EVAR for Traumatic Aortic Injuries
S. Rahimi
Indications
Indications for endovascular repair of traumatic aortic injuries include dissection, pseudoaneurysm, and rupture. The patient must have adequate anatomy to allow advancement of the endovascular delivery system and adequate proximal and distal aortic seal zones to exclude the area of injury without major branch vessel coverage. The exception to this is the left subclavian artery which in the setting of trauma can be covered with good outcomes.
Mural hematomas and intimal flaps are considered minor injuries and will usually resolve on their own. Pseudoaneurysms, even small ones, rarely remain stable over time, with an unacceptably high risk of rupture, embolization, fistulization, and compression of adjacent neurovascular structures.
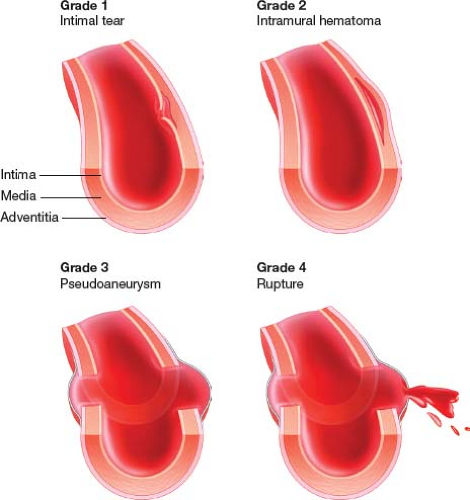
Traumatic aortic injury can be classified by a grading system 1 to 4: Grade 1, intimal tear; Grade 2, intramural hematoma; Grade 3, pseudoaneurysm; and Grade 4, rupture (Fig. 31.1). Grade 1 injuries can be observed and Grades 2 to 4 should be repaired.
It is important to take into consideration the associated injuries of the trauma patient. The most life-threatening injuries must be assessed first. There are times when the patient needs to be stabilized and the aortic repair should be delayed. There are also times when simultaneous repair is indicated.
Aortic injury can occur from blunt or penetrating trauma. Penetrating trauma can occur at any level. Repair for blunt aortic trauma will be by far the most common scenario with the majority of those being thoracic aortic transection due to the thoracic aorta being fixed and immobile at the level of the ligamentum arteriosum. Blunt injuries can also occur at the level of the diaphragm, another location where the aorta is fixed and immobile relative to the aortic segment proximally and distally.
Contraindications
Endovascular repair is contraindicated if the aortic diameter proximally and distally to the injured segment is too small or large for approved devices. If the aorta adjacent to
the injured segment has severe angulation, endovascular repair is contraindicated. In the acute setting endovascular repair is contraindicated when the access vessels are too small or diseased to allow for advancement of the delivery system or if the area of injury requires coverage of major visceral vessels or the left common carotid or innominate artery to exclude the injured segment.
the injured segment has severe angulation, endovascular repair is contraindicated. In the acute setting endovascular repair is contraindicated when the access vessels are too small or diseased to allow for advancement of the delivery system or if the area of injury requires coverage of major visceral vessels or the left common carotid or innominate artery to exclude the injured segment.
In a more stable clinical setting conduits for access and debranching procedures can be used to treat some of these injuries with endografts. A seal zone of normal uninjured aorta is required for seal and exclusion of the injured segment both proximally and distally by the endograft. If this seal zone is not available, then endovascular repair is contraindicated. In the acute setting, if the aortic injury is contained (no evidence of rupture) and the patient has other life-threatening injuries, the aortic repair should be delayed.
Additional contraindications include patients with known allergy to the device materials or patients who have a condition that threatens to infect the graft.
One of the first steps in caring for these patients prior to surgery is to avoid hypertension. In these patients, antihypertensive therapy with nitroprusside or labetalol is recommended until a decision about aortic repair is reached.
The key component in the planning is the CTA scan to determine if the patient is a candidate for endovascular repair of the injured aorta. To achieve a reliable seal, landing zones of at least 1.5 cm are recommended. This is problematic, as approximately one-half of all patients with thoracic aortic rupture are within 1 to 2 cm of the left subclavian artery (see Fig. 31.2), implying that the origin of this vessel will have to be crossed in a significant number of cases. There is low risk of acute left arm ischemia following this and delayed steal syndrome can be electively treated with left carotid–subclavian bypass when the patient has stabilized.
 Figure 31.2 Injury very close to left subclavian artery. Note the floppy portion of stiff wire bending off the aortic valve to allow the endograft to take the outer curvature of the aortic arch. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree