EVAR for Infrarenal Abdominal Aortic Aneurysm Repair
Jeffrey C. Hnath
The development of the endovascular abdominal aortic repair (EVAR) by Parodi revolutionized the treatment of abdominal aortic aneurysms (AAA). Open AAA repairs were effective in preventing rupture but could be associated with significant perioperative morbidity and mortality. EVAR offered a less invasive option that was both less morbid and could also be used in patients deemed unfit for open AAA repair.
The indications for repair of AAA are related to size, shape, symptoms, and growth rate. AAA repair is indicated at a diameter of 5 to 5.5 cm when the risk of rupture outweighs the risk of perioperative death or complication. Aneurysm shape is important, as a saccular aneurysm may be more prone to rupture than a fusiform aneurysm. Abdominal pain, back pain, or aneurysm tenderness are signs and symptoms of an AAA that could be about to rupture, indicating the need for urgent repair. An accelerated growth rate of more than 5 mm per year also indicates an unstable aneurysm that requires repair.
Preoperative planning is the most important aspect of a successful EVAR. CT angiography of the abdomen and pelvis gives fine details of the anatomy to guide the selection of devices and the route to deliver the devices. Rarely an actual angiogram is necessary for planning and this is done mainly to evaluate the iliac arteries for suitability of endograft delivery.
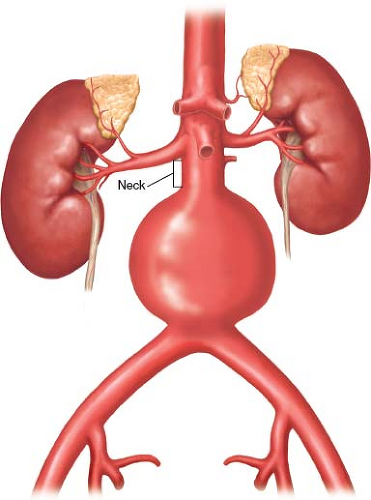
Aortic Neck
The bottom edge of the lowest renal artery is the beginning of the aortic neck and is the starting point for neck measurement and for determining graft length (Fig. 32.1).
The angle of which the lowest renal artery emanates from the aorta should be noted in order to adjust the gantry angle of the fluoroscopy unit intraoperatively. For example, if the renal artery comes off the aorta at the 4 o’clock position, the gantry should be angled at 30 degree left anterior oblique (LAO) to get the most accurate images.
The angle of which the lowest renal artery emanates from the aorta should be noted in order to adjust the gantry angle of the fluoroscopy unit intraoperatively. For example, if the renal artery comes off the aorta at the 4 o’clock position, the gantry should be angled at 30 degree left anterior oblique (LAO) to get the most accurate images.
The length of normal aorta below the renal arteries is referred to as the neck. The endograft needs a length of normal aorta to achieve a seal as well as graft fixation. Each endograft device requires a certain length of aorta as dictated by the indications for use (IFU). Generally 15 mm of normal neck is required, but there are some devices that only require 10 mm per their IFU. The seal is based in a pressure fit between the outer walls of the endograft and the inner wall of the aorta. Device size is based in a 10% to 15% oversize compared to the aortic diameter to achieve the pressure fit. Undersizing may result in a leak secondary to poor wall apposition and oversizing may result in a leak from fabric in-folding. Some device IFUs measure diameter from intima to intima such as the Excluder (Gore, Flagstaff, AZ) and others measure adventitia to adventitia such as the Talent (Medtronic, Minneapolis, MN).
CT angiograms also show the degree of intra-aortic mural thrombus. A significant amount of mural thrombus may contraindicate an EVAR or it may affect the choice of endograft fixation. The endografts are held in place by two types of fixation. Passive fixation results from the pressure the graft exerts outwardly on the inside of the aortic walls. Active fixation results from hooks or anchors that actively grasp the inside of the aorta. If there is a significant degree of mural thrombus, consideration may be given to using a device that has suprarenal fixation and hooks above the renal arteries. Grafts with suprarenal fixation are also good for aortas with short necks or if the neck has a reverse conical taper configuration.
The angle of the neck is important to note as well when choosing a device. Some endografts are inherently more rigid than others and this may lead to slippage or leaks in a severely angled neck. There are newer endografts on the market that have improved flexibility that are designed for angled necks such as the Aorfix (Lombard, Irvine, CA).
Aortic Length
The length of aorta is an important measurement because some devices require a certain length of aorta to be able to fully open a gate for cannulation. A short AAA may require either a specific device or a uni-iliac configuration with a femoral to femoral crossover bypass.
Iliac Access Arteries
Evaluation of the iliac arteries necessitates the CT angiogram to include the pelvis. The iliac artery imaging is important because occlusive disease or small size may preclude a repair or require different devices or maneuvers. Generally, the artery diameter multiplied by three will give the French size of the artery. Fortunately, the newer devices are packaged into lower profile hydrophilic packaging to allow for safe delivery through the iliac arteries. If there is a question regarding the suitability of the iliac arteries, then digital subtraction angiography may be necessary preoperatively. The CT angiogram will also provide the diameter of the iliac arteries for selection of an appropriately sized device to achieve a seal.
Positioning
The patient is placed supine on an operating table that is radiolucent to allow for unobstructed imaging of the abdomen. The safety strap for the table is placed across the lower thighs and the cautery grounding pads are placed on the lower thighs as well to prevent obstructing the imaging.
Anesthesia
The type of anesthetic is based on patient comfort and physician comfort. A straightforward percutaneous EVAR (PEVAR) may only require sedation and local anesthetic, whereas an agitated patient or a patient with anatomy that has potential for rupture, may be better served with general anesthesia.
Femoral Access
Bilateral femoral arteries can be accessed by either a cut down or percutaneously. Open exposure can be performed through either longitudinal or transverse incisions. Only enough artery needs to be exposed to allow for clamping and arterial repair. Limiting the incision may reduce wound complications such as skin necrosis and lymph leaks.
Percutaneous femoral artery access is another option in carefully selected patients. Patients with small common femoral arteries, heavily calcified vessels, or stenotic femoral arteries my benefit from open exposure to allow proper repair. PEVAR has been made possible by the use of multiple suture mediated closure devices and the reduction in size of the delivery devices.
Puncture the anterior aspect of the common femoral artery either under fluoroscopic or ultrasound guidance. A small squirt of contrast through the access needle will confirm an adequate artery and good placement.
A regular stiffness wire (Bentson, Cook Medical, Bloomington, IN) is placed into the aorta followed by a 6- or 7-Fr sheath to dilate the tract.
The skin is nicked with a scalpel to prevent the knot of the Perclose device from catching on the dermis at the end of the case.
The sheath is removed and a Perclose device (Abbott Vascular, Chicago, IL) is advanced into the femoral artery. The wire is removed and the Perclose device is pulled back until the side port bleeding stops. For a sheath 12-Fr or smaller, 1 Perclose is deployed
at the 12 o’clock position. If a larger sheath is to be used, the Perclose is positioned at 2 o’clock and a second at 10 o’clock.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree