The aim of this study was to determine whether patients from the Clinical Evaluation of the XIENCE V Everolimus Eluting Coronary Stent System in the Treatment of Patients With de Novo Native Coronary Artery Lesions (SPIRIT) IV trial who underwent percutaneous coronary intervention, who had target lesions with jailed side branches, had improved clinical outcomes when treated with the XIENCE V versus Taxus Express 2 drug-eluting stent. In the SPIRIT III randomized trial, patients with target lesions with jailed side branches after XIENCE V compared with Taxus Express 2 implantation had lower 2-year rates of major adverse cardiac events. The SPIRIT IV trial represents a larger more diverse patient population compared with SPIRIT III. In the large-scale, prospective, multicenter, randomized SPIRIT IV trial, 3,687 patients who underwent coronary stenting with up to 3 de novo native coronary artery lesions were randomized 2:1 to receive XIENCE V versus Taxus Express 2 stents. Two-year clinical outcomes of patients with or without jailed side branches after stenting were compared. A jailed side branch was defined as any side branch >1.0 mm in diameter within the target segment being stented, excluding bifurcations deemed to require treatment. Of the 3,687 patients in SPIRIT IV, a total of 1,426 had side branches that were jailed during angioplasty of the target lesion. Patients with jailed side branches after XIENCE V compared with Taxus Express 2 implantation had significantly lower 2-year rates of target lesion failure (6.5% vs 11.9%, p = 0.001), major adverse cardiac events (6.6% vs 12.2%, p = 0.0008), ischemia-driven target vessel revascularization (4.1% vs 7.9%, p = 0.004), and stent thrombosis (0.6% vs 2.8%, p = 0.001). In conclusion, patients with jailed side branches after stenting with XIENCE V compared to Taxus Express 2 devices had superior clinical outcomes at 2 years in the large-scale randomized SPIRIT IV trial.
Side branch jailing during coronary artery stent implantation occurs when the implanted stent covers the ostium of a side branch originating from the parent vessel. This is frequently associated with side branch compromise and increased rates of periprocedural myocardial infarction and can contribute to higher rates of adverse outcomes in these patients. In a post hoc analysis from the Clinical Evaluation of the XIENCE V Everolimus Eluting Coronary Stent System in the Treatment of Patients With de Novo Native Coronary Artery Lesions (SPIRIT) III randomized trial, patients with jailed side branches after treatment with XIENCE V (Abbott Vascular, Santa Clara, California) compared with Taxus Express 2 (Boston Scientific Corporation, Natick, Massachusetts) stents had lower rates of major adverse cardiac events sustained out to 2 years. The purposes of the present study were to investigate whether the frequency and consequences of side branch jailing favor the XIENCE V in the larger and more complex SPIRIT IV population and to investigate whether the improved clinical outcomes with XIENCE V compared with Taxus Express 2 devices seen in SPIRIT IV may in part be explained by the presence of jailed side branches. We therefore performed a post hoc analysis of patients with and without jailed side branches from the SPIRIT IV trial, comparing 2-year clinical outcomes between the XIENCE V and Taxus Express 2 treatment arms.
Methods
The design of the SPIRIT IV trial has been previously described in detail. In brief, SPIRIT IV was a prospective, randomized, single-blind, active-controlled clinical trial at 66 United States clinical sites, in which 3,687 patients ≥18 years who underwent percutaneous coronary intervention were randomized in a 2:1 ratio to XIENCE V or Taxus Express 2 stents. Patients with up to 3 de novo native coronary artery lesions, with target lesion lengths ≤28 mm and reference vessel diameters ≥2.5 to ≤4.25 mm, were enrolled. Lesions with side branches were permitted unless the side branch had an ostial stenosis >50% and was >2.0 mm in diameter. A jailed side branch was defined by the angiographic core laboratory as any side branch >1.0 mm in diameter within the target segment being stented.
The primary end point was target lesion failure (a composite of cardiac death, target vessel myocardial infarction, and ischemia-driven target lesion revascularization) at 1 year. Secondary end points included major adverse cardiac events (a composite of cardiac death, all myocardial infarctions, and ischemia-driven target lesion revascularization), myocardial infarction, all-cause mortality, and definite or probable stent thrombosis according to the Academic Research Consortium criteria. An independent angiographic core laboratory (Cardiovascular Research Foundation, New York, New York) assessed all angiograms blinded to treatment assignment for baseline and final lesion characteristics using validated quantitative methods (MEDIS Medical Imaging Systems, Leiden, The Netherlands).
The XIENCE V stent is composed of an L-605 cobalt chromium alloy with a stent strut thickness of 81 μm and a polymer coating consisting of a primer layer and a drug matrix layer containing everolimus, with a total thickness of 7.8 μm. XIENCE V stents were available in diameters of 2.5, 3.0, 3.5, and 4.0 mm and in lengths of 8, 18, and 28 mm. The Taxus Express 2 stent is composed of 316 L stainless steel with a stent strut thickness of 132 μm and a Transulate polymer carrier coating loaded with paclitaxel, with a total thickness of 19.6 μm. Taxus Express 2 stents were available in diameters of 2.5, 2.75, 3.0, 3.5, and 4.0 mm and in lengths of 8, 12, 16, 20, 24, 28, and 32 mm.
Continuous variables were compared with the use of Student’s t test and are presented as mean ± SD. Categorical variables were compared using Fisher’s exact tests and are expressed as counts and percentages. Time-to-event survival curves were estimated according to the Kaplan-Meier method and were compared using the log-rank test. All statistical tests were 2 tailed, and p values <0.05 were considered significant. Demographic, clinical, and procedural variables were included in univariate and multivariate Cox regression analyses. Final models were built on the basis of statistical significance and clinical consideration. The presence of a side branch at the target lesion was forced into the final model of the multivariate regression analyses in this study. All statistical analyses were performed using SAS version 9.1.3 (SAS Institute Inc., Cary, North Carolina).
Results
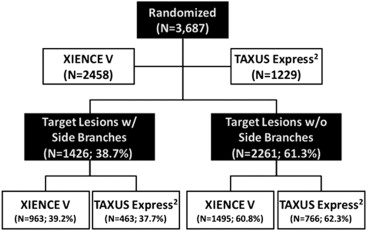
A total of 3,687 patients were enrolled in SPIRIT IV (2,458 receiving XIENCE V stents and 1,229 Taxus Express 2 stents), of whom 963 XIENCE V (39.2%) and 463 Taxus Express 2 (37.7%) patients had ≥1 jailed side branch within the stented segment ( Figure 1 ). Baseline demographics, as well as pre- and postprocedural Thrombolysis In Myocardial Infarction (TIMI) flow grades, were similar between patients with and without jailed side branches ( Table 1 ). Total stent length per lesion was greater in XIENCE V than in Taxus Express 2 patients in the side branch and no–side branch groups. Antiplatelet therapy compliance was similar between groups (p >0.40): aspirin use was >96% at 1 year and >95% at 2 years, and clopidogrel or ticlopidine use was >93% at 1 year and >70% at 2 years.
| Variable | Target Lesions With Side Branches | Target Lesions Without Side Branches | ||||
|---|---|---|---|---|---|---|
| XIENCE V (n ∗ = 963, L † = 1,307) | Taxus Express 2 (n = 463, L = 635) | p Value | XIENCE V (n = 1,495, L = 1,835) | Taxus Express 2 (n = 766, L = 950) | p Value | |
| Age (yrs) | 63.2 ± 10.8 | 63.3 ± 9.8 | 0.94 | 63.3 ± 10.4 | 63.4 ± 10.5 | 0.79 |
| Men | 66.8% | 68.3% | 0.59 | 68.4% | 67.5% | 0.70 |
| Diabetes mellitus | 30.2% | 29.7% | 0.85 | 33.2% | 34.2% | 0.64 |
| Requiring insulin | 7.0% | 9.1% | 0.17 | 9.5% | 10.1% | 0.71 |
| Hypertension ‡ | 76.6% | 75.8% | 0.74 | 77.9% | 76.3% | 0.43 |
| Hypercholesterolemia § | 75.6% | 72.1% | 0.17 | 76.4% | 77.6% | 0.53 |
| Current smokers | 19.9% | 24.5% | 0.05 | 21.9% | 19.4% | 0.19 |
| Previous myocardial infarction | 19.9% | 20.7% | 0.72 | 21.9% | 19.4% | 0.19 |
| Unstable angina pectoris | 27.1% | 29.5% | 0.37 | 28.1% | 28.5% | 0.84 |
| Previous PCI | 10.1% | 7.7% | 0.17 | 11.9% | 11.0% | 0.62 |
| Lesion characteristics | ||||||
