Femoral Endarterectomy with Profundaplasty
Michael Belkin
James T. McPhee
The common femoral artery (CFA) and proximal profunda femoral artery (PFA) are frequent sites of atherosclerotic occlusive disease. Furthermore, the CFA is the access point for many aspects of vascular surgery procedures as well as many other diagnostic and therapeutic interventional procedures including aneurysm-related and coronary interventions. The presence or absence of occlusive disease at the femoral level may be that which dictates one’s candidacy for purely percutaneous revascularization attempts of either the iliac or superficial femoral arteries or whether open surgical reconstruction is indicated. In general, attempting downstream interventions beyond a diseased CFA or in-flow procedures above a diseased CFA without formally addressing the common femoral disease is ill advised and unlikely to yield a durable result. Despite reports to the contrary, there is currently no realistic role for endovascular interventions within the common femoral or PFA, leaving these two vessels almost exclusively in the domain of open vascular reconstruction.
In general, the profunda femoral is an underappreciated blood vessel in the human body. Its robust collateral network is that which allows for downstream reconstitution of inflow occlusions by way of hypogastric and circumflex iliac connections. It is also that vessel which provides limb-saving collateral flow beyond superficial femoral arterial occlusions. A common mantra we maintain on our service, particularly in smokers, is, “as goes the profunda, so goes the leg.” Simply stated, patency of the profunda, as well as durable reconstructions thereof plays heavily into not only the symptom resolution of one’s lower extremity occlusive disease but more so whether or not they keep their leg long-term.
Indications for femoral artery reconstruction are similar to those for any peripheral vascular reconstruction including life-limiting claudication in a patient failing maximal medical intervention (smoking cessation, walking regimen, antiplatelet therapy, and statin use for LDL goal <70 mg/dL), ischemic rest pain, or tissue loss. CFA as well as PFA reconstruction typically consists of endarterectomy and patch angioplasty (EA/PA). This technique allows for restored luminal flow as well as a soft, sewable landing zone for an inflow procedure or takeoff point for an adjunctive outflow procedure. Occasionally,
CFA and PFA reconstruction may stand alone as isolated procedures, particularly in claudicants or patients with ischemic rest pain, but they are more typically performed in conjunction with either inflow or outflow procedures, specifically when one suffers from more severe critical limb ischemia symptoms such as tissue loss. Not uncommonly, an inflow aortobifemoral or axillobifemoral bypass will require CFA reconstruction to maximize graft outflow. Likewise, a distal bypass may require CFA/PFA reconstruction to maximize graft inflow and/or to insure that the thigh is revascularized in addition to the infrageniculate limb. In addition, CFA/PFA reconstruction typically serves as the access point for hybrid reconstructions whereby retrograde iliac or antegrade superficial femoral artery (SFA) interventions may be performed through the newly constructed PA in the case of multilevel disease.
CFA and PFA reconstruction may stand alone as isolated procedures, particularly in claudicants or patients with ischemic rest pain, but they are more typically performed in conjunction with either inflow or outflow procedures, specifically when one suffers from more severe critical limb ischemia symptoms such as tissue loss. Not uncommonly, an inflow aortobifemoral or axillobifemoral bypass will require CFA reconstruction to maximize graft outflow. Likewise, a distal bypass may require CFA/PFA reconstruction to maximize graft inflow and/or to insure that the thigh is revascularized in addition to the infrageniculate limb. In addition, CFA/PFA reconstruction typically serves as the access point for hybrid reconstructions whereby retrograde iliac or antegrade superficial femoral artery (SFA) interventions may be performed through the newly constructed PA in the case of multilevel disease.
Additional applications for CFA reconstruction may relate to maximizing one’s candidacy for either remote cardiac interventional procedures (valvuloplasty/valve replacement) or endovascular aneurysm repairs. In certain patients, iliofemoral occlusive disease could otherwise obviate endovascular approaches to aneurysmorrhaphy or more advanced cardiac interventions. This may relegate these patients to more invasive open thoracic approaches, which in some, may be prohibitive.
Contraindications to femoral arterial reconstruction are few and are mostly related to the presence of coexistent systemic disease. While CFA reconstruction is feasible to perform under regional or local anesthetic, more commonly, this will be done with general anesthesia and therefore appropriate cardiovascular risk stratification should be performed. Patients with prior radiotherapy treatment to the groin or with active infection or multiple prior interventions should be considered on a case-by-case basis before proceeding as groin level wound complications may be devastating.
With femoral level occlusive disease one may encounter either a weakly palpable or an absent femoral pulse on physical examination. In nonobese patients, palpation of the external iliac artery above the inguinal ligament may be possible and helpful in determining to what degree iliac occlusive disease is present if a pulse is present at that level. Even in the absence of a femoral pulse one would expect to palpate at least a calcific cord in the region of the CFA, which even in a patent artery, may be too calcified to transmit a detectable impulse. Pulse palpation is made additionally challenging by the emerging obesity problem. After noninvasive studies have confirmed femoral level disease (either resting or exercise ankle brachial indices [ABIs]), further preoperative evaluation may consist of imaging by way of computed tomography angiography (CTA), magnetic resonance angiography (MRA), or digital subtraction angiography (DSA). This will allow for assessment of concurrent inflow or infrainguinal occlusive disease and proper operative planning. DSA may provide the added benefit of allowing for pressure gradient measurements as well as the potential for intervention. There is an additional noninvasive measure that bears mentioning known as the profundapopliteal collateral index (PPCI). Mathematically, this refers to a preoperative segmental pressure gradient across the knee joint and is expressed as: above-knee pressure–below-knee pressure/above-knee pressure. Patients with a larger gradient across the knee joint (>0.5) are less likely to benefit from an adjunctive profundaplasty. As previously mentioned, while isolated single level common femoral or profunda occlusive disease does occur, this is the exception rather than the rule, and one must plan accordingly if the need for additional inflow or outflow procedures at the time of femoral artery reconstruction based on the patient’s presenting symptoms is warranted.
In our experience, the quality of noninvasive imaging has improved to the extent where many patients may not routinely require formal angiogram if their disease burden is limited to the aortoiliac or iliofemoral systems. Those with multilevel occlusive disease and certainly those patients who require infrainguinal bypass may still be best served by formal diagnostic angiography.
Positioning
Patients undergoing femoral artery reconstruction should be placed supine on an angiographically suitable operative table. The table pedestal will typically be oriented toward the feet to allow for adjunctive inflow arteriography at the time of the femoral reconstruction, if needed. Both groins are clipped of hair. We find excluding the genitalia circumferentially with an impervious drape before prepping helps minimize infectious complications. The abdomen, groins, and thighs are prepped with a chlorhexidine-based preparation solution.
As in any vascular surgical reconstruction one must have a primary plan as well as a “bail out” or back-up plan. In the case of CFA/PFA level reconstruction, potential pitfalls may relate to disruption of either inflow or outflow tracts at the time of surgery. If the inflow disease is more progressive than initially believed, one should be poised to perform retrograde angiography and adjunctive iliac intervention to ensure maximal inflow into the reconstruction. We routinely include the contralateral groin in the operative field, so in the event that retrograde techniques are unsuccessful due to dissection or occlusion, contralateral CFA access may be obtained to facilitate up-and-over antegrade iliac endovascular intervention. Including the contralateral groin in the field has the added benefit of allowing for femoral crossover grafting for inflow if endovascular maneuvers are unsuccessful. Similarly, if the endpoint on the SFA should become compromised or untenable it is beneficial to have distal revascularization options. To that end maintaining the entire ipsilateral leg in the preparatory field will allow for assessment of distal perfusion as well as adjunctive SFA intervention or distal bypass if the need should arise.
Ioban is used to exclude all exposed skin and the patient is draped from the thighs to the upper abdomen. Including the abdomen in the field allows for emergency iliac artery or aortic access if complications related to adjunctive iliac interventions should arise.
Technique
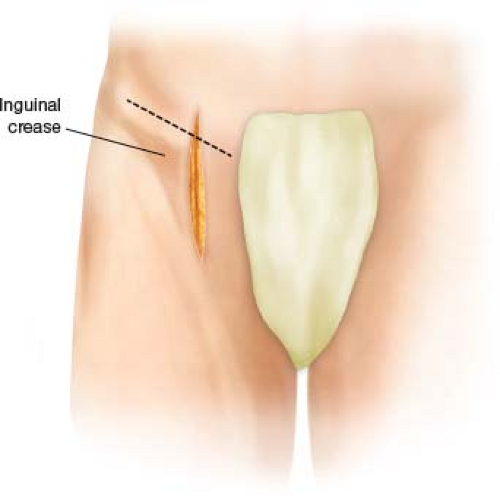
While oblique incisions above the inguinal fold are appropriate for exposure of otherwise healthy CFAs for endograft placement, more extensive exposure will be typically needed for femoral artery and profunda reconstruction. To that end, an obliquely oriented or strictly longitudinal incision from the level of the inguinal ligament through the groin fold is the best approach to the femoral vessels for the purposes of reconstruction (Fig. 23.1). A standard approach to the CFA is performed with specific attention paid to serial ligation of lymph nodes and lymphatic tissue as the dissection is deepened through the subcutaneous tissue and fat (Fig. 23.2). It is preferable to work in a lateral to medial fashion, sweeping the lymphatic tissue medially toward the femoral vein. This will allow the lymphatics to be mobilized more so than divided, further limiting the risk of postoperative lymphatic leakage. Weitlaner retractors are used at the upper pole and lower poles of the incision to maximize exposure. Often, no femoral pulse is appreciated in these patients, but the dissection can be oriented toward the firm calcific wall of the femoral artery. In the rare occasion where no pulse or calcium is appreciated one is best served by identifying the inguinal ligament, at which point the femoral vessels will be traversing directly beneath.
With each new layer of tissue that is divided, deepening the retraction will serve to maximize the exposure of the femoral vessels. An assistant or fixed upper arm retractor with either an Army-Navy or Ladyfinger style retractor may be used at the upper pole of the incision to gently retract the inguinal ligament allowing further access onto the external iliac artery. Rarely fixed cephalad retraction with fixed retractors such as the Bookwalter system may be useful in morbidly obese patients.
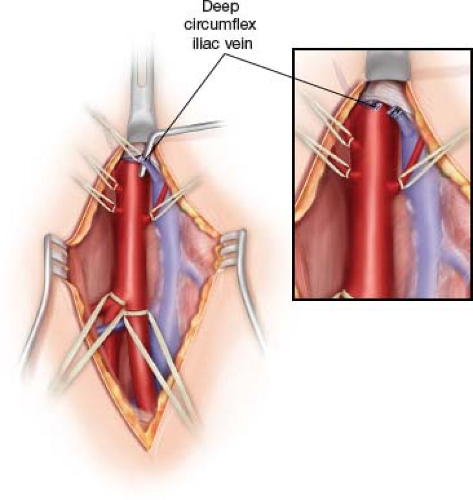
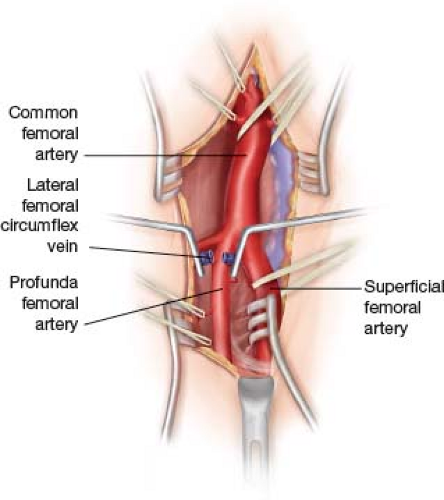
To perform a proper CFA EA and reconstruction the entire length of the artery with all of its side branches must be circumferentially dissected and controlled from the external iliac down through the femoral bifurcation. Any unidentified side branches will lead to troublesome back-bleeding during the reconstruction phase of the operation if not properly controlled externally. The extent of SFA and profunda exposure will be dictated by the burden of disease and which is the more critical outflow vessel in a given scenario. As the proximal exposure of the CFA progresses it is helpful to elevate the inguinal ligament off of the vessel to gain access to the external iliac system. At times, a partial limited division of the inguinal ligament can be performed if more proximal exposure is needed. As in any arterial exposure the safest place to proceed is along the anterior wall of the vessel. Crossing anterior to the CFA as it transitions to the external iliac artery beneath the inguinal ligament will be the deep circumflex iliac crossing vein in most people (Fig. 23.3). Injury to this vein makes for troublesome bleeding that may be difficult to control. The confluence of the two branches (deep
circumflex iliac and inferior epigastric) may be directly anterior to the arterial wall. Ligating the two branches separately allows for more secure division. We find that standard ligation with additional clip placement behind the ties nearly guarantees adequate control and allows for safe division (Fig. 23.3, inset). At this level the medially oriented deep circumflex iliac artery branch will be identified and controlled with a vessel loop. Circumferential control of the CFA at this level is necessary to allow for adequate clamp placement. Occasionally, a larger vessel loop or umbilical tape can be indirectly passed above this branch to facilitate clamping.
