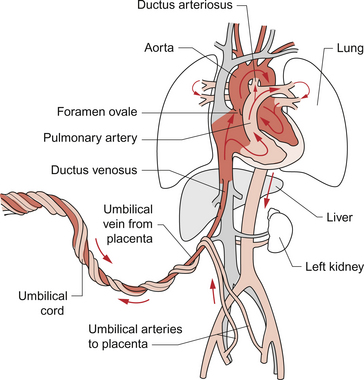
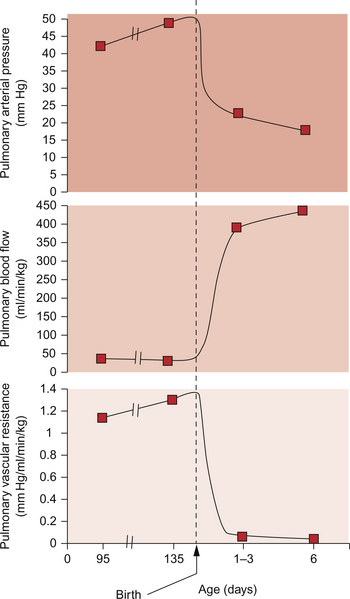
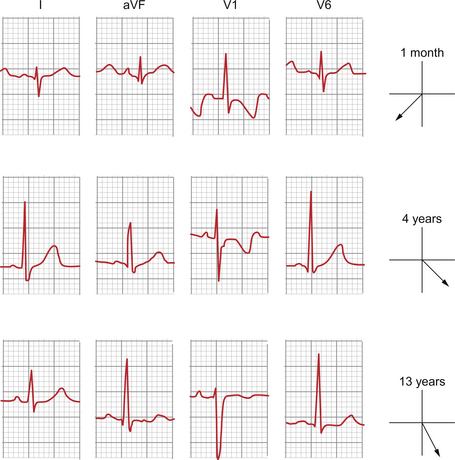
12 Though the main functions of the fetal cardiovascular system are the same as in the adult, i.e. the distribution of oxygen and nutrients to the body and the transfer of carbon dioxide and waste products to the organ of excretion, there are some fundamental differences. Before birth the lungs are collapsed and filled with fluid and the organ of oxygenation, nutrient delivery and waste excretion is the placenta. The fetus is essentially a parasite and must extract oxygen and nutrients from the maternal circulation. Despite adaptations, such as an increased affinity of fetal haemoglobin (HbF) for oxygen compared with adult haemoglobin (HbA), the fetus exists in a state of relative hypoxia. Haemoglobin in the blood returning from the placenta is generally around 80% saturated with oxygen compared to above 98% in the pulmonary venous blood of a child or adult (see Chapter 1). Carbon dioxide levels are correspondingly elevated in the fetus. It is important to remember that the fetus is adapted to tolerate these conditions and aspects of this adaptation initially persist after birth. As in adult life the brain, after the heart, is the dominant oxygen demanding organ. In contrast to the adult, in the fetus the oxygen supply comes from the placenta and so the most highly oxygenated blood arrives at the heart in the inferior vena cava rather than in the pulmonary veins. This blood is partially desaturated at around 80% despite the high affinity of HbF for oxygen. In order to ensure optimum supply of oxygen to the brain the fetal circulation has two major structural differences compared to that in the adult, the ductus arteriosus and the foramen ovale. Figure 12.1 summarizes the fetal circulation. The division of blood flow at the level of the right atrium has an important impact on the flow of blood around the aortic arch. Since the major recipient of the relatively well oxygenated blood is the brain, only a small proportion (about 10%) of the left ventricular output passes through the section of the aortic arch between the origin of the left subclavian artery and the opening of the ductus arteriosus. To re-cap, the main features of the fetal circulation compared with the adult circulation are as shown in Table 12.1. Table 12.1 Main features of the fetal circulation compared with the adult circulation Sometimes transition from fetal to adult circulation at birth is incomplete, leading to so-called persistent fetal circulation. An example of a case history is shown in Case 12.1:1. The first breath opens the airways and allows gas exchange across the alveolar membrane. The lungs expand and blood vessels open. This initiates a drop in the pulmonary vascular resistance (see Figure 12.5). Combined with the sudden rise in peripheral resistance resulting from the loss of the low-resistance placenta, there is a profound alteration in haemodynamics in the newborn infant. The blood leaving the right ventricle is preferentially directed through the now low-resistance lungs and returns to the left atrium. This increase in venous flow into the left atrium raises the left atrial pressure. At the same time there is a fall in right atrial pressure because venous return to this chamber has been reduced following the loss of the placental circulation. As left atrial pressure is now higher than right atrial pressure the foramen ovale, a flap valve, closes. Thus, in the newborn any detectable flow across the atrial septum is predominantly left to right. With the changes in pressures and the establishment of lung ventilation there is a sharp increase in blood oxygen content. This improved tissue oxygenation reduces the acidaemia to which the fetus has been adapted. Rising pH and Pao2 inhibit the synthesis of prostaglandins in the ductus arteriosus. This leads to closure of the ductus arteriosus separating the pulmonary circulation from the systemic circulation. Though generally the duct has closed within 24 hours of birth, early echocardiography demonstrates that a small left to right ductal shunt persists in a large minority of newborns for some days or even weeks. However this shunt is not usually of clinical significance. Table 12.2 summarizes the normal variation of HR and BP with age. An estimate of the normal systolic BP, for a given age in children, can be made from the formula: systolic BP = 80 + (2 × age in years). Table 12.2 Heart rate and BP variations with age The variation in heart rate reflects the relatively small size of the infant heart compared with its body mass and the relatively low compliance (increased stiffness) of the ventricles. The stiff ventricles mean that the stroke volume of the heart responds less dramatically to increasing venous return (preload effects) compared to an adult (see Chapter 4). In order to meet the demand for increased cardiac output the newborn heart rate must rise substantially, even at rest. Thus it is not unusual to see heart rates in newborns varying from 90 bpm when deeply asleep to 160 bpm when only slightly active. In the sick newborn under stress heart rates over 200 bpm may be seen with the heart still in sinus rhythm. Broadly speaking the ECG of the child has the same components as that of the adult, i.e. P waves, QRS complexes and T waves (see Chapter 7). However the relative contribution of the right and left ventricles to the shape of the ECG trace is different in children compared to adults. There is therefore a progressive change in the pattern of the ECG through childhood which reflects the declining contribution of the muscle mass of the right ventricle compared to the left ventricle. The large muscle mass of the newborn right ventricle affects the axis of the QRS complex in the frontal plane. The axis of the frontal QRS vector in the infant may be well past the upper limit of normal for the adult with the normal range being as high as +180°. Again, with time and the involution of the right ventricle, the axis ‘swings’ leftwards until it reaches the normal range for adults −30° to +90° (see Chapter 7). This change over time means that the acceptable axis for children in the frontal plane is very wide ranging. Broadly speaking, the axis should be inferior, i.e. between 0° and 180°. Deviation above the horizontal axis should be considered abnormal in the absence of evidence to the contrary. In the presence of physical evidence to support it a rightwards axis more extreme than usual may be suggestive of a residual load on the right ventricle. Put simply if the QRS vector is positive (i.e. pen deflection is upwards) in lead aVF then the vertical plane axis of the heart is probably normal. The chest leads are particularly informative. In V1 the QRS complexes are initially dominantly positive with a dominant R wave reflecting depolarization in the relatively hypertrophied septum. T waves in V1 may be positive in the first 2 weeks of life but then become negative and remain inverted up until late childhood. The initial solely, or dominantly, positive deflection in V1 slowly becomes equiphasic and by adulthood will be purely negative in the majority of normal ECGs. Figure 12.2 shows the typical variation. Broadly, the normal range for the intervals between successive components of the ECG for children are shorter than for adults and generally the younger the child the shorter the interval. This largely reflects the physical size of the heart, as a wave of electrical activity spreading through a smaller heart has a shorter distance to travel and so takes less time. This generalization applies for everything but the index referred to as the corrected QT interval (QTc). This is defined as the QT interval/square root (preceding R–R interval). Generally this falls with increasing age. Identification of the QTc has become clinically more important with increasing understanding of the role that abnormal repolarization plays in sudden death in young people. This may be evident in prolongation of the QTc above the normal range for an adult on the resting ECG.
FETAL CARDIOVASCULAR SYSTEM AND CONGENITAL HEART DISEASE
Introduction
Fetus
Adult
Newly oxygenated, but still partially desaturated, blood leaves the placenta and arrives at the right atrium in the inferior vena cava
Blood which is nearly fully saturated with oxygen arrives at the left atrium via the pulmonary veins
Pressure in right atrium is higher than that in the left atrium
Left atrial pressure is higher than that in the right atrium
Right-to-left shunting of blood occurs across the foramen ovale
There is no shunt at atrial level
The right ventricle supplies blood to the systemic circulation
The right ventricle only supplies blood to the pulmonary circulation
The right ventricle output predominantly passes through the ductus arteriosus into the aorta
The right ventricle output passes to the lungs
Resistance to blood flow is low in the placenta and this leads to a low peripheral resistance overall
Peripheral resistance to blood flow is high
Stiff, fluid-filled, lungs have high resistance to flow
Expanded, air-filled lungs, have low resistance to blood flow
How does the transition from fetal to adult circulation occur?
Changes at birth
Longer term changes in the heart during childhood and adulthood
Age (yr)
HR (bpm)
Systolic BP (mm Hg)
<1
110–160
70–90
1–2
100–150
80–95
2–5
95–140
80–100
5–12
80–120
90–110
>12
60–100
100–120
The normal ECG in childhood
Thoracic Key
Fastest Thoracic Insight Engine