The investigators describe idiopathic restrictive cardiomyopathy in a 50-year-old woman. Eleven other family members had cerebrovascular accidents, arrhythmias, and/or heart failure requiring cardiac transplantation. The patient developed dyspnea and palpitations at 19 years of age, when echocardiography demonstrated normal left ventricular systolic function, biatrial enlargement, and a restrictive Doppler mitral inflow pattern; restrictive hemodynamics were confirmed on cardiac catheterization. She was managed for many years with diuretics, antiarrhythmic agents, and anticoagulation and underwent cardioversion for recurrent atrial fibrillation. In conclusion, the patient ultimately underwent cardiac transplantation.
Idiopathic restrictive cardiomyopathy (IRC) is an uncommon cardiac disorder characterized by left ventricular (LV) diastolic dysfunction with normal LV systolic function and wall thickness and symptoms of heart failure. We report the largest pedigree to date, a family in which 3 generations and ≥12 members had signs and symptoms consistent with restrictive cardiomyopathy.
Case Descriptions
The index patient, a woman, initially presented at 19 years of age with occasional palpitations, dyspnea, abdominal bloating, and limited exercise tolerance. Twelve family members in 3 generations had cardiac dysfunction, and 3 had strokes ( Figure 1 ).
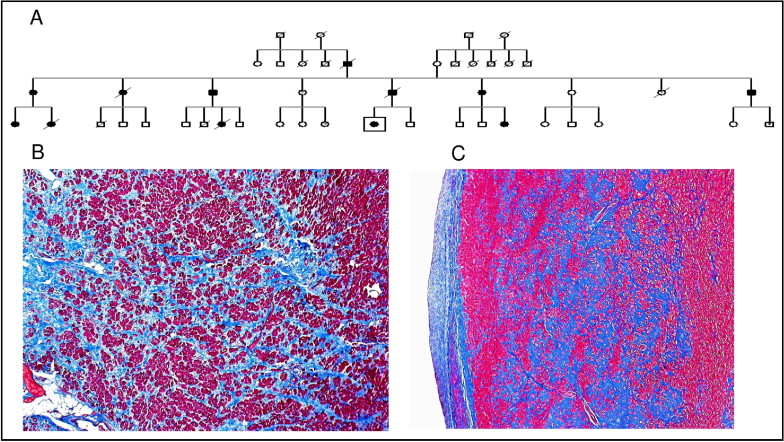
The index patient in generation II had arrhythmias and multiple cerebrovascular accidents and died at 65 years of age. Generation III had 6 patients consistent with IRC. The father (III-5) had heart failure, atrial fibrillation and ascites. At his death at 68 years of age, his heart demonstrated markedly dilated atria and an organizing thrombus in the right atrial appendage, features consistent with IRC ( Figure 1 ).
In the patient’s generation (generation IV), 1 cousin required cardiac transplantation, another had multiple strokes and died, a third died at 16 years of age from advanced IRC, and a fourth required a defibrillator and heart failure therapy. The family shows father-to-daughter transmission with no skipped generations.
The index patient, when seen at 50 years of age, had congestive heart failure, low blood pressure, jugular venous distention, and an S3 gallop. Chest x-ray showed pulmonary vascular congestion. Electrocardiography intermittently exhibited atrial flutter. Echocardiography showed normal LV size and systolic function, an LV ejection fraction of 60%, marked biatrial enlargement, a restrictive Doppler mitral inflow pattern with a reduced mitral valve deceleration time, and high E/E′ ratio consistent with increased left atrial pressure.
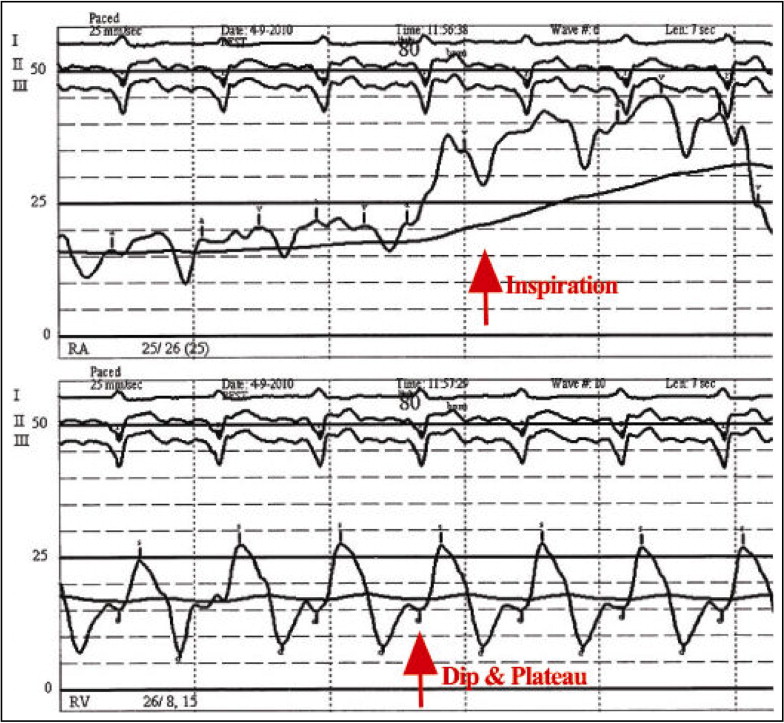
After medical management for 32 years with high-dose diuretics, digoxin, and sotalol for atrial fibrillation and flutter, and anticoagulation, the patient’s exercise tolerance decreased and her heart failure worsened. Right-sided cardiac catheterization revealed a low cardiac output of 2.2 L/min and elevated filling pressures ( Figure 2 ) with a Kussmaul’s sign on the right atrial (RA) pressure tracing and a diastolic dip and plateau wave form on the right ventricular (RV) pressure tracing. At 51 years of age, the patient underwent cardiac transplantation. The explanted heart demonstrated subendocardial interstitial fibrosis, with no evidence of infiltrative disease, ischemic changes, or vasculitis( Figure 1 ).