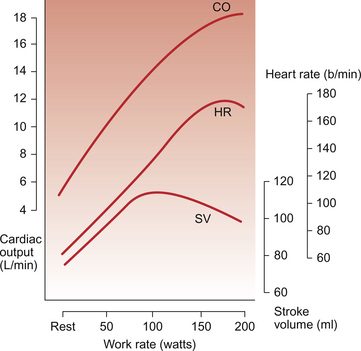
13 • an increase in stroke volume of the heart • a modest increase in mean arterial blood pressure • changes in the distribution of blood flow to support exercising muscles. Increased extraction of oxygen from arterial blood (see Chapter 1) in exercising muscles will also contribute to the increase in oxygen delivery. Identification of the key physiological events at the initiation of dynamic exercise has long been contentious and is still the subject of debate, despite the existence of theoretical models for more than 100 years. Reflex control of the circulation normally relies on sensory information provided from baroreceptors and chemoreceptors (see Chapter 10). These same reflexes function during ongoing exercise, but mean arterial BP, Po2 and Pco2 do not change significantly at the start of exercise. The changes in cardiac function during exercise therefore occur too rapidly to be explained by activation of baroreceptor and chemoreceptor reflexes. The most popular hypothesis used to explain the initiation of cardiovascular responses to exercise is the ‘feedforward’ or ‘central command’ theory. This suggests that the areas of the brain which drive muscle contraction at the start of exercise also produce the drive to increase heart rate and lung ventilation. This theory was first proposed in 1913 and numerous modifications have been suggested since then. The parts of the brain particularly involved in ‘central command’ are thought to be the motor cortex and the hypothalamus. The cerebellum, which has the major role in the coordination of muscle movement, is also involved in coordinating the cardiovascular response to exercise. Areas within the medulla control the sympathetic and parasympathetic nerves which normally regulate heart rate and cardiac contractility as part of the baroreceptor reflex (see Chapter 10). At the start of exercise, the influence of central command over the medullary centres is to decrease vagal tone and to increase sympathetic drive, thus increasing heart rate. Part of this response may be an alteration in the operation of the baroreceptor reflex (see Chapter 10). Under normal conditions, this reflex keeps blood pressure relatively constant at a ‘set point’. During exercise, central command induced changes in this set point have the same effect as a blood pressure which is too low, hence leading to an increase in heart rate. Reflex activation of the sympathetic nervous system also leads to peripheral vasoconstriction (see Chapter 9). This occurs particularly in the splanchnic and kidney circulations and in the vessels of non-contracting muscles. This helps to divert blood flow to active muscles. The central command mechanism is probably complemented by feedback from metabolite concentrations, particularly [K+], detected by chemoreceptors in contracting muscles and information from mechanoreceptors within moving joints and muscles. Cardiac output is a function of both heart rate and stroke volume. Figure 13.1 shows the effect of different intensities of dynamic exercise on cardiac output, heart rate and stroke volume in healthy young individuals. Intense exercise in trained athletes may require a fivefold increase in cardiac output. Changes in stroke volume reach maximum levels at a moderate exercise intensity (see below). Beyond this level, further increases in cardiac output are provided solely by increases in heart rate. Increased oxygen delivery to tissues is also achieved by increasing the extraction of oxygen from arterial blood (see Chapter 1). Thus, the arterial–venous oxygen content difference widens with increasing exercise intensity. Maximum heart rate in intense exercise in a physically fit 20 year old ‘textbook person’ is 180–195 bpm. This figure changes with age so that maximum heart rate in a 10-year-old may be 210 bpm (see Chapter 12), whereas in a person aged 65 it is only about 165 bpm. Central command dominates heart rate control in mild exercise but, in more intense forms of exercise, autonomic reflexes (see Chapter 10) and the indirect effects of metabolites (see Chapter 9) generated in contracting muscles become increasingly important. Secretion of adrenaline (epinephrine) and noradrenaline (norepinephrine) from the adrenal medulla, and their effect on the sinoatrial node, also contributes to the increase in heart rate. Stroke volume of the heart increases during dynamic exercise but reaches a maximum level at an exercise intensity of about half maximum O2 consumption (Fig. 13.1). The extent of changes in stroke volume appears to vary with the type of dynamic exercise and the physical fitness of the individual. In trained individuals there may be relatively greater changes in stroke volume at lower workloads. In Chapter 4 the factors determining the stroke volume of the heart are identified as: Increased filling of the right ventricle (increased preload) occurs as a result of increased contraction of limb muscles and therefore increased venous return to the heart. A simple, but often neglected, concept is that increases in cardiac output can only be achieved if there is an equivalent increase in venous return of blood to the heart, you can’t get out what you don’t put in! Sympathetic nervous system activation during dynamic exercise will lead to venoconstriction which also increases preload on the heart. When resting in a supine position, because there is less effect of gravity on venous return from the lower part of the body, stroke volume is already higher than in an upright posture. The cardiac output increases which occur during exercise in a supine position (e.g. swimming) are achieved almost entirely as a result of an increase in heart rate because stroke volume is already approaching maximum levels at the start of exercise. Contractility increases in the heart are associated with an increase in myocyte intracellular [Ca++] and lead to an increased force of ventricular contraction (see Chapter 4). Sympathetic nervous system activation in exercise and the release of adrenal medulla catecholamines will lead to increased contractility via activation of β-adrenoceptors. The modest increase in mean arterial blood pressure (Fig. 13.2
EXERCISE AND THE CARDIOVASCULAR SYSTEM
Dynamic (isotonic) exercise
Initiation of the cardiovascular responses to exercise
Cardiovascular changes in sustained exercise
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


EXERCISE AND THE CARDIOVASCULAR SYSTEM