Migraine is a common neurovascular disorder characterized by attacks of severe headache, autonomic and neurologic symptoms. Migraine can affect many systems in the body, yet its effects on cardiovascular system are unclear. We hypothesized that migraine and coronary microvascular angina may be manifestations of a common systemic microvascular dysfunction and clinically associated. Forty patients with migraine and 35 healthy volunteers were included into the study. Using transthoracic Doppler echocardiography, coronary flow was visualized in the middle or distal part of the left anterior descending artery. Coronary diastolic peak flow velocities were measured with pulse wave Doppler at baseline and after dipyridamole infusion (0.56 mg/kg/4 min). Coronary flow reserve of <2 was considered normal. In addition, thorough 2-dimensional and Doppler echocardiographic examinations were also performed. Fifty-two women and 23 men were included. Coronary flow reserve was significantly lesser in the migraine group than in the control group (1.99 ± 0.3 vs 2.90 ± 0.5, p <0.05). In addition, mitral annular velocities were lower and the ratio of early mitral inflow velocity to early mitral annular velocity (E/E′ lateral and E/E′ septal) was higher in migraineurs than in the control group (p <0.05 for all), indicating diastolic function abnormalities in the migraine group. In conclusion, these findings suggest that there is an association between coronary microvascular dysfunction and migraine independently of the metabolic state of the patients. A common pathophysiologic pathway of impaired endothelial vasodilatation, vasomotor dysfunction, and increased systemic inflammatory factors may play a role in these 2 clinical conditions and could be the underlying cause of subclinical systolic and diastolic left ventricular dysfunction in migraineurs.
Pathophysiology of migraine includes changes in cortical excitability, neuroinflammation, and dysfunction of the vascular wall. Several studies indicate that migraine is associated with inflammatory markers, oxidative stress and thrombosis, high blood pressure, hypercholesterolemia, impaired insulin sensitivity, high homocysteine levels, stroke, generalized peripheral vasoconstriction, decreased brachial artery flow–mediated dilatation and increased nitrate-mediated response, microvascular retinal abnormalities, and reduced circulating endothelial progenitor cells, which are surrogate biological markers of impaired vascular function and high cardiovascular risk. All indicate the possibility of migraine being a local manifestation of a systemic vascular abnormality rather than a primary cerebral phenomenon. Accordingly, we hypothesized that patients with migraine have greater incidence of coronary microvascular dysfunction compared with healthy controls.
Methods
Forty patients with migraine who were diagnosed according to 2004 International Headache Society guideline and 35 healthy volunteers from 18 to 55 years of age were included in this study. Patients were excluded if they had documented coronary artery disease, diabetes mellitus, hypertension, dyslipidemia, severe valvular disease, congenital heart disease, hypertrophic cardiomyopathy, chronic heart failure, cardiac rhythm other than sinus, thyroid disease, chronic obstructive pulmonary disease, cor pulmonale, systemic diseases such as collagenosis, hemolytic, hepatic, and chronic renal disease, or inadequate visualization of coronary flow on transthoracic Doppler echocardiogram. Coronary artery disease was defined as the presence of one of the following: typical angina, ST-segment or T-wave changes specific for myocardial ischemia, Q-waves or incidental left bundle branch block on electrocardiogram, wall motion abnormality on echocardiogram, a noninvasive stress test revealing ischemia or any perfusion abnormality, or a history of a myocardial infarction or revascularization. Patients having unequivocal symptoms underwent a noninvasive stress test, treadmill exercise, or myocardial perfusion scintigraphy, and those demonstrating positive results were excluded. The study complies with the Declaration of Helsinki. All participants gave written informed consent, and the study protocol was approved by the institutional ethics committee.
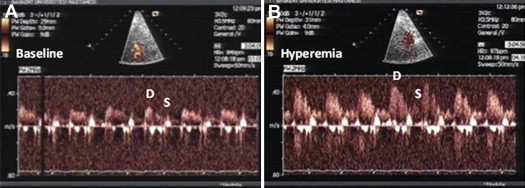
Transthoracic echocardiography was performed with a commercially available cardiac ultrasound system (Acuson Sequoia C256; Acuson Siemens, Mountain View, California) equipped with a broadband 3.5 MHz transducer with second harmonic capabilities. All patients underwent standard 2-dimensional and Doppler echocardiographies conforming to the American Society of Echocardiography/European Association of Echocardiography recommendations. In addition, longitudinal myocardial systolic and diastolic velocities at the mitral annular level from the lateral and septal sites were measured using pulsed-wave tissue Doppler in the apical 4-chamber view. Coronary flow was assessed in the mid to distal left anterior descending artery using a modified foreshortened view obtained by slightly sliding the transducer upward and medially from an apical 2-chamber view. For color Doppler coronary flow mapping, velocity ranges from ±11 to ±24 cm/s were selected, and left anterior descending artery color flow was searched over the epicardial part of the distal anterior wall. Pulsed-wave Doppler signal of the left anterior descending artery flow that displayed a characteristic biphasic flow pattern, with larger diastolic and smaller systolic components, was recorded under color Doppler guidance ( Figure 1 ). Systolic and diastolic peak velocities were recorded at baseline and under induced hyperemia by 0.56 mg/kg dipyridamole infusion over 4 minutes. Coronary diastolic peak velocities (DPVs) were measured at baseline and after dipyridamole infusion. The 3 highest Doppler recordings were averaged for each measurement. Coronary flow reserve (CFR) was calculated as the ratio of hyperemic to baseline DPV. A CFR value of <2 was accepted as abnormal. Heart rate, blood pressure, and electrocardiographic variables were monitored during the studies.
All analyses were conducted using SPSS software (Statistical Package for the Social Sciences, version 11.5; SSPS Inc., Chicago, Illinois). Continuous variables are expressed as mean ± SD or median (interquartile range) and categorical variables as percentages. The Shapiro-Wilk test was used to test the normality of distribution. Variables with a normal distribution were compared by a Student’s t test or univariate analysis of variance. Variables that showed a nonhomogenous distribution were compared by the Mann Whitney U test. Categorical variables were compared with the chi-square test. Correlations were studied by the Spearman’s correlation test. Multivariate logistic regression analysis was performed to determine independent parameters associated with CFR. A p value <0.05 was considered statistically significant.
Results
Table 1 presents a comparison of the clinical and laboratory variables of the 2 groups. Eleven patients (28%) had migraine with aura and 29 patients (73%) without. In patients with migraine, levels of total cholesterol, low-density cholesterol (LDL), triglyceride were higher than those in control, and high-density cholesterol level was lower than that in controls (p <0.05 for all).
| Clinical Characteristics | Migraine (n = 40) | Control (n = 35) | p |
|---|---|---|---|
| Age (yrs) | 31 ± 8 | 34 ± 8 | NS ∗ |
| Women (%) | 73 | 66 | NS † |
| Body mass index (kg/m²) | 24 ± 4 | 25 ± 4 | NS ∗ |
| Total cholesterol level (mg/dl) | 186 ± 332 | 168 ± 31.4 | 0.03 ∗ |
| High-density lipoprotein (mg/dl) | 43 ± 9 | 51 ± 14 | 0.01 ∗ |
| Low-density lipoprotein (mg/dl) | 114 ± 23 | 96 ± 30 | 0.01 ∗ |
| Triglycerides (mg/dl) | 122 ± 36 | 100 ± 47 | 0.04 ∗ |
| Creatinine (mg/dl) | 0.7 ± 0.1 | 0.7 ± 0.2 | NS ∗ |
| C-reactive protein (mg/L) | 1.3 (0.1–15.4) | 0.8 (0.1–11.0) | NS ‡ |
| Hemoglobin (g/dl) | 14 ± 2 | 14 ± 2 | NS ∗ |
| Leukocytes (1,000/μl) | 5.700 ± 4 | 6.660 ± 2 | NS ∗ |
| Thrombocytes (1,000/μl) | 269 ± 50 | 255 ± 61 | NS ∗ |
Two-dimensional, Doppler, and tissue Doppler echocardiographic examination findings are presented in Table 2 . Left ventricular diastolic and systolic diameters, ventricular wall thicknesses, and left ventricular mass index were similar in both groups. There were no significant differences with respect to left ventricular ejection fraction between the groups. However, septal and lateral mitral annular systolic velocities were lower in migraineurs than in the control group (p <0.05). The ratio of early mitral diastolic flow velocity to annular velocity (E/E′ lateral and E/E′ septal), which indicates the left ventricular filling pressure, was higher in the migraine group than in the control group (p <0.05). During dipyridamole infusion, no significant electrocardiographic changes or adverse effects were observed including headache. There were no significant differences between systolic and diastolic blood pressures at rest and during hyperemia. Heart rate was similar at baseline in both groups and increased similarly after dipyridamole infusion. The mean baseline DPV was also similar in both groups. However, DPV at hyperemia was significantly lower in patients with migraine compared with controls (p <0.0001), and CFR was significantly less in the migraine group than in the control group (1.99 ± 0.3 vs 2.90 ± 0.5, p <0.05). There were 17 (43%) of 40 patients with migraine with impaired CFR compared with 3 (8.5%) of 35 control patients (p = 0.001). No significant difference was observed in CFR between the migraineurs with and without aura (1.9 ± 0.4 vs 2.08 ± 0.2, p = NS). Women were more frequent in both groups and CFR was significantly less in women compared with men (2.32 ± 0.6 vs 2.63 ± 0.6, p <0.05).
| Echocardiographic Data | Migraine (n = 40) | Control (n = 35) | p |
|---|---|---|---|
| 2-Dimensional measurements | |||
| Interventricular septum (cm) | 0.9 (0.6–1.2) | 0.9 (0.5–1.1) | NS † |
| Posterior wall (cm) | 0.8 (0.6–1.2) | 0.9 (0.5–1.1) | NS † |
| Left ventricular diastolic diameter (cm) | 4.0 ± 0.3 | 4.2 ± 0.5 | NS ∗ |
| Left ventricular systolic diameter (cm) | 2.5 ± 0.2 | 2.7 ± 0.3 | NS ∗ |
| Ejection fraction (%) | 56 (50–67) | 59 (50–64) | NS † |
| End-diastolic volume (ml) | 86 ± 17 | 86 ± 17 | NS ∗ |
| End-systolic volume (ml) | 38 ± 9 | 35 ± 8 | NS ∗ |
| Stroke volume (ml) | 47 ± 11 | 51 ± 11 | NS ∗ |
| Left ventricular mass index (g/m²) | 62 (33–81) | 60 (38–94) | NS † |
| Doppler measurements | |||
| Mitral lateral systolic velocity (cm/s) | 11 ± 2 | 13 ± 3 | 0.02 ∗ |
| Mitral septal systolic velocity (cm/s) | 9 ± 2 | 11 ± 3 | 0.001 ∗ |
| Mitral lateral early mitral annular velocity (cm/s) | 16 ± 4 | 19 ± 3 | 0.001 ∗ |
| Mitral septal early mitral annular velocity (cm/s) | 14 ± 4 | 16 ± 4 | 0.006 ∗ |
| Mitral early mitral inflow velocity wave (cm/s) | 83 ± 15 | 85 ± 13 | NS ∗ |
| Mitral late mitral inflow velocity wave (cm/s) | 65 ± 11 | 62 ± 12 | NS ∗ |
| Early mitral inflow velocity/late mitral inflow velocity | 1.2 (0.6–1.8) | 1.3 (1.0–2.0) | NS † |
| Early mitral inflow velocity/early mitral annular velocity lateral | 5.1 (2.7–11) | 4.5 (2.8–7.0) | 0.01 † |
| Early mitral inflow velocity/early mitral annular velocity septal | 6.3 (2.7–12) | 5.2 (3.5–7.6) | 0.007 † |
| Measurements related to coronary flow assessment | |||
| Baseline heart rate (beats/min) | 76 ± 8 | 73 ± 12 | NS ∗ |
| Baseline systolic blood pressure (mm Hg) | 110 (80–140) | 110 (100–140) | NS † |
| Baseline diastolic blood pressure (mm Hg) | 75 (60–90) | 70 (60–80) | NS ∗ |
| Peak heart rate (beats/min) | 100 ± 11 | 96 ± 14 | NS ∗ |
| Baseline diastolic peak coronary flow velocity (cm/s) | 30 (22–43) | 28 (22–47) | NS † |
| Baseline systolic peak coronary flow velocity (cm/s) | 19 ± 3 | 19 ± 4 | NS ∗ |
| Hyperemic diastolic peak coronary flow velocity (cm/s) | 61 ± 9 | 83 ± 13 | <0.0001 |
| Hyperemic systolic peak coronary flow velocity (cm/s) | 30 (23–46) | 40 (25–66) | <0.001 ∗ |
| CFR | 1.99 ± 0.3 | 2.08 ± 0.2 | <0.05 ∗ |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


