Negative T waves (NTWs) in right precordial leads (V 1 to V 3 ) may be observed on the electrocardiogram (ECG) of healthy subjects but can also represent the hallmark of an underlying arrhythmogenic right ventricular cardiomyopathy (ARVC). It has been a consistent observation that NTWs usually become upright with exercise in healthy subjects without underlying heart disease. No systematic study has evaluated exercise-induced changes of NTWs in ARVC. We assessed the prevalence and relation to the clinical phenotype of exercise-induced right precordial NTWs changes in 35 patients with ARVC (19 men, mean age 22.2 ± 6.2 years). Forty-one healthy subjects with right precordial NTWs served as controls. At peak of exercise (mean power 149 ± 43 W, mean heart rate 83.6 ± 12.6% of target), NTWs persisted in 3 patients with ARVC (9%), completely normalized in 12 (34%), and partially reverted in 20 (57%). Patients with ARVC with or without NTWs normalization showed a similar clinical phenotype. The overall prevalence of right precordial T waves changes during exercise (normalization plus partial reversal) did not differ between patients with ARVC and controls (92% vs 88%, p = 1.0), whereas there was a statistically nonsignificant trend toward a greater prevalence of complete normalization in controls (56% vs 34%, p = 0.06). In conclusion, our study demonstrated that right precordial NTWs partially or completely revert with exercise in most patients with ARVC, and NTWs normalization is unrelated to the clinical phenotype. Exercise-induced NTWs changes are inaccurate in differentiating between ARVC patients and benign repolarization abnormalities.
Negative T-waves (NTWs) on resting electrocardiogram (ECG) can become positive during exercise and return to baseline in the postexercise phase. In patients with previous myocardial infarction, this phenomenon is called “pseudonormalization” and reflects residual perfusion and myocardial viability of the infarct area. Exercise-induced normalization of NTWs also occurs in conditions other than coronary heart disease. It has been a consistent observation that NTWs usually become upright with exercise in healthy subjects without underlying heart disease. NTWs in right precordial (V 1 to V 2 /V 3 ) leads are also observed in up to 80% of patients with arrhythmogenic right ventricular cardiomyopathy (ARVC), an inherited cardiomyopathy characterized pathologically by myocardial fibrofatty replacement and clinically by electrical instability leading to ventricular arrhythmias and sudden death. The current perspective is that, at variance with healthy subjects, right precordial NTWs persist with exercise in ARVC patients. However, this view is not supported by systematic scientific data. The aim of this study was to systematically assess the prevalence and correlation with the disease phenotype of right precordial NTW changes during exercise testing in a consecutive series of patients with ARVC and in a group of age- and sex-matched healthy subjects.
Methods
The study sample included 35 consecutive patients with ARVC undergoing exercise test at the time of first clinical evaluation during the period 2010 to 2012. Patients were enrolled in the study if they (1) fulfilled the criteria (2 major criteria, 1 major criteria plus 2 minor criteria, or 4 minor criteria) for definite diagnosis of ARVC according to the 2010 Revised Task Force Criteria, (2) showed NTWs in right precordial leads (V 1 to V 3 ), and (3) were not on β blockers or antiarrhythmic drugs at the time of exercise testing. A group of 41 healthy subjects, with age and gender comparable to the ARVC study patients served as controls. They exhibited right precordial NTWs with no ST segment elevation on ECG obtained at their first preparticipation cardiovascular evaluation before embarking in competitive sport programs. All patients and controls underwent the same comprehensive clinical evaluation including family and personal history, electrocardiography, signal-averaged electrocardiography, 24-hour ECG Holter monitoring, exercise testing, echocardiogram, and cardiac magnetic resonance. Technical equipment, protocols, and reference values have been reported in detail elsewhere.
Maximal bicycle exercise testing was performed at the time of first clinical evaluation according to a protocol of 25 to 50 W increments every 3 minutes. Twelve-lead ECG, heart rate, and blood pressure were recorded at baseline, during the third minute of each exercise stage, at peak exercise, and every 3 minutes into recovery. Criteria for interrupting the test were target heart rate (220 minus age), complex ventricular arrhythmias, hypotension, symptoms, or exhaustion. The ECG patterns of right precordial NTWs in response to exercise were classified as persistence of T-wave inversion that is no or minor (<50%) changes of NTW amplitude; T-wave normalization that is NTW becoming upright with exercise; and partial reversal when there was a positive increase in the T-wave amplitude ≥50% in ≥2 contiguous leads. ECG interpretation was performed independently by 2 observers (AZ, ME), in case of disagreement a third observer (DC) was consulted.
Categorical differences among groups were evaluated by the chi-square test or Fisher’s exact test as appropriate. Continuous variables were expressed as mean ± SD and compared with Student’s t test or with the rank sum test as appropriate. Normal distribution of continuous variables was assessed by the Kolmogorov-Smirnov test. A value of p <0.05 was considered significant. Statistics were analyzed with SPSS version 17 (SPSS Inc., Chicago, Illinois).
