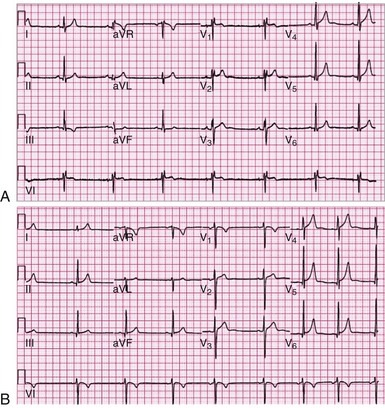
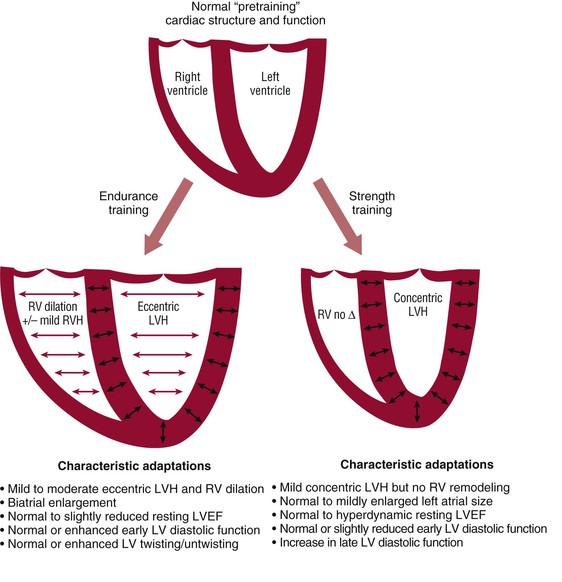
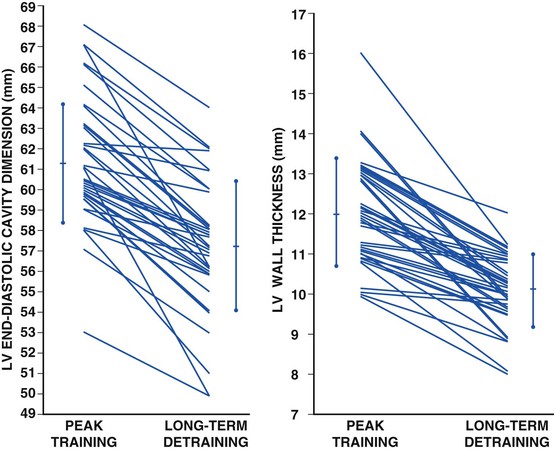
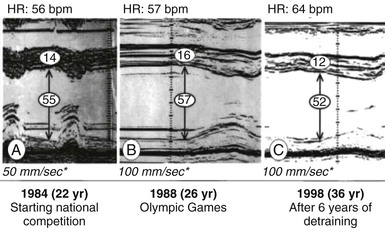
Paul D. Thompson, Aaron Baggish Cardiovascular (CV) specialists require an understanding of exercise physiology, the benefits and risks associated with exercise, and the CV adaptations that occur with exercise training because of the following: 1. Many of the symptoms of CV disease appear during the stress of physical exertion. 2. Patients with or without CV disease request advice on exercise from CV specialists. 4. CV specialists must commonly evaluate symptoms in active individuals. Concern about the CV risks and benefits related to exercise is not new. In 1867, the London surgeon F.C. Sky equated the Oxford-Cambridge crew race to cruelty to animals and opined that such extreme exertion would cause heart disease.1 Concern about rowers’, runners’, and bicyclists’ hearts emerged in the late 19th century, when these activities migrated from being occupational competitions among only the working classes to being sporting activities for the social elite.1 The normal CV adaptations to exercise training include resting bradycardia, global cardiac enlargement, and functional pulmonic and aortic valve flow murmurs. Evaluation of these normal adaptations by auscultation and cardiac percussion, the diagnostic tests of the day, led to their interpretation as signs of pathologic heart block, dilated cardiomyopathy, and valvular obstruction, respectively.1 Concerns about the risks associated with prolonged and vigorous exercise were commonplace in the 19th and early 20th centuries. Clarence DeMar, the winner of seven Boston Marathons, took a 5-year hiatus from competition during the peak of his competitive years, in part because according to DeMar, “The frequent warnings of the doctors and fans of the danger to one’s heart … had left their impression.”1 Such concerns pertain to the present inasmuch as questions persist about the risks related to exercise and the effects of prolonged exercise on myocardial function.2 “Physical activity” refers literally to any body movement, but in epidemiologic studies examining physical activity and health, it refers to activities producing substantial increases in oxygen (O2) consumption. Physical activity can be performed during work or during leisure and recreational tasks, and both work and leisure activities have been used to study the effects of physical activity on CV health. Physical activity designed to improve health or obtain performance benefits is considered “exercise.” Exercise requiring primarily an increase in O2 transport is referred to as “aerobic exercise,” whereas exercise primarily stressing the skeletal muscular system is referred to as “resistance exercise.” Repetitive exercise designed to increase the capacity of O2 transport and the CV system is labeled “aerobic exercise training,” whereas repetitive exercise designed to increase muscle strength is considered “strength” or “resistance” exercise training. Athletic and work activities can be divided into primarily aerobic or resistance exercise activities depending on their aerobic and strength components, but such divisions are arbitrary because aerobic activities such as jogging enhance leg muscular strength and resistance exercises such as weightlifting can stress the O2 delivery system, depending on the resistance used and the number of exercise repetitions performed. The basic principles of the acute response to exercise and the CV adaptations to exercise training have been summarized elsewhere3,4 and are discussed in Chapter 47; only principles critical to this chapter are repeated here. Physical activity acutely increases O2 demand, which prompts the CV system to increase cardiac output (Q) and the arterial-venous (A-V) O2 difference. The increase in Q is coupled to the energy required such that a 1-liter increase in oxygen consumption ( The CV response to exercise has both an external and internal work rate.3 The external work rate is the The primary CV effect of repetitive aerobic exercise sessions or aerobic exercise training is to increase maximal exercise capacity, measured physiologically by an increase in Intense and prolonged aerobic exercise training produces an array of CV adaptations, commonly referred to as “athlete’s heart.” Such changes include an increase in resting SV and a decrease in resting HR. The physiologic mediators of these CV adaptations are not fully defined but are accompanied by and may be produced by increased resting vagal tone and reduced resting sympathetic tone. These changes in autonomic tone, most manifested in highly trained endurance athletes, can be associated with resting bradycardia, marked sinus arrhythmia, first-degree heart block, Mobitz I second-degree atrioventricular (AV) block, and even third-degree AV block during sleep. The reduced AV conduction velocity may make accessory conduction pathways, such as those of Wolff-Parkinson-White syndrome, more apparent. The increased vagal tone may also contribute to an increased prevalence of an early repolarization ST-segment pattern and ST-T wave abnormalities in athletes (Fig. 79-1).6 Four-chamber cardiac enlargement accompanies the increase in SV, but left ventricular (LV) wall thickness usually increases only mildly.4 Small increases in aortic root dimensions also occur, but increases in aortic size greater than expected for body size are not associated with athlete’s heart.7 In contrast to the extensive cardiac changes reported in endurance-trained athletes, strength exercise training produces modest increases in LV wall thickness with little change in chamber dimensions.4 Exercise training evokes numerous structural and functional cardiac adaptations (Fig. 79-2).8 Athletes have an increase in the average dimensions of all four cardiac chambers, but the dimensions generally do not exceed the upper limits of normal (ULN), and contractile function is usually preserved. For example, among 947 national-caliber and international-caliber Italian athletes, only 16 had LV wall thickness greater than 12 mm, the ULN.9 LV end-diastolic chamber size was also greater than 55 mm, the ULN value, in 45% of 1300 elite Italian athletes.10 The most marked increases in LV size occurred in the largest athletes, and LV dimensions were inversely related to HR (r = −0.37) and directly related to body surface area (r = 0.76).10 Cessation of exercise training, or “detraining,” may help in clinically differentiating adaptations to exercise training as a result of hypertrophic cardiomyopathy. Several studies have examined the effect of cessation of exercise training, or “detraining,” in endurance athletes with eccentric LV hypertrophy (LVH), a geometric pattern of hypertrophy characterized by concomitant LV wall thickening and chamber dilation. Regression of eccentric LVH can occur in highly trained athletes after 6 to 34 weeks (mean, 13 weeks) of abstinence from exercise.11 A detraining study of 40 Italian male athletes with eccentric LVH and peak fitness LV dimensions (mean ± SD) of 61.2 ± 2.9 mm and LV wall thickness of 12.0 ± 1.3 mm reported complete normalization of wall thickness and a significant but incomplete reduction in cavity dilation after 5.8 ± 3.6 years of detraining (Figs. 79-3 and 79-4).12 Because the LV wall thickening and concentric LVH common in strength-trained athletes can regress partially after 3 months and completely after 6 months of detraining, the later 6-month period is recommended for such diagnostic trials.13 Multiple epidemiologic, cross-sectional studies comparing CV risk in healthy subjects at various levels of work and leisure physical activity have demonstrated that more active subjects have lower CV risk than do their more sedentary counterparts. The