circumflex iliac and inferior epigastric) may be directly anterior to the arterial wall. Ligating the two branches separately allows for more secure division. We find that standard ligation with additional clip placement behind the ties nearly guarantees adequate control and allows for safe division (Fig. 23.3, inset). At this level the medially oriented deep circumflex iliac artery branch will be identified and controlled with a vessel loop. Circumferential control of the CFA at this level is necessary to allow for adequate clamp placement. Occasionally, a larger vessel loop or umbilical tape can be indirectly passed above this branch to facilitate clamping.
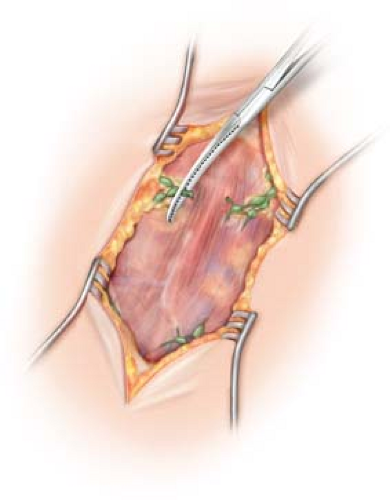 Figure 23.2 Fastidious clamping, ligation, and division of inguinal fat and lymphatic tissue will minimize the risk of postoperative lymphatic complications. |
Distally, the dissection will be carried to the extent necessary to allow for reconstruction. Many patients will have a chronically occluded SFA and therefore no clamping zone needs to be established; however, regardless of patency, several centimeters of the SFA will need to be mobilized to allow for proper dissection of the profunda laterally. If the SFA is not occluded but severely diseased, one should dissect it out for several centimeters to identify a reasonably soft zone for clamping, if it exists, otherwise, occasionally endoluminal balloon control may become necessary.
The PFA is an extremely fragile vessel, akin to the subclavian and axillary arteries. Utmost care should be taken when handling it and dissecting it as injury to it may be difficult to control. The extent of dissection required on the profunda will be dictated by preoperative imaging as well as the feel of the vessel at the time of surgery. If it is widely patent on angiography and soft, one need not extensively expose the profunda and its branches as focal clamping or control of the origin of the vessel should suffice. If the profunda is widely patent on imaging, yet has a porcelain-like calcific wall, the patient will not likely benefit from EA; however, one must dissect it distally enough to find a reasonable clamp zone or be prepared for balloon control, as clamping the diseased vessel wall will often prove problematic. Typically, as the profunda arborizes, one will find that the large side branches are often soft and controllable. Many patients may have focal orificial profunda disease in which case an eversion-type EA may be planned, and again an extensive profunda exposure may not be necessary in these instances. For the patients with extensive profunda occlusive disease on imaging and by palpation in the operating room, attempts at orificial EA will not likely serve the patient well as more often than not the nonvisualized endpoint may leave a large flap and lead to occlusion. In these instances we strongly advocate completely delineating the profunda and its branches until a soft clampable outflow vessel is encountered. In some patients this may be an extremely extensive exposure. It is unlikely that a surgeon will ever regret having
too much profunda exposure. It is not uncommon however to regret not having enough profunda exposure at the time of EA, which means further dissection must be carried out with an open vessel and clamp in situ, which is suboptimal.
too much profunda exposure. It is not uncommon however to regret not having enough profunda exposure at the time of EA, which means further dissection must be carried out with an open vessel and clamp in situ, which is suboptimal.
 Get Clinical Tree app for offline access 
|