(1)
Department of Neuroscience, University of Turin Ospedale Molinette, Turin, Italy
Abstract
The vertebral artery (VA) originates from the subclavian artery. It runs posterosuperiorly behind the anterior scalene muscle, commonly reaching the foramen of the transverse process of the sixth cervical vertebra. This first segment of the VA has been called Vl (Huber 1979; Osborn 1999). The artery can enter the foramen at the inferior or superior level (Huber 1979). It runs further vertically through the foramina of the transverse processes from C6 to C2 (the V2 segment), surrounded by the venous plexus. The spinal nerves lie behind. Between the foramina of C2 and C1, the artery curves laterally and somewhat anteriorly. Exiting from C1 begins the V3 segment, which curves backward, running in the sulcus of the posterior arch of C1; it then forms a second upward and forward curve and reaches the foramen magnum, where the artery penetrates the dura and forms its last segment (V4). It is conceivable that these curves protect the VA, allowing it to accommodate more easily movement in the atlantooccipital region (Fig. 6.1).
6.1 Extracranial Sector
The vertebral artery (VA) originates from the subclavian artery. It runs posterosuperiorly behind the anterior scalene muscle, commonly reaching the foramen of the transverse process of the sixth cervical vertebra. This first segment of the VA has been called Vl (Huber 1979; Osborn 1999). The artery can enter the foramen at the inferior or superior level (Huber 1979). It runs vertically (V2 segment) through the foramina of the transverse processes from C6 to C2, surrounded by the venous plexus. The spinal nerves lie behind. Between the foramina of C2 and C1, the artery curves laterally and somewhat anteriorly. Exiting from C1 begins the V3 segment, which curves backward, running in the sulcus of the posterior arch of C1; it then forms a second upward and forward curve and reaches the foramen magnum, where the artery penetrates the dura and forms its last segment (V4). It is conceivable that these curves protect the VA, allowing it to accommodate more easily movement in the atlantooccipital region (Fig. 6.1).
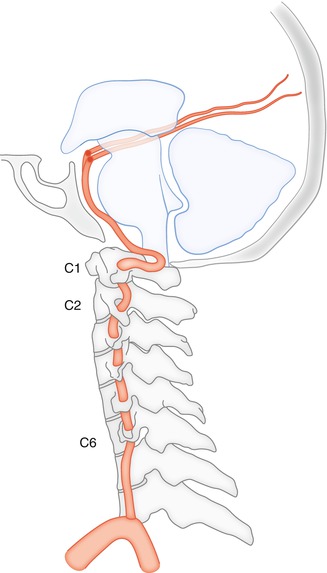
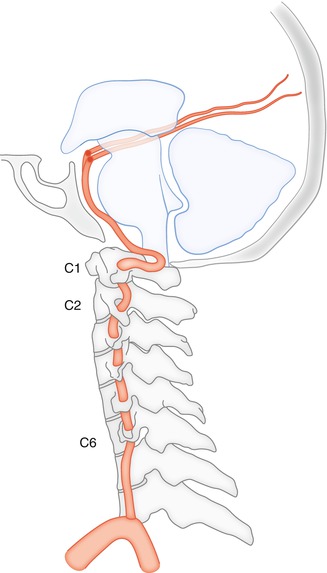
Fig. 6.1
Extracranial course of the vertebral artery arising from the subclavian artery and entering the intracranial cavity at the foramen magnum
6.1.1 Branches
Muscular spinal branches have possible anastomoses with branches of the external carotid artery (Figs. 6.2 and 6.7a) and with the cervical ascending artery (Fig. 15.18).

