Tako-tsubo cardiomyopathy (TC) is a novel form of acute heart failure, characterized by regional left ventricular dysfunction without coronary artery obstruction, and usually triggered by a stressful event. Excessive circulating catecholamines have been implicated in the pathophysiology of this condition. This report documents the unusual occurrence of acute TC events in 2 male subjects of disparate ages, 16 and 66 years, for whom subsequent investigation in both led to the unexpected discovery of catecholamine-producing pheochromocytoma. Marked elevation of plasma catecholamines (epinephrine, norepinephrine, and dopamine) was present in both subjects and were remarkably similar to those previously reported in female patients with TC triggered by emotional stress. These observations show a common link between TC occurrence and elevated catecholamine levels in both male and female patients and, therefore, support the hypothesis that excessive levels of catecholamines may be involved in the pathophysiology of TC independent of age or gender.
Tako-tsubo cardiomyopathy (TC) is a novel form of acute heart failure characterized by regional left ventricular (LV) dysfunction without coronary artery obstruction, predominantly afflicting women of advanced age, triggered by a stressful event. Excessive circulating catecholamines have been implicated in the pathophysiology of this condition, such as that may occur in patients with adrenal and extra-adrenal pheochromocytoma. Also, TC is uncommon in men and is virtually nonexistent in patients <20 years. This report documents the occurrence of acute TC events in a 16-year-old boy and in a 66-year-old man for whom subsequent investigation in both led to the unexpected discovery of catecholamine-producing neuroendocrine tumors, additional evidence of the importance attributable to catecholamines in the mechanism of TC.
Case Report #1
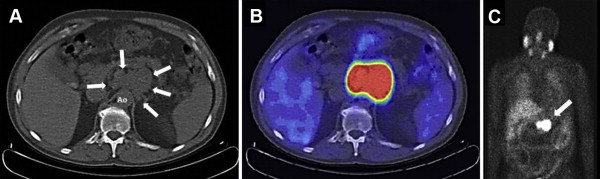
A previously healthy 16-year-old white boy was presented to the emergency department with acute chest pain. For 2 months, he had experienced exertional chest pain, light-headedness, and nausea. On the day of admission, chest pain awoke him from sleep. In the emergency department, blood pressure was 114/47 mm Hg and heart rate 126 beats/min. Electrocardiogram showed sinus tachycardia with ST elevation in leads V2 to V3, and initial troponin I was increased, 1.9 ng/ml. Echocardiogram demonstrated a regional wall motion abnormality in a noncoronary distribution with akinesia of the mid-LV segments and hypercontraction at the base and apex (mid-LV ballooning pattern), typical of TC; ejection fraction was 52% ( Figure 1 ). Cardiovascular magnetic resonance imaging showed absent delayed gadolinium uptake without evidence of myocarditis. Computed tomographic (CT) coronary angiogram demonstrated normal epicardial coronary arteries. Unexpectedly, a large oval mass above the right kidney was evident by both cardiovascular magnetic resonance imaging and CT coronary angiogram that measured 6.5 × 7.7 × 7.1 cm ( Figure 1 ).
Biochemical testing revealed markedly elevated plasma and urinary catecholamines and metabolites ( Table 1 ). Phenoxybenzamine was administered for 1 week with transition to intravenous phentolamine for 24 hours at which time right subcostal laparotomy revealed a right suprarenal tumor measuring 7 cm largely confined to the retroperitoneum. A large (1.5 cm) right adrenal vein was identified draining to the inferior vena cava, and a right thoracotomy was performed with right diaphragmatic takedown to allow complete exposure of the tumor. The adrenal vein was ligated and a well-encapsulated tumor was excised, without significant complications ( Figure 1 ). Histologic examination demonstrated pheochromocytoma with positive staining for chromagranin and synaptophysin. The postoperative course was uneventful, the patient remained normotensive, and predischarge echocardiogram showed complete resolution of segmental wall motion abnormalities with a global ejection fraction of 69%.