reduction in risk in the most active versus the least active subjects is approximately 30%.14 Similarly and as discussed in Chapter 47, patients participating in cardiac rehabilitation programs have a reduced risk for recurrent cardiac events. The specific mechanisms mediating this effect have not been defined, but habitual physical activity has multiple potentially beneficial effects on atherosclerotic risk factors. Specifically, habitual physical activity reduces SBP, body weight, blood glucose, and triglycerides and increases high-density lipoprotein cholesterol.15 Some of the effects of exercise on blood pressure, glucose, and triglycerides occur acutely within 24 hours of a single aerobic exercise session.16 Such observations raise the possibility that the effects of “exercise training” on these parameters include an acute exercise effect magnified by the greater amount of exercise that can be performed by a trained person in a single exercise session because of the increase in exercise capacity produced by exercise training. Exercise training also produces potentially beneficial effects on clotting factors and inflammation. The increases in vagal tone may reduce the risk for ventricular fibrillation in response to ischemia.17 Cross-sectional studies, however, cannot prove that the reductions in CV risk are due to physical activity alone. Individuals who choose to be more physically active may inherit greater exercise capacity, thereby leading them to select active lifestyles and to have innately lower CV risk. Supporting this possibility is the observation that rats selected and bred over multiple generations for superior exercise performance have lower CV risk factors even though these risk factors were not used in the selection process.18 The same physiologic factors associated with increased exercise capacity may also be associated with reduced CV risk, and individuals choosing an active lifestyle may have lower CV risk independent of their exercise habits. This possibility appears unlikely, however, given the plethora of epidemiologic and experimental evidence linking increased physical activity with lower CV risk, but it remains a possibility that requires consideration. Despite the putative benefits of habitual physical activity, convincing evidence has shown that vigorous physical activity, generally defined as six or more METS, or metabolic equivalents, of resting energy expenditure (3.5 mL of O2 per kilogram of body weight per minute), transiently increases the risk for sudden cardiac death (SCD) and acute myocardial infarction (AMI).17
Exercise and Sports Cardiology
Introduction and Historical Perspective
Definition of Terms
The Cardiovascular Response to Exercise and Exercise Training
 ) produces a 5- to 6-liter increase in Q. Q is increased by augmentation of both the heart rate (HR) and stroke volume (SV). Several mechanisms increase the A-V O2 difference, including shunting of blood from the renal and splanchnic beds to exercising muscle, hemoconcentration from loss of plasma fluid into the extravascular space as a result of the osmotic force produced by metabolites released into the interstitial space during exertion, and increased arterial oxygen extraction by active skeletal and cardiac muscle. Myocardial O2 (MO2) demand depends in part on HR and systolic blood pressure (SBP) and increases with exertion because both HR and SBP increase. As discussed in Chapter 47, this increase in O2 can produce ischemia in individuals with flow-limiting coronary artery lesions. In addition, the coronary arteries should dilate in response to the myocardial metabolic demands of exertion, but inadequate vasodilation or frank vasoconstriction develops with exercise in some individuals with coronary atherosclerosis because of endothelial dysfunction.5 Cardiac ischemia, induced by exercise, can contribute to cardiac events during exercise, as discussed later.