Fig. 6.2
(a) AP angiogram of the right vertebral artery showing its extracranial course. Radiculomedullary artery (arrowhead) continuing in the ascending and descending segments (arrow) of the anterior spinal artery. (b) Vertebral angiogram, lateral view: hypoplastic vertebral artery (VA) ending in the posterior inferior cerebellar artery. Hypoglossal branch of the ascending pharyngeal artery (arrow with dot) anastomosing with the ascending radiculomeningeal branch of the VA (arrowhead), contributing to form the so-called odontoid arch. Posteriorly runs the anterior spinal artery (ASA; double arrow). Muscular branch at the C1–C2 level, which presents possible anastomosis with the corresponding branches of the occipital and ascending pharyngeal arteries. (c) Another example of a connection between the hypoglossal branch of the ascending pharyngeal artery (arrow with dot) and ascending radiculomeningeal branch of the VA (arrows)
Spinal branches include branches for the dura and bone structures, and radicular branches supply the nerves. After supplying the nerves, other radicular branches (radiculomedullary arteries) reach the spinal cord, continuing in the anterior spinal artery (ASA) and posterior spinal artery (PSA). An anterior radiculomedullary artery, supplying the ASA, is frequently visible on the VA angiogram at the C4–C6 level. The ascending and descending segments are easily recognizable, anastomosing cranially with the descending ASA, arising from the intracranial VA, and caudally with the segment arising from the radiculomedullary artery of the intercostal arteries (Fig. 6.2). Alternatively, the radiculomedullary artery can sometimes arise from the ascending cervical artery. The PSAs are seldom identifiable on the normal vertebral angiogram.
Meningeal branches of the distal extracranial VA are as follows:
On the vertebral angiogram, a small branch is frequently visible anterior and lateral to the ASA on the lateral and AP views, respectively. This artery, first described by Greitz and Lauren (1968), has been called the anterior meningeal artery. Further studies (Lasjaunias et al. 1978a) have demonstrated that this artery is a radiculomeningeal branch which arises from the VA at the level of the third vertebral body. The anterior meningeal artery runs cranially in the spinal canal and anastomoses with the contralateral branch at the level of the dorsal surface of the odontoid process. The anterior meningeal artery is connected further with the hypoglossal artery, which is a branch of the ascending pharyngeal artery; this passes the hypoglossal foramen and enters the spinal canal. This connection is also called the odontoid arch (Figs. 6.2, 6.3, 6.9, 3.8, 3.29, 3.30, 15.19, and 15.20) See also Sect. 3.4.
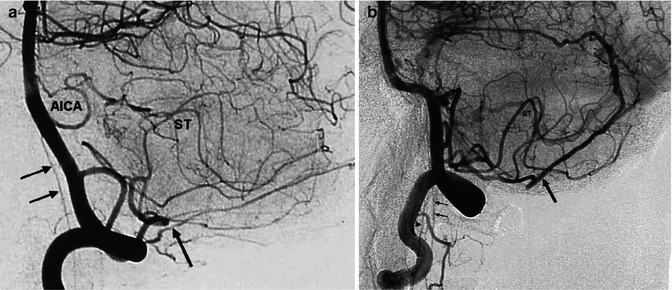
Fig. 6.3
Vertebral angiogram, lateral view. (a) Falx cerebelli artery FCA (arrow); ASA (double arrow). Tortuous first segments of the PICA, typical pattern of the supratonsillar segment (ST), AICA. (b) FCA (arrow) is dilated, supplying a dural arteriovenous fistula. The FCA continues in the meningeal branch along the straight sinus. ASA (double arrow). Ascending meningeal branch of the VA (arrowhead)
The falx cerebelli and posterior meningeal arteries originate from the extracranial, sometimes from the intracranial, VA. They may also originate from the posterior inferior cerebellar, occipital, or ascending pharyngeal arteries. There is a balance between these arteries, so one can predominate in supplying the dura of the posterior fossa. The falx cerebelli artery (FCA) runs close to the falx cerebelli and continues in the meningeal branch along the straight sinus; it anastomoses superiorly with the paramedian branches of the middle meningeal artery (see Chapter 3.7.11). On the lateral angiogram, the FCA runs slightly away from the inner table of the skull, and it is near the midline in the AP view (Figs. 6.3, 13.9, and 13.13). The posterior meningeal artery runs on the dura covering the cerebellar hemispheres, so it has a more lateral course in the AP view; it runs close to the inner table of the skull on the lateral angiogram (Figs. 13.1 and 15.22).
6.2 Intracranial Sector
At the level of the foramen magnum, the VA penetrates the dura, where it is sometimes identifiable owing to a small change in the caliber. The artery runs in the subarachnoid space ventrolateral to the medulla oblongata and joins the contralateral artery at the bulbopontine junction to form the basilar artery. The basilar artery runs on the ventral surface of the pons in the median–paramedian position; it sometimes adopts a tortuous course and displays a lateral extension toward the cerebellopontine angle (Fig. 6.12). In the interpeduncular fossa under the floor of the third ventricle, the basilar artery divides into the two posterior cerebral arteries (PCAs). The point of the division can be more caudally located with a cranial course of the PCAs (Fig. 7.9c). The basilar artery may be elongated, especially in hypertensive and atherosclerotic patients, and it bulges to the floor of the III ventricle. In such cases, the PCAs have first a caudally directed course before they encircle the midbrain. Many arteries arise from the intracranial sector of the vertebrobasilar system (Fig. 6.4a, b). In this chapter we will consider the branches for the medulla and pons and cerebellum. The branches supplying midbrain, thalamus, and the temporo-occipital area are described in the section of the PCA (Chap. 7).
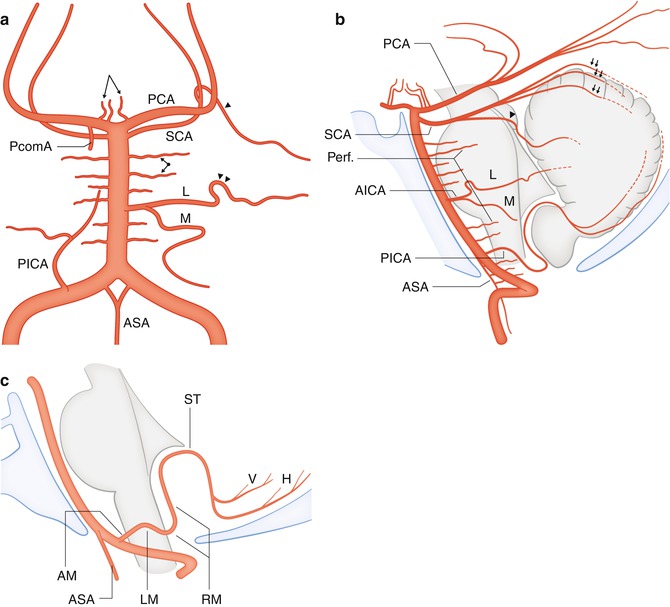
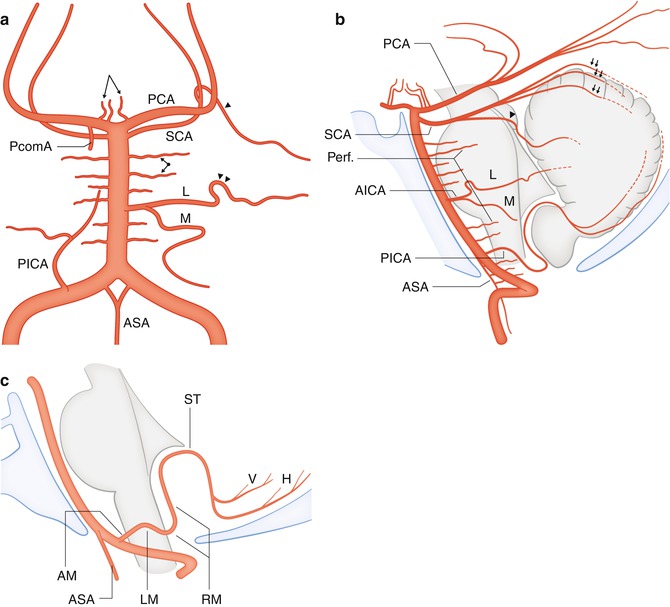
Fig. 6.4
(a) Drawing showing the intracranial vertebrobasilar sector in the AP projection. The two vertebral arteries unite in the basilar artery. Anterior spinal artery (ASA). Posterior inferior cerebellar artery (PICA) replacing on the right the absent AICA. Lateral branch (L) and medial branch (M) of the AICA replacing on the left the absent PICA. Loop of the lateral branch in front of the meatus acusticus (arrows head). Superior cerebellar artery (SCA). Marginal branch (arrow head). Latero-pontine arteries (arrows with angle and dot). Posterior cerebral artery (PCA), Posterior communicating artery (PcomA). Posterior thalamoperforating branches (arrows with angle). (b) Lateral view. Perforators for brainstem (arrow dividing in two branches). SCA with its vermian and hemispheric branches (arrows). Marginal branch (arrow head). Pial anastomoses between PICA, AICA, and SCA (——-). Other indications as in (a). (c) Course of the PICA as seen on the lateral angiogram. Anterior medullary segment (AM), lateral medullary segment (LM), retromedullary segment (RM), supratonsillar segment (ST), vermian (V), hemispheric branches (H), and Anterior spinal artery (ASA)
6.2.1 Branches of the VA
6.2.1.1 Perforators of the VA
Small arteries arise from the posterior surface of the VA (Duvernoy 1999) running on the anterior surface of the medulla (anterior branches) especially in its superior part. Other branches of the VA extend to the lateral surface of the medulla (lateral branches) in its inferior and middle portion. Some anastomoses, irregular in number, are present between these superficial vessels especially laterally on the surface of the olive. From the superficial arteries arise perforators not visible on the angiogram supplying the medulla.
The perforating branches are basically end arteries without possibility of a collateral circulation. This is a common feature for all perforators supplying the brainstem which are progressively described in the next chapters.
6.2.1.2 Posterior Inferior Cerebellar Artery
The posterior inferior cerebellar artery (PICA) arises bilaterally from the first intradural segment of the VA and sometimes from its extradural segment. It runs anterolaterally to the medulla, reaching its posterior border after a variable course. During its course, the PICA has a close relationship with cranial nerves IX, X, XI, and XII. Further, it takes an upward course along the anterior surface of the tonsilla, which it surrounds superiorly and forms a typical loop on the angiogram that is commonly recognizable. Small branches for the choroid plexus of the IV ventricle arise at this level. The PICA further divides into the vermian and hemispheric branches (Fig. 6.4a, b, c).
Vascular Territories. The PICA gives off perforators arising from his LM segment for the lateral medulla. There is a balance between the branches of the PICA and those of the VA which commonly predominate (Duvernoy 1999). Furthermore, the PICA supplies the posterior medulla together with the PSA, through perforators arising from its RM segment. The distal branches supply the tonsilla, the inferior vermis, and inferior surface of the cerebellar hemisphere.
Variants. The PICA can be very large and also partially supply the contralateral hemisphere. Sometimes, it is hypoplastic or absent and is replaced by a large anterior inferior cerebellar artery (AICA). For other variants see Sects. 2.5 and 6.2.4.
On the angiogram, the PICA and its segments can be better studied in the lateral view. The first segments (anterior medullary and lateral medullary) can be characterized by a tortuous course. It is always easy to identify the retromedullary and supratonsillar segments, which surround the tonsilla and the inferior vermian and hemispheric branches. In the AP view, the different segments cannot easily be separately distinguished (Figs. 6.2, 6.3, 6.5, 6.6, 6.7, 6.8, 6.9, 6.10, and 6.11).
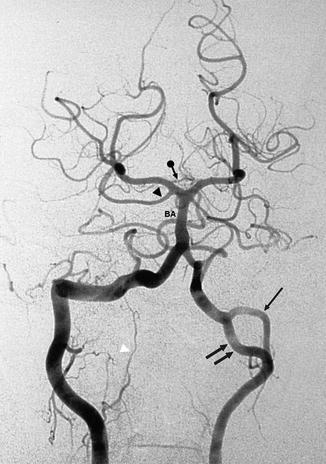
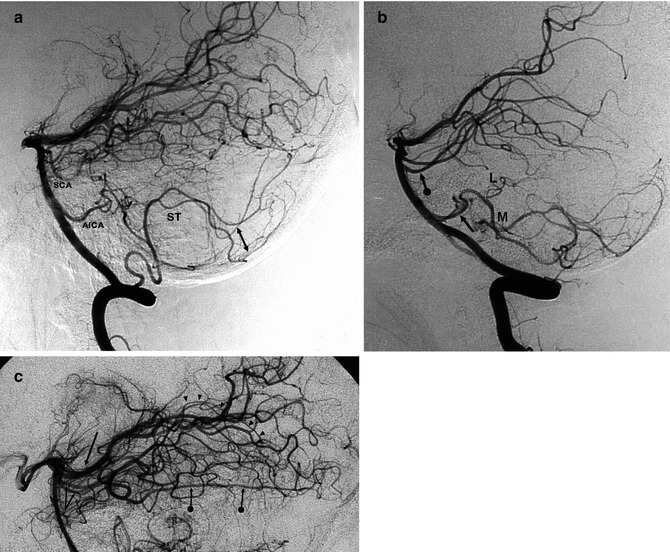
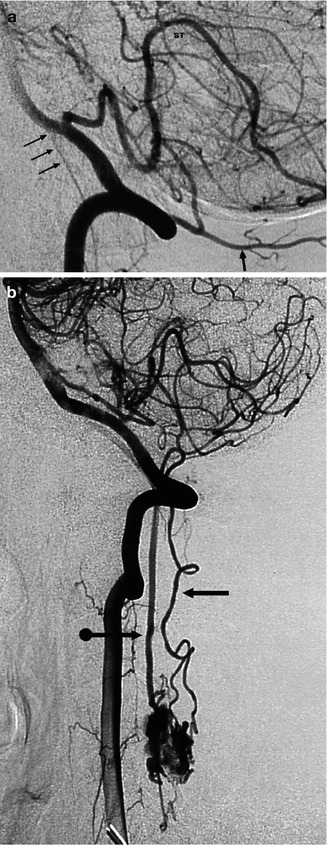
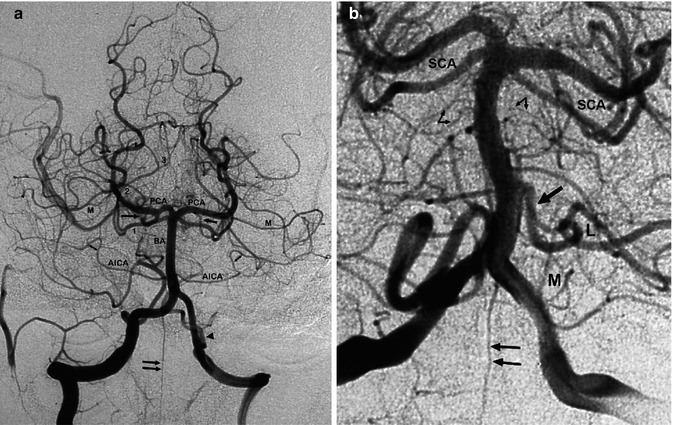
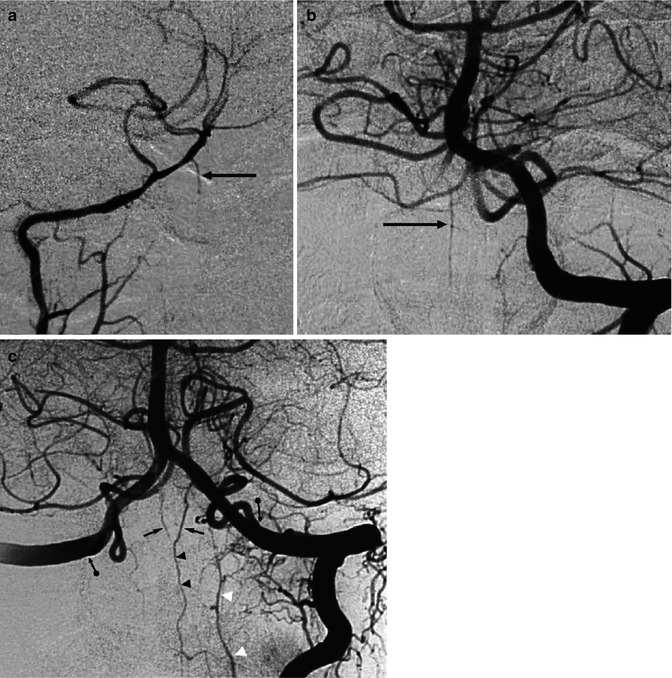
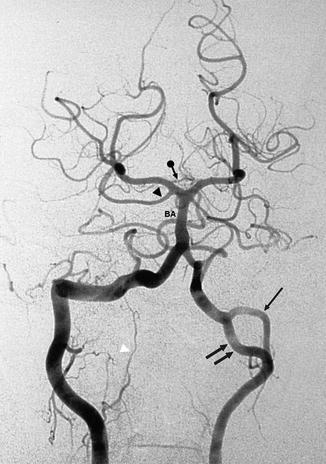
Fig. 6.5
Vertebral angiogram, AP view. Asymmetric lumen of the vertebral arteries. There is duplication of the left vertebral artery. The anomalous vessel (double arrow) is larger than the true artery (arrow). Normal basilar artery (BA) continuing in both PCAs. From the right P1 arises a large posterior thalamoperforating branch, dividing distally into small branches (arrow with dot). The right superior cerebellar artery (SCA) arises from the right P1 (arrowhead). Presence on the right of a radiculomeningeal branch (white arrowhead)
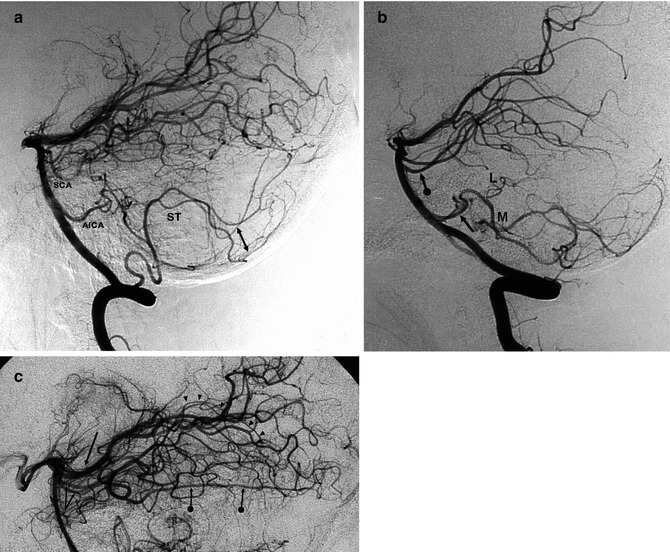
Fig. 6.6
(a) Lateral vertebral angiogram. Tortuous first segments of the PICA. Typical supratonsillar loop (ST). Vermian and hemispheric branches (bidirectional arrow). AICA, SCA. (b) Lateral vertebral angiogram. The PICA is absent bilaterally. It is replaced by two well-developed AICAs (arrow). In this case the lateral branch (L) is very small, while the medial (M) is well developed. SCA (arrow with dot). (c) Lateral vertebral angiogram (detail), showing the SCAs (arrow with angle). Cerebellar branches (arrow heads). Well-developed lateral hemispheric branch (arrows with dot). PCA (arrow)
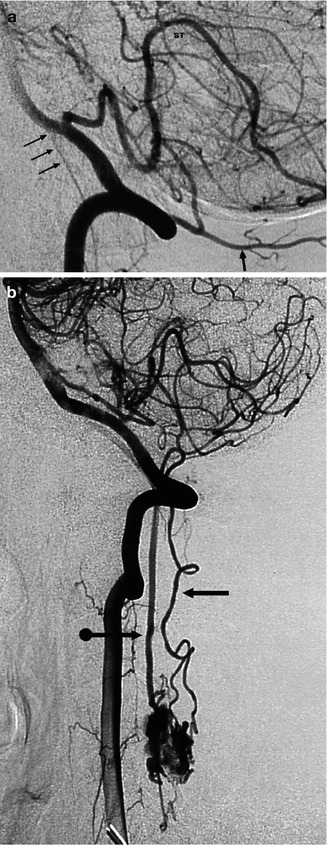
Fig. 6.7
(a) Lateral vertebral angiogram (detail). PICA with its typical supratonsillar loop (ST). ASA (arrows). Muscular branch at the level of C1, which can potentially anastomose with the corresponding branch of the occipital artery (arrow). (b) Patient with arteriovenous malformation involving the cervical spinal cord. Lateral vertebral angiogram showing the supply by a very dilated ASA (arrow with dot) and PSA (arrow)
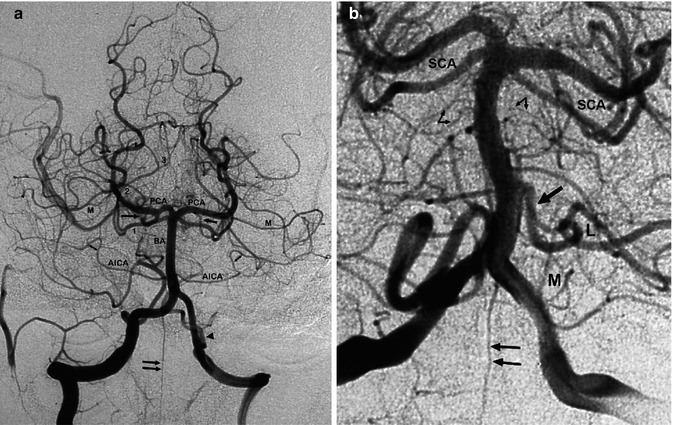
Fig. 6.8
Vertebral angiogram, AP view. (a) Asymmetric vertebral artery. Basilar artery (BA). Both PICAs are well developed. That on the left probably has an extracranial origin (arrowhead). Unilateral origin of ASA (double arrow). Bilateral AICA. Note the loop in front of the internal meatus acusticus (bidirectional arrows). The numbers 1, 2, and 3 indicate, respectively, the pontine, midbrain, and quadrigeminal segments of the SCA. The latter continues in its terminal vermian branches. Marginal branch (M) of the SCA. From both PCA, retrograde injection of the posterior communicating artery (arrow) is particularly well developed on the right. This allows identification of the P1 segment of the posterior cerebral artery (PCA). On the right, there is an anastomosis between a branch of the vertebral artery and the occipital artery. (b) Bilateral voluminous vertebral artery. On the right, a well-developed PICA arises from the VA. On the left, a voluminous AICA replaces the absent PICA (arrow). Lateral branch (L), medial branch (M), and superior cerebellar artery (SCA). Lateral pontine arteries (arrow with angle) take their origin from the basilar artery (arrow). Unilateral ASA (double arrow)
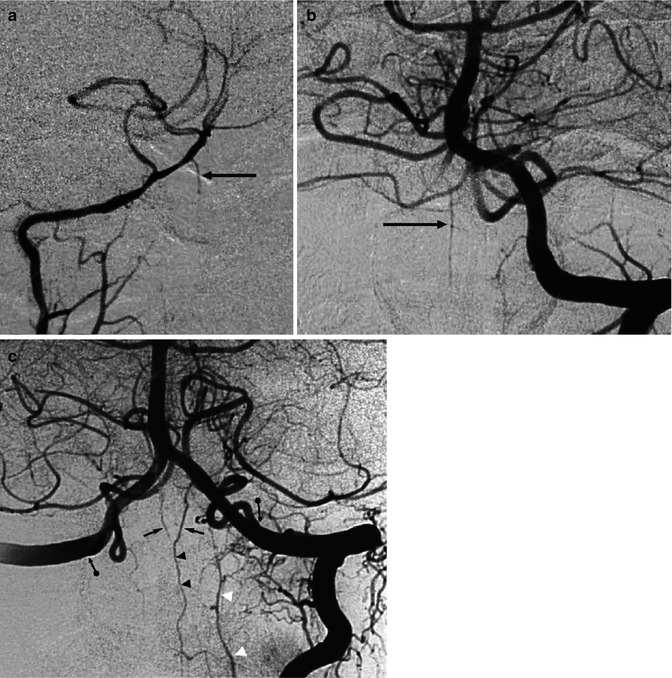
Fig. 6.9




Left and right vertebral angiogram in the same patient. On the angiogram of the well-developed left vertebral artery (b), there is a partial injection of the hypoplastic right vertebral artery injected also selectively (a). Unilateral origin of the ASA (arrow) from the hypoplastic right vertebral artery. Study in a different patient (c). Left vertebral angiogram with retrograde injection of the contralateral vertebral artery. ASA (arrowhead) with its bilateral contribution (arrow) deriving from the vertebral arteries. Radiculomeningeal artery (white arrowhead) arising at the C3 level of VA. Probable bilateral extradural origin of the PICA (arrow with dot)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


