Emerging evidence has shown the potential of marked improvement in left ventricular ejection fraction (LVEF) in patients with recent-onset cardiomyopathy (ROCM) on medical therapy. This study was designed to determine the frequency and to identify predictors of normalization of LVEF in a cohort of Chinese patients with ROCM receiving contemporary medication. A consecutive series of patients admitted from October 2008 to November 2012 with the clinical diagnosis of ROCM and LVEF ≤40% by echocardiography at presentation were followed up at least 12 months to identify those with normalization of LVEF, defined as an increase in LVEF to a final level of ≥50%. An array of clinical and echocardiographic variables regarded as potentially relevant to normalization was evaluated to identify predictors using logistic regression analysis. After a mean follow-up of 31 ± 13 months, 48% of 128 patients had normalized their LVEF, showing a significant increase in LVEF from 32 ± 6% to 58 ± 5%, of which 68% occurred within 1 year after initial diagnosis. Multivariate analysis demonstrated that normalization of LVEF was associated with a history of hypertension, higher systolic blood pressure at presentation, shorter electrocardiographic QRS duration, smaller left ventricular end-diastolic diameter, and higher LVEF by echocardiography at baseline. In conclusion, nearly 1/2 of a relatively large number of Chinese patients with ROCM have shown normalization of LVEF on current medical therapy after a medium-term follow-up, which was associated with some clinical and echocardiographic parameters.
Current medical therapy has led to remarkable improvements in the survival and control of symptoms in patients with dilated cardiomyopathy (DCM) over the past decades. Despite the increasing recognition that marked improvement in left ventricular systolic function, as reflected mainly by left ventricular ejection fraction (LVEF), is possible in some patients with DCM, neither the likelihood of normalization of LVEF nor the clinical variables associated with its occurrence in patients with recent-onset cardiomyopathy (ROCM), defined as <6 months of symptom duration, is well delineated because of smaller number of patients studied or shorter follow-up period in previous reports. Furthermore, data on the frequency of normalization of LVEF in Chinese patients with ROCM are lacking to date. Thus, the present study was designed to determine the frequency and to identify some predictors of normalization of LVEF in a relatively large number of Chinese patients with ROCM on contemporary medical therapy after a relatively long-term follow-up.
Methods
The registry of all adult patients (aged ≥18 years) referred for evaluation of heart failure at the Heart Failure Care Unit, Fuwai Hospital, from October 2008 to November 2012 was reviewed to identify ROCM. The diagnosis of DCM was made according to the recommendations on diagnosis and treatment of cardiomyopathy (China) in 2007. All patients had an LVEF of ≤40% by echocardiography and symptom duration of <6 months at presentation, in the absence of significant coronary artery disease, primary restrictive, or hypertrophic cardiomyopathy, primary valvular, or congenital heart disease. Patients on cardiac resynchronization therapy were excluded, because we focused on the effect of medication alone. Patients with known cardiomegaly for >6 months were not considered to have ROCM regardless of symptom duration. However, patients in whom a history of hypertension or alcohol use was documented in the medical records were included because in an individual patient it is often unclear whether these factors cause, exacerbate, or have no relation to the development of cardiomyopathy.
An array of clinical and echocardiographic variables regarded as potentially relevant to normalization of LVEF was evaluated on admission. Transthoracic echocardiography was performed in all patients at baseline, and LVEF was measured using the modified Simpson method. All patients were clinically followed up at least 12 months or until cardiac transplantation or death, at intervals of 3 to 6 months by telephone interview or on outpatient clinic visit, depending on severity of illness and involvement of the referring physician. Repeat echocardiography was performed within 3 months after discharge when possible, every 6 to 12 months thereafter, and whenever clinically indicated. Normalization of LVEF was defined as an increase in LVEF to a final level of ≥50% by echocardiography during follow-up. This study was approved by local ethics committees of Fuwai Hospital.
Continuous variables are expressed as mean ± SD or median (interquartile range) and categorical variables as percentage. For group comparisons, the Student t test or Mann-Whitney U test for continuous variables and chi-square test or Fisher’s exact test for categorical variables were used. Changes in variables from baseline to follow-up in each group were compared using paired Student t test. Risk estimation associated with normalization of LVEF was performed using univariate and multivariate logistic regression models with forward conditional (stepwise) method. After the final model was derived, it was tested for calibration using the Hosmer-Lemeshow chi-square test, and capacity of discrimination was tested using the area under the receiver operating characteristic curve. All tests were 2-tailed, and a significant difference was considered at the p <0.05. Statistical analysis was performed using the SPSS 19.0 statistical software package (SPSS, Inc., IBM, Armonk, New York).
Results
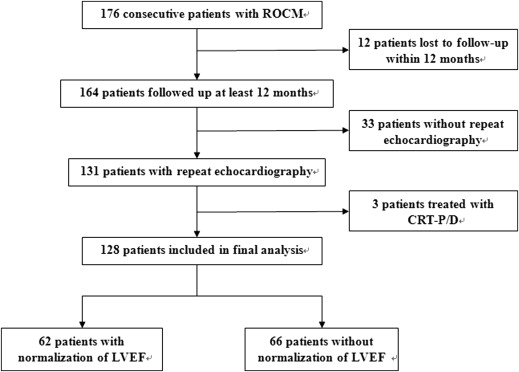
A consecutive cohort of 176 patients with ROCM was reviewed during the period, and 128 patients were enrolled in the final analysis. The study flow diagram is shown in Figure 1 .
The mean age of study subjects was 43 ± 14 years. At baseline, LVEF was 30 ± 6%, left ventricular end-diastolic diameter (LVEDD) was 66 ± 7 mm, symptom duration was 1.9 ± 1.4 months, and percentage of New York Heart Association functional class II, III, and IV on admission was 14%, 59%, and 27%, respectively.
Therapy on discharge included a β blocker in 95%, an angiotensin-converting enzyme inhibitor (ACEI) or angiotensin receptor blocker (ARB) in 84%, spironolactone in 96%, digoxin in 79%, and loop diuretics in 100% of patients. Baseline characteristics are summarized in Table 1 .
| Variable | Normalization of LVEF | p Value | |
|---|---|---|---|
| Yes (n = 62) | No (n = 66) | ||
| Age (yrs) | 44 ± 12 | 42 ± 14 | 0.457 |
| Men | 54 (87) | 49 (74) | 0.067 |
| Body mass index (kg/m 2 ) | 26 ± 5 | 25 ± 4 | 0.214 |
| SBP (mm Hg) | 123 ± 17 | 106 ± 18 | <0.001 |
| Symptom duration (months) | 1.8 ± 1.4 | 2.1 ± 1.5 | 0.176 |
| NYHA functional class | |||
| Class II | 11 (18) | 7 (10) | 0.154 |
| Class III | 31 (50) | 44 (67) | |
| Class IV | 20 (32) | 15 (23) | |
| Hypertension | 27 (44) | 11 (17) | 0.001 |
| Diabetes mellitus | 11 (18) | 17 (26) | 0.273 |
| Atrial fibrillation/flutter | 14 (23) | 9 (14) | 0.188 |
| Hemoglobin (g/L) | 152.7 ± 17.8 | 147.7 ± 16.6 | 0.106 |
| Albumin (g/L) | 41.7 ± 4.2 | 41.6 ± 5.1 | 0.959 |
| Total bilirubin (μmol/L) | 23.1 ± 11.9 | 27.5 ± 18.4 | 0.112 |
| Direct bilirubin (μmol/L) | 4.2 ± 2.7 | 5.7 ± 6.1 | 0.063 |
| Serum creatinine (μmol/L) | 91.3 ± 21.3 | 93.3 ± 23.7 | 0.616 |
| eGFR (ml/min/1.73 m 2 ) ∗ | 90 ± 28 | 87 ± 26 | 0.529 |
| Blood urea nitrogen (mmol/L) | 6.9 ± 2.0 | 7.4 ± 2.7 | 0.294 |
| Serum sodium (mmol/L) | 139.4 ± 2.8 | 138.1 ± 3.6 | 0.027 |
| NT-proBNP (pg/ml) † | 1322.7 (731.4–2183.1) | 1543.7 (863.6–3095.1) | 0.112 |
| QRS duration (ms) | 98 ± 16 | 111 ± 29 | 0.002 |
| Corrected QT interval (ms) | 447 ± 39 | 452 ± 40 | 0.463 |
| Left bundle branch block | 1 (2) | 9 (14) | 0.028 |
| Left atrial diameter (mm) | 43 ± 6 | 43 ± 6 | 0.866 |
| LVEDD (mm) | 63 ± 5 | 69 ± 7 | <0.001 |
| LVEF (%) | 32 ± 6 | 28 ± 5 | <0.001 |
| Right ventricular diameter (mm) | 24 ± 4 | 24 ± 6 | 0.509 |
| Medication on discharge | |||
| ACEI or ARB | 56 (90) | 51 (78) | 0.046 |
| β Blocker | 60 (97) | 62 (94) | 0.448 |
| Spironolactone | 60 (97) | 63 (96) | 1.000 |
| Digoxin | 48 (77) | 53 (80) | 0.689 |
∗ eGFR (ml/min/1.73 m 2 ) = 175 × creatinine −1.234 (mg/dl) × age −0.179 × 0.79 (if female).