) produces a 5- to 6-liter increase in Q. Q is increased by augmentation of both the heart rate (HR) and stroke volume (SV). Several mechanisms increase the A-V O2 difference, including shunting of blood from the renal and splanchnic beds to exercising muscle, hemoconcentration from loss of plasma fluid into the extravascular space as a result of the osmotic force produced by metabolites released into the interstitial space during exertion, and increased arterial oxygen extraction by active skeletal and cardiac muscle. Myocardial O2 (MO2) demand depends in part on HR and systolic blood pressure (SBP) and increases with exertion because both HR and SBP increase. As discussed in Chapter 47, this increase in O2 can produce ischemia in individuals with flow-limiting coronary artery lesions. In addition, the coronary arteries should dilate in response to the myocardial metabolic demands of exertion, but inadequate vasodilation or frank vasoconstriction develops with exercise in some individuals with coronary atherosclerosis because of endothelial dysfunction.5 Cardiac ischemia, induced by exercise, can contribute to cardiac events during exercise, as discussed later.
 required by the exercise task and, as mentioned earlier, is a direct determinant of Q.
required by the exercise task and, as mentioned earlier, is a direct determinant of Q.  can also be estimated from treadmill speed and grade or from a stationary bicycle watt requirement. The internal work rate refers to the MO2 required for the exercise task and is related directly to increases in HR. In contrast to Q, the HR response to exercise and therefore to MO2 is not determined by the external work rate or
can also be estimated from treadmill speed and grade or from a stationary bicycle watt requirement. The internal work rate refers to the MO2 required for the exercise task and is related directly to increases in HR. In contrast to Q, the HR response to exercise and therefore to MO2 is not determined by the external work rate or  but instead by the
but instead by the  required relative to the individual’s maximal exercise capacity—or
required relative to the individual’s maximal exercise capacity—or  . Individuals with higher exercise capacity and a greater
. Individuals with higher exercise capacity and a greater  have a larger SV at any given external work rate such that any exercise task, as well as
have a larger SV at any given external work rate such that any exercise task, as well as  demand, requires a slower HR to generate the same, externally determined Q.
demand, requires a slower HR to generate the same, externally determined Q.
 . This increase in healthy subjects results from increases in maximal Q and the maximal A-V O2 difference.3 Because maximal HR is largely immutable, determined by age, and minimally affected by exercise training, the increase in maximal Q results from an increase in maximal SV. The increase in SV means that performing the same exercise task, which requires the same
. This increase in healthy subjects results from increases in maximal Q and the maximal A-V O2 difference.3 Because maximal HR is largely immutable, determined by age, and minimally affected by exercise training, the increase in maximal Q results from an increase in maximal SV. The increase in SV means that performing the same exercise task, which requires the same  , can be performed at a slower HR and a lower MO2 or internal work rate. The reduction in HR and thereby MO2 contributes to the increase in exercise capacity in patients with angina pectoris after exercise training (see Chapter 47). In addition to the increase in maximal exercise capacity, exercise training also increases endurance capacity, or the ability to perform submaximal effort for a prolonged period. This effect is a critically important component of the exercise training response because few work and recreational tasks require maximal CV effort.
, can be performed at a slower HR and a lower MO2 or internal work rate. The reduction in HR and thereby MO2 contributes to the increase in exercise capacity in patients with angina pectoris after exercise training (see Chapter 47). In addition to the increase in maximal exercise capacity, exercise training also increases endurance capacity, or the ability to perform submaximal effort for a prolonged period. This effect is a critically important component of the exercise training response because few work and recreational tasks require maximal CV effort.
The Effects of Habitual Physical Activity on Cardiovascular Risk (See also Chapter 42)
The Cardiovascular Risks of Exercise
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Exercise and Sports Cardiology
79