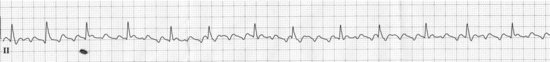
Atrial flutter with variable AV block
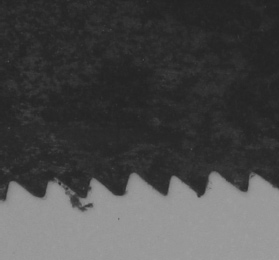
Saw (we can’t assume anything)

Sawteeth (from a real saw)
DESCRIPTION
This is a supraventricular arrhythmia where there’s an actual circuit usually up in the right atrium where a wave of electricity spins around at about 300 times a minute, producing a very characteristic sawtooth pattern in the inferior-looking leads (II, III, and aVf), with no isoelectric baseline between the sawteeth. My carpenter friends inform me that flutter waves more closely resemble a crosscut saw’s teeth than a rip saw’s teeth. This useful information will undoubtedly help in the identification of this arrhythmia, and will be on the test. In other leads the flutter waves are usually not apparent; in V1 you may see little “blips” at the rate of 300, but usually not the sawteeth.
Fortunately for most patients, the AV node cannot conduct each flutter wave to the ventricles, but it can usually conduct every other one, so the ventricular response is at a rate of 1/2 of 300, or 150 beats per minute. Unfortunately, when the conduction is every other flutter wave (or 2:1 conduction as the cognizati like to call it) it may be difficult to see the flutter waves, as they may be buried in the T waves of the complexes. But if the AV node is sick, or if it is blocked by various medications, or if you are pressing on the patient’s eyeball (no longer recommended), or pressing on his/her carotid (acceptable in some circumstances), or immersing his/her face in cold water, the AV node may block more than every other beat and you may see every third (3:1 block) or fewer beats conduct and more clearly identify the flutter waves.
HABITAT
Besides certain aviaries or lepidoptera, flutter is usually found in individuals with structural heart disease, or in individuals with lung disease. There appears to be no predilection for carpenters or sawyers.
CALL
“This patient is staying in sinus tachycardia at 150!”
RESEMBLANCE TO OTHER ARRHYTHMIAS
Atrial flutter with 2:1 AV block is easily mistaken for a sinus tachycardia. In general, however, a patient lying in bed will not have a sinus tachycardia at 150, especially one that is constant and unwavering at or around that rate. If your monitor has the ability to trend heart rate, a trend graph of atrial flutter will show it to jump abruptly to its rate and then not change at all, in contrast to a sinus tachycardia which will usually rise and slow gradually and possibly fluctuate to some extent.
If you can see the flutter waves, there may be arguments (there always are) as to whether what you are seeing is actually atrial flutter, “coarse” atrial fibrillation, or “fib–flutter”. As usual, it doesn’t usually matter, since the drugs and treatment are identical for atrial fibrillation and atrial flutter (anticoagulate and control the rate) unless you are an electrophysiolgist planning an ablation, and in that case you wouldn’t be arguing, you would just know. If the sawteeth really keep changing in shape and aren’t that pointy, especially if you see them best in V1 instead of in II, III, and aVF, it probably isn’t flutter but more likely atrial fibrillation.
CARE AND FEEDING
Atrial flutter can be tricky to care for, because it doesn’t slow gradually and peacefully as atrial fibrillation usually does. Instead, it slows (if it slows at all) by quantum drops in heart rate. To wit, if we start with 2:1 block (rate 150, 1/2 of 300) and add some verapamil, we may drop to 3:1 (1/3 of 300), rate 100. Pretty nice, eh? But what if the sub-intern decides she’d like it just a bit slower so she gives some intravenous β-blocker, and suddenly we’re down to 6:1 block (1/6 of 300), rate 50. Lots of flutter waves and not that many QRS complexes, and everyone’s sweating! So we stop all the slower-downers (digoxin, verapamil, diltiazem, β-blockers) and before you know it, we’re back with 2:1 block at 150 per minute again! Sometimes it’s just easier and safer to electrically cardiovert the patient rather than struggle with all the pharmacology. Just make sure all the anticoagulation rules are obeyed (same as Atrial fibrillation, see page 23), and maybe check with your electrophysiologist. As opposed to atrial fibrillation, they can actually ablate atrial flutter with their hot little catheters with a high likelihood of success.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


