 patients (59%), and left ventricular ejection fractions in 100 patients (29%). Most patients in whom cardiac catheterization data were not available were referred directly to a cardiovascular surgeon. The patients without cardiac catheterization data available to us underwent coronary angiographic studies before being referred to BUMC; however, the results of these studies were not available to us.
The mean ± standard deviation and percentages were calculated to describe the study cohort. The hazard ratios and 95% confidence intervals were estimated to describe survival. Kaplan-Meier plots were used to describe the unadjusted survival in patients with bicuspid valve disease—versus—tricuspid valve disease. A Cox proportional hazards model was used to assess the adjusted association between undergoing concomitant bicuspid valve disease (vs tricuspid valve disease) and survival. The model was adjusted by age, gender, and concomitant CABG. Restricted cubic splines were used for age. Possible effect modification by gender and age was investigated and ruled out. The Grambsch and Therneau test statistic was used to test for proportionality of hazards in the Cox model. Statistical analyses were performed using SAS, version 9.2 (SAS Institute, Cary, North Carolina) and R software, version 2.13.0.
Results
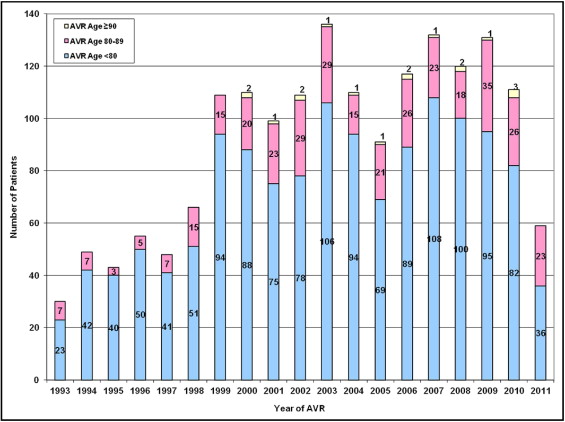
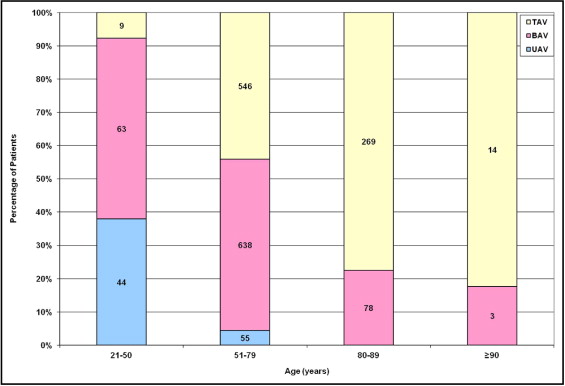
The frequency of AVR for AS with or without AR in the octogenarians and nonagenarians among the 1,725 patients during each year of the study years (1993 to 2011) is displayed in Figure 2 . The frequency of aortic valve structure stratified by 3 age groups is displayed in Figures 2 and 3 and stratified by 4 age groups in all 1,725 patients is displayed in Figure 3 . Of the 116 patients aged 21 to 50 years, 107 (92%) had either a congenitally unicuspid or bicuspid aortic valve. Of the 1,245 patients aged 51 to 79 years, 693 (56%) had a congenitally malformed valve (unicuspid in 55 and bicuspid in 638). Of the 364 octogenarians and nonagenarians, none had a unicuspid valve. Of the 347 octogenarians, 78 (22%) had bicuspid valves, and of the 17 nonagenarians, 3 (18%) had a bicuspid aortic valve ( Figure 3 ).
The characteristics of the 347 octogenarians and 17 nonagenarians are listed in Table 1 . Concomitant CABG was performed in 208 (60%) of the 347 octogenarians. Of the 347 octogenarians, survival data were available for 340. A total of 133 (39%) died either during the operation or during follow-up (≤14 years after AVR). The interval from AVR to death ranged from 0 to 14 years (median 4.3). Of these 347 octogenarians, 78 patients (22%) had bicuspid aortic valves and 269 (78%) had tricuspid aortic valves; 150 (43%) were women and 197 (57%) were men. The operatively excised bicuspid aortic valves in the men weighed from 0.81 to 7.84 g (mean 3.61), and in the women, from 0.79 to 4.90 g (mean 2.62). The operatively excised tricuspid aortic valves in the men ranged from 1.00 to 6.60 g (mean 2.31), and in the women, from 0.45 to 6.40 g (mean 1.64).
| Characteristic | Patients | Octogenarians | Nonagenarians |
|---|---|---|---|
| Total (n) | 364 | 347 | 17 |
| Mean age (years) | — | 83 | 91 |
| Men | 209 (57%) | 197 (57%) | 12 (71%) |
| Women | 155 (43%) | 150 (43%) | 5 (29%) |
| Bicuspid aortic valve | 81 (22%) | 78 (22%) | 3 (18%) |
| Weight (g) | |||
| Men | |||
| Range | 0.81–7.84 | 4.20, 5.73, 9.75 | |
| Mean | 3.61 | 6.56 | |
| Women | |||
| Range | 0.79–4.90 | — | |
| Mean | 2.62 | ||
| Tricuspid aortic valve | 283 (78%) | 269 (78%) | 14 (82%) |
| Weight (g) | |||
| Men | |||
| Range | 1.00–6.60 | 1.08–4.43 | |
| Mean | 2.31 | 2.30 | |
| Women | |||
| Range | 0.45–6.40 | 0.43–2.22 | |
| Mean | 1.64 | 1.27 | |
| Preoperative hemodynamics | |||
| Left ventricular peak systole (mm Hg) | 195 | ||
| Range | 96–266 | 95–237 | |
| Mean | 187 | 179 | |
| Left ventricular end diastole (mm Hg) | 193 | ||
| Range | 2–56 | 14–32 | |
| Mean | 22 | 22 | |
| Aorta peak systole (mm Hg) | 233 | ||
| Range | 75–200 | 64–168 | |
| Mean | 143 | 129 | |
| Aorta end diastole (mm Hg) | 233 | ||
| Range | 34–101 | 28–76 | |
| Mean | 62 | 54 | |
| Left ventricular aortic peak systolic gradient (mm Hg) | 205 | ||
| Range | 11–130 | 20–69 | |
| Mean | 47 | 49 | |
| Left ventricular aortic mean gradient (mm Hg) | 203 | ||
| Range | 9–89 | 25–57 | |
| Mean | 39 | 42 | |
| Aortic valve area (cm 2 ) | 214 | ||
| Range | 0.18–1.84 | 0.41–1.07 | |
| Mean | 0.73 | 0.66 | |
| Ejection fraction (%) | 96 | ||
| Range | 10–80 | 15–70 | |
| Mean | 51 | 39 | |
| Concomitant coronary bypass grafting | 221 (61%) | 208 (60%) | 13 (76%) |
| Hospital stay ⁎ (days) | 344 | ||
| Range | 3–38 | 4–25 | |
| Mean | 11.1 | 10.1 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


