Uncorrected congenital heart disease (CHD) frequently leads to pulmonary arterial hypertension (PAH), the most severe form of which is Eisenmenger syndrome (ES). We compared patients with idiopathic or heritable PAH (IPAH or HPAH; n = 1,626) against those with CHD-associated PAH (n = 353) who were enrolled in the Registry to Evaluate Early and Long-Term PAH Disease Management (REVEAL Registry). Of patients with CHD-associated PAH, 151 had ES. Compared with the IPAH or HPAH cohort, the ES cohort had greater systemic blood flow (2 ± 1 vs 3 ± 2 L/min/m 2 , p <0.001), lower mean right atrial pressure (10 ± 6 vs 7 ± 4 mm Hg, p <0.001), higher mean pulmonary artery pressure (53 ± 14 vs 65 ± 17 mm Hg, p <0.001), higher pulmonary vascular resistance index (22 ± 12 vs 32 ± 31 Wood units × m 2 , p <0.001), and lower systemic arterial oxygen saturation at rest (92 ± 11% vs 84 ± 13%, p <0.001). At 4 years from enrollment and 7 years from diagnosis, survival rate was similar between IPAH or HPAH and CHD-associated PAH cohorts. For the overall CHD-associated PAH cohort, longer 6-minute walk distance, lower mean right atrial pressure, brain natriuretic peptide level <50 pg/ml, and the presence of acute vasoreactivity were predictors of survival at 4 years from enrollment; younger age and lower mean right atrial pressure were predictors of survival at 7 years from diagnosis. In conclusion, these observations support predicted physiologic differences (e.g., hemodynamics) between patients with IPAH or HPAH and patients with CHD-associated PAH, with or without a systemic-pulmonary shunt. These differences, however, did not translate into significantly improved 4- and 7-year survival rates in patients with ES versus IPAH or HPAH and CHD-associated PAH.
Eisenmenger syndrome (ES) is the most severe form of pulmonary arterial hypertension (PAH) associated with any congenital cardiac defects with unrepaired systemic-to-pulmonary communications and represents a disease state in which pulmonary hypertension is irreversible and the cardiac lesion inoperable. Despite this severity, patients with ES have historically had longer survival than patients with idiopathic PAH (IPAH), although ES shares morphologic features with other origins of PAH. In the present study, we sought to characterize the clinical features and outcomes of patients with congenital heart disease (CHD)–associated PAH enrolled in the Registry to Evaluate Early and Long-term Pulmonary Arterial Hypertension Disease Management (REVEAL Registry). REVEAL provides current information on demographic, clinical, and treatment patterns in patients with World Health Organization group 1 PAH, including the subgroup of CHD-associated PAH. Because several baseline demographic, functional, laboratory, and hemodynamic variables were found to be independently associated with PAH survival rate in a multivariate model, we compared baseline demographic and hemodynamic characteristics, as well as outcomes at 4 years from enrollment and 7 years from diagnosis, of patients with CHD-associated PAH against those of patients with IPAH or heritable PAH (HPAH) enrolled in REVEAL. Our objective was to gain a better understanding of CHD-associated PAH to enhance disease management strategies and thus improve the survival and quality of life of patients with this condition.
Methods
The design and baseline characteristics of the patients enrolled in the REVEAL Registry have been previously described. REVEAL, a longitudinal registry involving 55 pulmonary hypertension centers in the United States (university affiliated and community hospitals), was designed to provide current information about the demographics, course, and management of newly and previously diagnosed patients with World Health Organization group 1 PAH. The data download for this analysis occurred on March 7, 2012.
REVEAL participants include newly (confirmed by diagnostic right-sided cardiac catheterization within 3 months before enrollment) and previously (confirmed by diagnostic right-sided cardiac catheterization ≥3 months before enrollment) diagnosed patients with World Health Organization group 1 PAH. Hemodynamic parameters confirming PAH included (1) mean pulmonary artery pressure ≥25 mm Hg at rest or mean pulmonary artery pressure >30 mm Hg with exercise contemporaneous with pulmonary capillary wedge pressure, (2) pulmonary capillary wedge pressure or left ventricular end-diastolic pressure ≤18 mm Hg, and (3) pulmonary vascular resistance ≥240 dynes•s•cm −5 or ≥3.0 Wood units. The present analysis excluded patients with pulmonary capillary wedge pressure or left ventricular end-diastolic pressure >15 mm Hg or missing data for these parameters.
REVEAL was initiated before the issuance of the 2009 Dana Point 4th World Symposium on PAH and conforms to the 3rd World Symposium on Pulmonary Hypertension recommendations linking pulmonary hypertension classification and PAH definition. Patients in REVEAL were categorized by PAH subgroups, and the present analysis includes IPAH, HPAH, and CHD-associated PAH repaired or unrepaired, with or without ES. Characteristics of patients with CHD-associated PAH were examined separately by repair status. Patients in the unrepaired or partially repaired subgroup were further categorized as having ES if either of the following 2 conditions were met: (1) the clinician determined that the patient had ES as a CHD-associated syndrome or (2) systemic arterial oxygen saturation was <90% based on systemic arterial oxygen saturation at rest from the right-sided cardiac catheterization at diagnosis or enrollment, or oxygen saturation at rest from the 6-minute walk distance at enrollment. The non-ES group included any other patient with unrepaired or partially repaired CHD whose clinician did not indicate ES as a CHD-associated syndrome and whose systemic arterial oxygen saturation values at diagnosis and enrollment were ≥90%. Patients with unrepaired or partially repaired CHD without these data available could not be placed in either the ES or non-ES subgroup.
Acute vasoreactivity was defined in 2 ways: (1) the adult consensus definition, which requires a decrease in mean pulmonary artery pressure of at least 10 mm Hg to a peak vasoreactivity value of <40 mm Hg, combined with an increase or no change in cardiac output and (2) the adaptation of the conventional pediatric criteria, which requires a decrease in mean pulmonary artery pressure of at least 20%, an increase or no clinically significant decrease in cardiac index (cardiac index remaining within normal limits of 2.5 to 4.0 L/min/m 2 ), and a decrease or no change in pulmonary vascular resistance/systemic vascular resistance ratio.
Descriptive statistics are provided for subgroup comparisons, including mean ± SD for continuous variables and percentage of nonmissing values for categorical data. The Fick method was used to calculate pulmonary and systemic blood flows for patients with CHD with unrepaired or partially repaired lesions (the method by LaFarge and Miettinen was used to estimate oxygen consumption). Either Fick or thermodilution methods were used for all other patients. p Values were calculated using the chi-square or Fisher’s exact test (because of small cell counts) for categorical data. The 2-sample t test was used for continuous data that were approximately normally distributed, and the Wilcoxon-Mann-Whitney test was used for continuous data not normally distributed. Because of multiple group comparisons, only p values <0.017 (or 0.05 divided by the 3 subgroup comparisons) should be considered statistically significant based on an overall α level of 0.05 for each variable of interest.
Four-year Kaplan-Meier survival estimates (±standard error) from time of enrollment were calculated for CHD subgroups and patients with IPAH or HPAH, and p values were calculated using log-rank test. Seven-year Kaplan-Meier survival estimates (±standard error) from diagnostic right-sided cardiac catheterization were also calculated for all groups, and p values were calculated from Cox proportional hazards models that accounted for left truncation. For analyses of survival from diagnosis, left truncation methods were used because many patients may not have been enrolled in the study until months or years after diagnosis. The survival of these patients from diagnosis to enrollment indicates that no event occurred during that period; thus, they are not included in the risk set between those 2 time points. Separate stepwise multivariate survival models from enrollment and diagnosis were estimated for all patients with CHD using Cox proportional hazards regressions. The outcome was all-cause mortality, and the model of survival from diagnostic right-sided cardiac catheterization accounted for left truncation. Nine candidate variables were considered for each regression. Candidate variables were selected based on clinical importance and exploratory univariate Cox proportional hazards models. Multiple imputation method was used in the stepwise multivariate models to fill in missing data for candidate predictors and estimate valid standard errors. For the survival analyses, patients who had undergone transplantation were not censored, and follow-up continued after transplantation.
Results
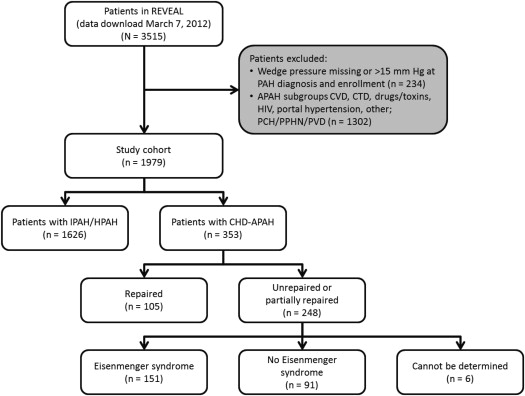
From March 30, 2006 to December 8, 2009, 3,515 patients with newly and previously diagnosed PAH were enrolled in REVEAL. The study cohort consisted of 1,979 patients ( Figure 1 ), of whom 1,626 had IPAH (n = 1,530) or HPAH (n = 96), and 353 had CHD-associated PAH (hereafter referred to as CHD). Within the CHD group, most (n = 248) were unrepaired or partially repaired, including 151 patients classified as having ES, 91 patients classified as not having ES, and 6 patients for whom ES classification could not be determined. Median follow-up from enrollment was 54 months in the overall CHD cohort and 48 months in the IPAH or HPAH cohort.
Demographic characteristics of the patients with IPAH or HPAH and CHD, stratified by CHD subgroups, are listed in Table 1 . Both groups comprised a majority of female patients, an unexpected finding, given that CHD has a relatively equal gender distribution compared with other cardiovascular diseases.
| Characteristic | Repaired CHD (A), n = 105 | Unrepaired or Partially Repaired CHD | IPAH or HPAH (D), n = 1,626 | p (A vs B) | p (A vs D) | p (C vs D) | |
|---|---|---|---|---|---|---|---|
| Unrepaired or Partially Repaired CHD (B), n = 248 | ES (C), n = 151 | ||||||
| Patients aged <19 yrs at diagnosis (%) | 28 (27) | 50 (20) | 32 (21) | 122 (8) | 0.18 | <0.001 | <0.001 |
| Age at date of diagnostic right-sided cardiac catheterization, mean ± SD (yrs) | 32 ± 20 | 35 ± 18 | 35 ± 18 | 47 ± 18 | 0.21 | <0.001 | <0.001 |
| Age at enrollment, mean ± SD (yrs) | 37 ± 19 | 40 ± 17 | 41 ± 16 | 50 ± 18 | 0.16 | <0.001 | <0.001 |
| Women (%) | 76 (72) | 178 (72) | 108 (72) | 1,257 (77) | 0.91 | 0.25 | 0.11 |
| Newly diagnosed | 15 (14) | 31 (13) | 17 (11) | 436 (27) | 0.65 | 0.005 | <0.001 |
| Time from PAH diagnosis to enrollment (mo) | |||||||
| n | 105 | 248 | 151 | 1,626 | 0.49 | 0.001 | <0.001 |
| Mean ± SD | 58 ± 75 | 59 ± 74 | 71 ± 88 | 36 ± 43 | — | — | — |
| 25th, 50th, 75th Percentile | 13, 35, 64 | 16, 36, 74 | 17, 42, 85 | 3, 21, 52 | — | — | — |
| New York Heart Association functional class at PAH diagnosis (%) ∗,† | |||||||
| I | 10 (15) | 4 (2) | 3 (3) | 38 (3) | <0.001 | <0.001 | 0.28 |
| II | 24 (36) | 57 (33) | 24 (23) | 253 (21) | — | — | — |
| III | 31 (47) | 95 (55) | 69 (66) | 725 (60) | — | — | — |
| IV | 1 (2) | 16 (9) | 9 (9) | 186 (16) | — | — | — |
| New York Heart Association functional class at enrollment (%) ∗,‡ | |||||||
| I | 14 (15) | 10 (4) | 5 (4) | 123 (8) | <0.001 | <0.001 | 0.15 |
| II | 46 (50) | 88 (39) | 53 (38) | 507 (31) | — | — | — |
| III | 33 (36) | 113 (50) | 75 (54) | 738 (45) | — | — | — |
| IV | 0 (0) | 14 (6) | 7 (5) | 105 (6) | — | — | — |
| Most recent 6-minute walk test distance at enrollment | |||||||
| n | 77 | 199 | 134 | 1,250 | <0.001 | <0.001 | 0.17 |
| Mean ± SD (m) | 432 ± 106 | 369 ± 120 | 355 ± 125 | 372 ± 135 | — | — | — |
| Six-minute walk test distance at PAH diagnosis | |||||||
| n | 24 | 63 | 38 | 503 | 0.11 | 0.023 | 0.77 |
| Mean ± SD (m) | 395 ± 121 | 348 ± 122 | 322 ± 117 | 329 ± 139 | — | — | — |
∗ The proportions of patients in functional classes I to IV were calculated based on the numbers of patients in each cohort with available data.
† Functional class data at diagnosis were missing for 39 patients in cohort A, 76 patients in cohort B, 46 patients in cohort C, and 424 patients in cohort D. p Values were 0.23 (A vs B), 0.013 (A vs D), and 0.24 (C vs D).
‡ Functional class data at enrollment were missing for 12 patients in cohort A, 23 patients in cohort B, 11 patients in cohort C, and 153 patients in cohort D. p Values were 0.54 (A vs B), 0.49 (A vs D), and 0.39 (C vs D).
Compared with patients in the IPAH or HPAH cohort, patients in the repaired CHD and ES cohorts were significantly younger in age and less likely to be newly diagnosed at enrollment. The median time between PAH diagnosis (by right-sided cardiac catheterization) and enrollment for patients in the IPAH or HPAH cohort was 21 months (interquartile range 3 to 52 months), compared with 42 months (interquartile range 17 to 85 months, p <0.001) for patients in the ES cohort.
Compared with the repaired CHD cohort, a greater proportion of patients in the unrepaired or partially repaired CHD and IPAH or HPAH cohorts were in New York Heart Association functional class III/IV at both diagnosis and enrollment. In addition, patients in the repaired CHD cohort had significantly longer 6-minute walk distance at enrollment than patients had in the unrepaired or partially repaired CHD and IPAH or HPAH cohorts.
From 1% to 5% of patients in each cohort did not have any initial symptoms later attributable to PAH. Among symptomatic patients, the most frequent initial symptom attributed to PAH was dyspnea on exertion, reported more frequently by patients in the IPAH or HPAH cohort (84%) than by patients in the repaired CHD cohort (59%, p <0.001) and in the ES cohort (71%, p <0.001). Dyspnea on exertion was reported more frequently by patients with unrepaired or partially repaired CHD than by those with repaired CHD (71% vs 59%, p = 0.029).
Compared with patients with IPAH or HPAH, patients with repaired CHD reported chest pain and/or discomfort (22% vs 7%, p <0.001) less frequently and palpitations more frequently (12% vs 23%, p = 0.001). Compared with patients with repaired CHD, patients with unrepaired or partially repaired CHD reported chest pain and/or discomfort (7% vs 19%, p = 0.003) more frequently and palpitations (23% vs 15%, p = 0.057) less frequently.
Approximately twice as many patients in the IPAH or HPAH cohort (21%) experienced a syncopal episode, compared with 11% in the repaired CHD cohort (p = 0.008), 12% in the ES cohort (p = 0.007), and 13% in the unrepaired or partially repaired CHD cohort.
The hemodynamic characteristics of patients at diagnosis are summarized in Table 2 . Between the IPAH or HPAH cohort and the repaired CHD cohort, mean pulmonary artery pressure, mean pulmonary vascular resistance index, and mean systemic arterial oxygen saturation at rest were similar. Compared with patients with IPAH or HPAH, patients with ES had significantly greater systemic blood flow and lower mean right atrial pressure, although mean pulmonary artery pressure and mean pulmonary vascular resistance index were significantly lower, and mean systemic arterial oxygen saturation at rest significantly higher, in the IPAH or HPAH cohort than in the ES cohort. Compared with the repaired CHD cohort, mean pulmonary artery pressure and mean pulmonary vascular resistance index were higher, and mean systemic arterial oxygen saturation at rest was lower, in the unrepaired or partially repaired CHD cohort.
| Characteristic | Repaired CHD (A) | Unrepaired or Partially Repaired CHD | IPAH or HPAH (D) | p (A vs B) ∗ | p (A vs D) ∗ | p (C vs D) ∗ | |
|---|---|---|---|---|---|---|---|
| Unrepaired or Partially Repaired CHD (B) | ES (C) | ||||||
| All (n) † | 105 | 248 | 151 | 1,626 | — | — | — |
| Mean right atrial pressure (mm Hg) | 8 ± 4 (95) | 7 ± 4 (237) | 7 ± 4 (144) | 10 ± 6 (1,473) | 0.27 | <0.001 | <0.001 |
| Mean pulmonary artery pressure (mm Hg) | 50 ± 16 (105) | 62 ± 16 (247) | 65 ± 17 (151) | 53 ± 14 (1,625) | <0.001 | 0.023 | <0.001 |
| Mean arterial pressure (mm Hg) | 81 ± 18 (73) | 86 ± 16 (194) | 87 ± 14 (117) | 92 ± 8 (1,093) | 0.048 | <0.001 | 0.002 |
| Mean pulmonary artery pressure/mean arterial pressure ratio (mm Hg) | 0.6 ± 0.2 (73) | 0.7 ± 0.2 (194) | 0.8 ± 0.2 (117) | 0.6 ± 0.4 (1,093) | <0.001 | 0.87 | <0.001 |
| Systolic pulmonary artery pressure (mm Hg) | 77 ± 23 (104) | 96 ± 32 (241) | 102 ± 36 (147) | 83 ± 21 (1,580) | <0.001 | 0.004 | <0.001 |
| Systolic blood pressure (mm Hg) | 111 ± 26 (73) | 117 ± 24 (241) | 117 ± 21 (116) | 125 ± 24 (1,080) | 0.11 | <0.001 | <0.001 |
| Systolic pulmonary artery pressure/systolic blood pressure ratio (mm Hg) | 0.7 ± 0.2 (73) | 0.9 ± 0.3 (190) | 0.9 ± 0.4 (115) | 0.7 ± 0.2 (1,063) | <0.001 | 0.37 | <0.001 |
| Pulmonary capillary wedge pressure ‡ (mm Hg) | 9 ± 3 (105) | 9 ± 4 (245) | 9 ± 4 (149) | 10 ± 4 (1,625) | 0.81 | 0.11 | 0.071 |
| Pulmonary blood flow § (L/min/m 2 ) | 3.0 ± 1.3 (77) | 3.7 ± 4.1 (129) | 3.0 ± 2.3 (82) | 2.3 ± 1.0 (1,224) | 0.16 | <0.001 | <0.001 |
| Systemic blood flow § (L/min/m 2 ) | 3.0 ± 1.3 (77) | 2.8 ± 1.4 (129) | 2.9 ± 1.6 (81) | 2.3 ± 1.0 (1,224) | 0.24 | <0.001 | <0.001 |
| Pulmonary-to-systemic blood flow ratio (L/min/m 2 ) | 0 | 1.6 ± 2.2 (124) | 1.1 ± 0.7 (78) | 0 | — | — | — |
| Pulmonary vascular resistance index (Wood units × m 2 ) | 16 ± 9 (79) | 28 ± 33 (128) | 32 ± 31 (81) | 22 ± 12 (1,228) | 0.001 | <0.001 | <0.001 |
| Systolic vascular resistance index (Wood units × m 2 ) | 27 ± 14 (54) | 37 ± 33 (100) | 36 ± 35 (61) | 41 ± 16 (667) | 0.027 | <0.001 | 0.075 |
| Pulmonary vascular resistance/systolic vascular resistance ratio (Wood units × m 2 ) | 0.6 ± 0.2 (65) | 0.9 ± 1.0 (108) | 1.1 ± 0.9 (67) | 0.6 ± 0.2 (791) | 0.011 | 0.73 | <0.001 |
| SVO 2 ¶ (%) | 68 ± 8 (61) | 63 ± 10 (94) | 61 ± 11 (57) | 62 ± 11 (966) | 0.002 | <0.001 | 0.38 |
| SAO 2 (%) | 93 ± 17 (67) | 88 ± 12 (214) | 84 ± 13 (139) | 92 ± 11 (969) | 0.005 | 0.71 | <0.001 |
| Systemic oxygen transport (ml/min/m 2 ) | 0 | 483 ± 240 (115) | 513 ± 272 (72) | 638 ± 0 (1) | — | — | 0.65 |
| Acute vasoreactivity: adult consensus definition (%) | 6 (11) | 6 (4) | 4 (5) | 100 (11) | 0.10 | >0.99 | 0.11 |
| Acute vasoreactivity: adaptation of conventional pediatric definition | 10 (18) | 12 (9) | 6 (8) | 210 (22) | 0.073 | 0.41 | 0.002 |
∗ p Values are calculated using the chi-square test for categorical data and t test for continuous data. Because of multiple group comparisons, only p values <0.017 (or 0.05 divided by the final number of comparisons) should be considered statistically significant based on an overall α level of 0.05 for each variable of interest.
† Among patients in REVEAL enrolled through December 2009 with wedge pressure ≤15 mm Hg at any time from PAH diagnosis up to enrollment, and group I diagnosis of CHD-associated PAH, IPAH, or HPAH.
‡ Wedge pressure is equal to mean pulmonary capillary wedge pressure at rest, if available, otherwise left ventricular end-diastolic pressure at rest.
§ Pulmonary and systemic blood flows are calculated from the Fick equation for patients with CHD shunts. For all others, they are equal to the Fick cardiac index, if available, otherwise thermodilution cardiac index.
¶ For patients with unrepaired or partial CHD lesions, SVO 2 = O 2 saturation proximal to shunt. All others, SVO 2 = MVO 2 saturation.
Among patients who underwent acute vasodilator testing, 22% of patients in the IPAH or HPAH cohort were responders (adaptation of conventional pediatric definition), compared with 18% (p = 0.41) in the repaired CHD cohort and 8% (p = 0.002) in the ES cohort. The proportion of responders in the repaired CHD cohort was twice than that in the unrepaired or partially repaired CHD cohort (18% vs 9%, p = 0.073). Using the adult consensus definition of acute vasoreactivity, however, the proportion of responders was similar among all the cohorts.
Test results of procedures that patients underwent before enrollment are summarized in Table 3 . Brain natriuretic peptide levels were significantly higher in the IPAH or HPAH cohort than in the repaired CHD cohort but similar between the IPAH or HPAH and ES cohorts. Brain natriuretic peptide levels were also similar between the repaired CHD and unrepaired or partially repaired CHD cohorts.
| Tests/procedures | Repaired CHD (A) | Unrepaired or Partially Repaired CHD | IPAH or HPAH (D) | p (A vs B) ∗ | p (A vs D) ∗ | p (C vs D) ∗ | |
|---|---|---|---|---|---|---|---|
| Unrepaired or Partially Repaired CHD (B) | ES (C) | ||||||
| All (n) † | 105 | 248 | 151 | 1,626 | |||
| Heart rate (beats/min), mean ± SD (n) | 80 ± 14 (101) | 84 ± 17 (239) | 84 ± 16 (149) | 83 ± 15 (1,511) | 0.017 | 0.029 | 0.76 |
| Brain natriuretic peptide level (pg/ml) | |||||||
| Mean ± SD (n) | 110 ± 122 (44) | 224 ± 393 (116) | 263 ± 455 (75) | 271 ± 514 (809) | 0.14 | 0.028 | 0.84 |
| 25th, 50th, 75th Percentile | 30, 69, 167 | 36, 81, 227 | 46, 110, 252 | 35, 106, 297 | — | — | — |
| Percent predicted DL CO | |||||||
| Mean ± SD (n) | 70 ± 18 (49) | 73 ± 27 (107) | 73 ± 27 (71) | 63 ± 23 (914) | 0.48 | 0.039 | <0.001 |
| Any pericardial effusion (%) ‡ | 7 (8) | 27 (15) | 14 (13) | 285 (23) | 0.12 | 0.001 | 0.019 |
| Right ventricular dysfunction (%) | |||||||
| None | 31 (37) | 56 (30) | 36 (32) | 341 (28) | 0.55 | 0.12 | 0.56 |
| Mild | 20 (24) | 38 (20) | 24 (21) | 227 (18) | — | — | — |
| Moderate | 17 (20) | 44 (24) | 28 (25) | 353 (29) | — | — | — |
| Moderate to severe | 2 (2) | 11 (6) | 8 (7) | 69 (6) | — | — | — |
| Severe | 14 (17) | 37 (20) | 18 (16) | 249 (20) | — | — | — |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