† NT-proBNP: 15 patients (12%) with absence of NT-proBNP results.
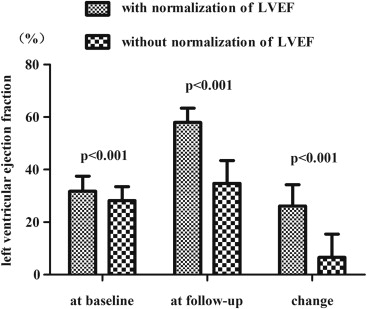
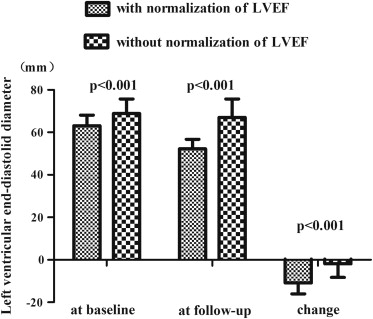
After a mean follow-up of 31 ± 13 months (range 1 to 59), 62 patients (48%) normalized their LVEF, showing a significant increase in LVEF from 32 ± 6% at baseline to 58 ± 5% at follow-up (p <0.001), with a mean increase of 26 ± 8% ( Figure 2 ). This increase in LVEF was associated with a marked decrease in LVEDD from 63 ± 5 to 52 ± 4 mm (p <0.001; Figure 3 ).
The shortest time from diagnosis to normalization was 1 month and the longest was 39 months, with a median time of 6 months. Moreover, 68% (n = 42) patients normalized their LVEF within 1 year after initial diagnosis.
On univariate analysis, normalization of LVEF was significantly associated with a history of hypertension, higher systolic blood pressure (SBP) at presentation, shorter QRS duration and absence of left bundle branch block on electrocardiogram, smaller LVEDD and lower LVEF by echocardiography, and higher serum sodium level ( Table 2 ).
| Variable | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| History of hypertension | 3.857 | 1.700–8.751 | 0.001 | 3.278 | 1.123–9.564 | 0.030 |
| SBP | 1.058 | 1.033–1.083 | <0.001 | 1.041 | 1.015–1.067 | 0.002 |
| QRS duration | 0.973 | 0.955–0.991 | 0.004 | 0.975 | 0.955–0.996 | 0.019 |
| Left bundle branch block | 0.104 | 0.013–0.846 | 0.034 | |||
| LVEDD | 0.848 | 0.790–0.911 | <0.001 | 0.914 | 0.869–0.962 | 0.001 |
| LVEF | 1.127 | 1.051–1.208 | 0.001 | 1.123 | 1.035–1.219 | 0.005 |
| Serum sodium | 1.130 | 1.011–1.263 | 0.031 | |||
Multivariate analysis demonstrated that a history of hypertension (odds ratio [OR] 3.278, p = 0.030), higher SBP at presentation (OR 1.041, p = 0.002), shorter QRS duration (OR 0.975, p = 0.019), smaller LVEDD (OR 0.914, p = 0.001), and higher LVEF (OR 1.123, p = 0.005) by echocardiography at baseline were significantly independent predictors of normalization ( Table 2 ). Accordingly, patients with a history of hypertension, presenting with higher SBP, shorter QRS duration, smaller echocardiographic LVEDD, and higher LVEF at baseline were associated with a higher likelihood of subsequent normalization of LVEF.
Finally, the optimal model to predict normalization of LVEF, written as the logit (linear exponential term of the logistic model), was:
log it P = 1.187 × hypertension + 0.040 × SBP − 0.025 × QRS − 0.090 × LVEDD + 0.116 × LVEF
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