Results
The study population included 35 patients with ARVC (19 men, mean age 22.2 ± 6.2 years), whose clinical characteristics are listed in Table 1 , and 41 controls (26 men, mean age 19.5 ± 9.2 years) who were asymptomatic, had a negative family history, and showed no evidence of structural heart disease, late potentials, or ventricular arrhythmias.
| Variable | Overall, n = 35 | Normalization | p | |
|---|---|---|---|---|
| Yes, n = 12 | No, n = 23 | |||
| Men | 19 | 6 | 13 | 0.71 |
| Age (yrs) | 22.2 ± 6.2 | 20.0 ± 10.3 | 28.7 ± 8.4 | 0.03 |
| Family history | ||||
| Sudden death | 4 | 1 | 3 | 1.0 |
| ARVC | 9 | 5 | 4 | 0.22 |
| Palpitations | 19 | 6 | 13 | 0.74 |
| Chest pain | 4 | 1 | 3 | 1.0 |
| Syncope | 8 | 1 | 7 | 0.22 |
| Sustained ventricular tachycardia | 7 | 3 | 4 | 0.67 |
| Cardiac arrest | 1 | 1 | 0 | 0.34 |
| Electrocardiographic findings | ||||
| Epsilon waves | 10 | 2 | 8 | 0.43 |
| Low QRS voltage in limb leads | 11 | 2 | 9 | 0.26 |
| S wave >50 ms in V 1 –V 3 | 15 | 3 | 12 | 0.17 |
| NTW beyond V 3 | 4 | 2 | 2 | 0.64 |
| Maximal NTW amplitude (mV) | 0.4 ± 0.1 | 0.4 ± 0.1 | 0.4 ± 0.1 | 0.73 |
| Late potentials on SAECG | 21 | 5 | 16 | 0.11 |
| 24-hour Holter monitoring | ||||
| ≥500 premature ventricular beats/24-h | 27 | 10 | 17 | 0.69 |
| Nonsustained ventricular tachycardia | 21 | 9 | 13 | 0.29 |
| Echocardiographic findings | ||||
| RV end-diastolic area (cm 2 ) | 28 ± 6 | 28 ± 6 | 28 ± 7 | 0.80 |
| RV fractional area change (%) | 35 ± 9 | 33 ± 7 | 37 ± 9 | 0.33 |
| RV regional wall motion abnormalities | 31 | 10 | 21 | 0.59 |
| LV end-diastolic volume (ml/mq) | 62 ± 10 | 59 ± 9 | 63 ± 11 | 0.31 |
| LV ejection fraction (%) | 57 ± 7 | 58 ± 5 | 57 ± 8 | 0.75 |
| LV regional wall motion abnormalities | 7 | 4 | 3 | 0.20 |
At peak of exercise, patients and controls reached similar power (162 ± 43 vs 158 ± 24 W), heart rate (169 ± 24 vs 177 ± 15 beats/min, corresponding to 84 ± 13% vs 88 ± 7% of target heart rate) and double product (27,643 ± 6,361 vs 28,314 ± 4,207 beats/min × mm Hg). Reasons for interruption were target heart rate in 20 patients (57%) and 26 controls (63%) and physical exhaustion in 15 patients (43%) and 15 controls (37%). One patient with ARVC showed significant ST segment depression at peak of exercise and underwent myocardial perfusion scintigraphy that excluded an underlying myocardial ischemia. Ventricular arrhythmias were induced or increased with exercise in 10 patients (29%) and reduced or suppressed in 15 (42%); in the remaining 10 patients (29%) no arrhythmias were observed thorough the exercise test. No controls showed significant ST segment depression or ventricular arrhythmias during exercise.
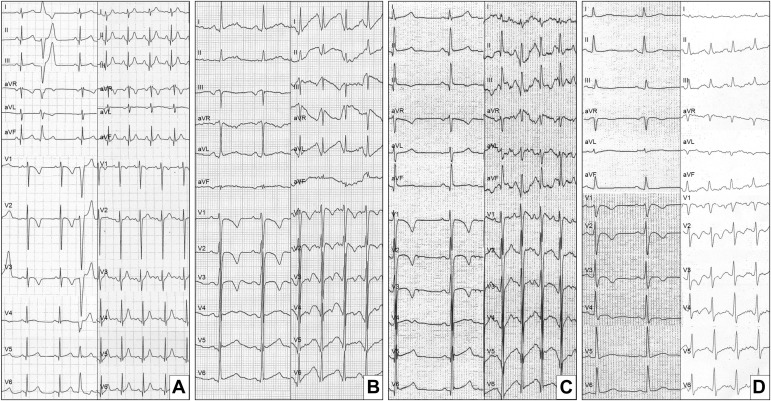
Among patients with ARVC, the deepest NTW in the right precordial leads on resting ECG had a mean amplitude of 0.4 ± 0.1 mV and was observed more often in lead V 2 (27/35, 77%). Right precordial NTWs persisted with exercise in 3 patients (9%), normalized in 12 (34%), and partially reverted in 20 (57%). T-waves became positive or less negative at a mean power of 110 ± 14 W and gradually returned to baseline during the postexercise phase. Representative cases of response to exercise of right precordial repolarization abnormalities and ventricular arrhythmias are shown in Figure 1 . Persistence of right precordial NTWs with exercise was observed in 5 controls (12%), T-waves normalization in 23 (56%), and partial reversal in 13 (32%). The overall prevalence of right precordial T-wave changes with exercise (normalization plus partial reversal) was similar in patients with ARVC and controls (92% vs 88%, p = 1.00), whereas when we compared only complete normalization, there was a statistically nonsignificant trend toward a higher prevalence in controls (56% vs 34%, p = 0.06).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