| Variable | Patient 1 | URL Multiple | Patient 2 | URL Multiple |
|---|---|---|---|---|
| Catecholamines, plasma (pg/ml) | ||||
| Dopamine (reference: < 30 pg/ml) | 47 | 1.6× | 41 | 1.4× |
| Epinephrine (reference: ≤ 111 pg/ml) | 482 | 4.3× | 296 | 2.7× |
| Norepinephrine (reference: 70-750 pg/ml) | 2282 | 3× | 1743 | 2.3× |
| Catecholamine metabolites, plasma (nmol/L) | ||||
| Metanephrine (reference < 0.9 nmol/L) | 13 | 14.4× | 4.7 | 5.2× |
| Normetanephrine (reference < 0.5 nmol/L) | 21 | 42× | 14 | 28× |
| Catecholamine metabolites, urine (μg/24 hours) | ||||
| Metanephrine (reference: 69-221 μg/24 hours) | 8828 | 40× | 7015 | 32× |
| Normetanephrine (reference: 91-456 μg/24 hours) | 6848 | 15× | 10327 | 23× |
Case Report #2
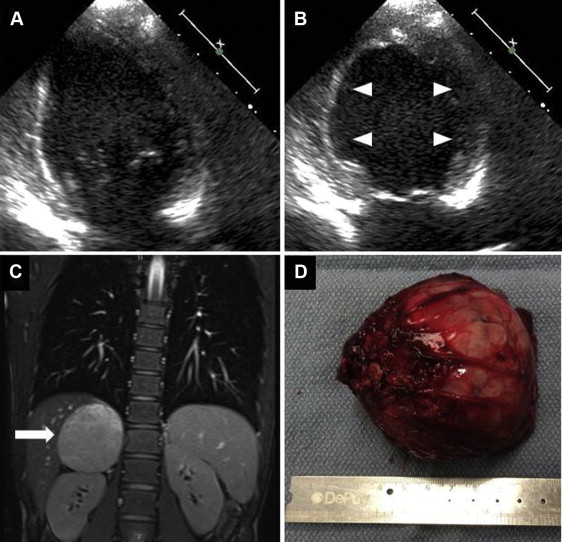
A 66-year-old man with previous paroxysmal atrial fibrillation, LV ejection fraction 55%, and no hypertension underwent elective outpatient surgical correction of right first metatarsal osteophyte under spinal anesthesia. In the recovery room, the patient developed acute hypertension (blood pressure 200/120 mm Hg), transient tachycardia (heart rate not recorded), and acute pulmonary edema requiring intubation. Initial electrocardiogram demonstrated diffuse ST-segment depression, and initial troponin I was increased, 5.8 ng/ml. Echocardiogram demonstrated a regional wall motion abnormality in a noncoronary distribution with akinetic basal LV segments and apical hypercontraction (basal LV ballooning pattern), typical of basal ballooning variant TC with ejection fraction of 40%. Coronary angiography revealed normal coronary arteries. Because of acute respiratory failure, a chest CT scan was performed that included the upper abdomen and incidentally showed a 7.6 × 5.7 × 5.1 cm irregular para-aortic mass ( Figure 2 ). Biochemical testing revealed markedly elevated plasma and urinary catecholamines and metabolites ( Table 1 ), and I-123-metaiodobenzyl-guanidine imaging was consistent with extra-adrenal pheochromocytoma (paraganglioma) ( Figure 2 ). Phenoxybenzamine, atenolol, and lisinopril were administered, and a follow-up echocardiogram at 1 week showed complete resolution of segmental wall motion abnormalities and normal ejection fraction of 71%. After 2 months of pharmacologic treatment, the patient underwent surgical exploration through transverse epigastric incision that revealed a peri-aortic tumor consistent with paraganglioma. The tumor was successfully freed from the aorta, superior mesenteric artery, and celiac plexus and complicated by transient hypotension (systolic blood pressure 70 mm Hg) and transient atrial fibrillation. The excised tumor was a 7 × 6 × 3 cm solid-to-cystic hemorrhagic mass, and histologic examination revealed extra-adrenal pheochromocytoma. The patient recovered completely.