Fig. 27.1
Lateral view of contrast injection in inferior caval vein: a 20 mm conduit is mounted between the inferior caval vein and pulmonary artery; a 4.5 mm fenestration allos righ-to-left shunt into the left atrium
Selective injection in the innominate vein and right hepatic vein is indicated to exclude venovenous connections. An aortogram should be performed to exclude significant aortopulmonary collateral arteries.
Anatomical abnormalities amendable to interventional treatment should be addressed first: balloon dilation and/or stenting of obstructed Fontan connections or stenosed/hypoplastic pulmonary arteries, occlusion of significant collaterals if appropriate and treatment of systemic obstruction (i.e. recoarctation) by balloon dilation and/or stenting.
27.6 Haemodynamic Assessment and Test Occlusion of Fenestration
Identifying “favourable” haemodynamics for fenestration closure is ill defined [4].
Measurement of PVR in Fontan circulation is fraught with difficulties due to inability in accounting for collateral circulation, possibility of pulmonary arteriovenous malformation, low cardiac output state, presence of systemic venous obstruction, unequal distribution of lung flow and possibility of pulmonary venous obstruction. All these factors multiply the error in accurate assessment of PVR.
Test occlusion of the fenestration is used during catheterization to identify patients presumably unsuitable for fenestration closure, by quantifying changes in the systemic or mean venous pressure and systemic saturation. Whether temporary test occlusion in a sedated and intubated patient is a reliable surrogate for predicting physiology in the awake and spontaneously breathing Fontan patient is debatable but is certainly recommended in case of unfavourable baseline haemodynamics and in high-risk patients.
Test occlusion can be performed using a 7-F balloon-tipped, multi-lumen catheter (Swan-Ganz catheter). The balloon catheter is passed over a wire into the systemic atrium; the balloon is inflated using 1 cc diluted contrast and pulled back against the atrial wall/fenestration to allow for temporary occlusion (at least for 15 min).
Alternatively, a small compliant balloon (typically a 6–8-mm Tyshak balloon (depending on fenestration size)) can be inflated within the fenestration itself, using the femoral sheath for pressure and saturation measurement.
Complete occlusion should be confirmed by angiogram (through the proximal port of the balloon-tipped catheter or the femoral sheath) (Fig. 27.2).
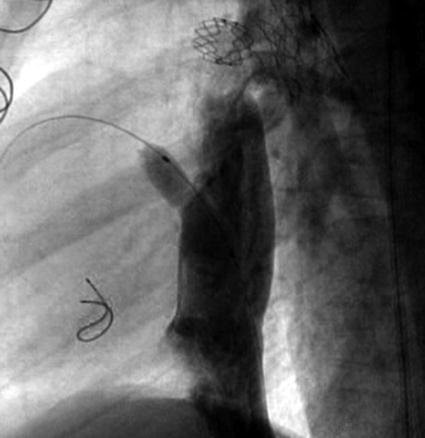
Fig. 27.2
Low-pressure balloon occlusion of 4.5 mm fenestration with a 6 mm Tyshak balloon; contrast injection through venous sheath confirms total occlusion
Measurements should be repeated, documenting VCI mean pressure and saturation and aortic pressure and saturation.
Fenestration occlusion can probably be undertaken safely in patients with a systemic venous pressure of <18 mmHg during test occlusion or in the absence of a significant (>4 mmHg) increase in mean systemic venous pressure or reduction in mixed venous saturation of >10 %.
We would strongly discourage fenestration closure in patients with systemic venous pressure of ≥20 mmHg.
27.7 Choice of Device
When planning transcatheter closure, various factors should be considered, including the size and location of the fenestration, its geometry, the distance between the atrial chamber and the internal edge of the conduit and the possibility of placing a long sheath in the systemic atrium. Patient size and weight should also be taken into consideration.
The ideal device must not only provide complete occlusion with reliable stability but also have a low profile without distorting the anatomy or obstructing flow within the Fontan conduit/baffle.
Along with the diversity of methods to complete the Fontan operation, a number of techniques have been utilized to create fenestrations, depending on the type of Fontan operation (extracardiac conduit versus lateral intra-atrial tunnel) and institutional preference. For the lateral tunnel type of Fontan, a coronary punch is used to create a fenestration in the Gore-Tex baffle. In case of the extracardiac conduit, a fenestration can again be created by placing a coronary punch in the Gore-Tex conduit, after which the atriotomy resulting from detaching the inferior vena cava from the right atrium is sewn to the Gore-Tex graft as a circle of about 2.5 cm, with the fenestration in the centre of the circle. This prevents the adjacent atrial wall from impacting the size of the fenestration. In some centres, the fenestration is made using a short (5–7-mm) polytetrafluoroethylene (PTFE) shunt between the extracardiac conduit and the systemic atrium to decrease unexpected spontaneous closure. Kreutzer et al. described a novel method to create a fenestrated extracardiac Fontan conduit by means of a pericardial tube anastomosed end to end with the inferior inlet of the right atrium [5].
Fenestration size is usually between 3.5 and 5 mm, depending on the type of fenestration (punch hole vs. short PTFE shunt) and patient characteristics (risk stratification).
In addition to intentional fenestrations, significant Fontan baffle leaks exist in up to 15 % of patients with a lateral tunnel-type Fontan. The baffle leaks are mostly located at the base of the right atrial appendage (RAA) at the suture line excluding the superior vena cava flow from the RAA. This suture line seems particularly susceptible to tiny leaks being left postoperatively due to the difficulty in tightly joining a smooth patch material to the corrugated surface created by the pectinate muscles. The increased venous pressure within the baffle can enlarge these channels creating a clinically significant shunt over time. While the origin of the leaks may be similar, the anatomy of the fistulous tract may vary.
Due to the varying location, size and type of fenestrations, several catheterization methods have been described for fenestration closure by multiple authors, including Gianturco coils, detachable coils, clamshell devices, CardioSEAL devices, Amplatzer septal occluders, Amplatzer duct occluders, Amplatzer vascular plugs, Helex septal occluder, Angel Wings devices, Gianturco-Grifka vascular occlusion devices and CARDIA™ PFO star device.
The placement of clips at the time of surgery to mark the location of the fenestration or to narrow the mid-portion of a tube graft for better anchoring of coils or devices has facilitated closure at the time of catheterization.
Over the past two decades, the following devices have been used in our unit for closure of fenestrations and baffle leaks: Rashkind device, CardioSEAL, Amplatzer ASD occluder, Amplatzer VSD occluder and PFO star type device. In search of an ideal device, we modified a 15-mm PFO star (FFD15, CARDIA™, Burnsville, MN) by removal of the left disc to reduce thrombogenicity in the left atrium, increase the amount and length of the LA legs from 2 by 15 mm to 3 by 20 mm to prevent dislodgement and later adding a pivot between the left and right umbrella [6]. We considered this device “ideal” because of its low profile, minimal fabric and metal, good closure rate and non-thrombogenicity. However, introducer sheaths are much larger than needed with the newer devices and although the loading mechanism has been simplified, there remains a learning curve. Currently, the Amplatzer duct occluder type II has become our device of choice for closing the typical punch-hole-type fenestration performed in our extracardiac Fontan conduits. This device has a high conformability and its dual articulating discs makes placement in the fenestration relatively easy. The fabric-free technology allows for delivery through a low-profile 4-F catheter while maintaining a high rate of occlusion without being bulky and potentially obstructive.< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