| Target coronary artery | ||||||
| Left anterior descending | 51.1% | 50.2% | 0.74 | 32.9% | 32.8% | 1.00 |
| Left circumflex | 21.8% | 23.5% | 0.42 | 25.8% | 26.7% | 0.62 |
| Right | 27.1% | 26.3% | 0.74 | 41.3% | 40.4% | 0.66 |
| Moderate to severe calcium | 30.3% | 28.0% | 0.31 | 23.0% | 24.4% | 0.39 |
| Lesion length (mm) | 15.2 ± 6.8 | 15.0 ± 6.7 | 0.51 | 14.5 ± 6.6 | 14.2 ± 6.6 | 0.36 |
| Reference vessel diameter (mm) | 2.74 ± 0.46 | 2.76 ± 0.45 | 0.29 | 2.75 ± 0.49 | 2.75 ± 0.48 | 0.90 |
| American College of Cardiology/American Heart Association lesion class | ||||||
| A | 8.7% | 12.3% | 0.02 | 12.9% | 15.6% | 0.06 |
| B1 | 35.8% | 35.7% | 1.00 | 42.4% | 43.1% | 0.75 |
| B2 | 33.2% | 30.7% | 0.28 | 26.4% | 26.0% | 0.86 |
| C | 22.3% | 21.3% | 0.64 | 18.3% | 15.4% | 0.06 |
| Procedural results | ||||||
| Single-vessel PCI | 77.2% | 75.2% | 0.42 | 87.4% | 85.9% | 0.32 |
| Double-vessel PCI | 21.6% | 24.2% | 0.28 | 12.1% | 13.8% | 0.26 |
| Triple-vessel PCI | 1.2% | 0.6% | 0.41 | 0.5% | 0.3% | 0.73 |
| Total stent length per lesion (mm) | 22.9 ± 8.9 | 21.3 ± 8.9 | 0.0002 | 22.1 ± 8.9 | 20.6 ± 8.9 | <0.0001 |
| Postdilation | 43.9% | 43.8% | 1.00 | 46.0% | 44.9% | 0.60 |
| Lesions with ≥2 stents implanted | 15.2% | 12.2% | 0.08 | 14.4% | 11.7% | 0.05 |
| Preprocedural TIMI flow grade | ||||||
| 0 | 0.7% | 0.3% | 0.52 | 0.7% | 0.2% | 0.11 |
| 1 | 2.0% | 0.9% | 0.13 | 1.4% | 1.7% | 0.62 |
| 2 | 7.8% | 10.2% | 0.08 | 7.1% | 7.9% | 0.44 |
| 3 | 89.5% | 88.5% | 0.53 | 90.7% | 90.2% | 0.63 |
| Postprocedural TIMI flow grade | ||||||
| 0 | 0.0% | 0.0% | 1.00 | 0.0% | 0.0% | 1.00 |
| 1 | 0.2% | 0.3% | 0.67 | 0.1% | 0.1% | 1.00 |
| 2 | 0.8% | 1.1% | 0.62 | 1.0% | 1.1% | 1.00 |
| 3 | 98.9% | 98.6% | 0.51 | 98.9% | 98.8% | 0.85 |
‡ Defined as a history of hypertension requiring medication.
§ Defined as a history of hypercholesterolemia requiring medication.
In patients with jailed side branches, periprocedural (<48 hours after the index procedure) creatine kinase-MB isoenzyme elevation (>1 times the upper limit of normal) and large creatine kinase-MB elevation (>5 times upper limit of normal) were significantly higher after Taxus Express 2 than XIENCE V implantation, a finding not seen in lesions without side branches ( Table 2 ). Taxus Express 2 patients with jailed side branches also had higher rates of large creatine kinase-MB elevation (>5 times the upper limit of normal) compared with Taxus patients without jailed side branches (5.9% vs 2.4%, p = 0.008). In contrast, side branch jailing was not associated with an increased creatine kinase-MB elevation in patients treated with XIENCE V stents (2.0% vs 3.0%, p = 0.20; Table 2 ). A significantly lower rate of periprocedural target vessel myocardial infarction was observed in the XIENCE V (vs Taxus Express 2 ) patients with jailed side branches (1.0% vs 3.3%, p = 0.005). Periprocedural target vessel myocardial infarction rates were not significantly different between stent treatments in patients without jailed side branches (XIENCE V 1.7% vs Taxus Express 2 0.9%, p = 0.14). Logistic regression analysis demonstrated a significant interaction between side branch jailing and stent type on periprocedural target vessel myocardial infarction (p = 0.002).
| Variable | Target Lesions With Side Branches | Target Lesions Without Side Branches | p Value (With vs Without Side Branches) | |||||
|---|---|---|---|---|---|---|---|---|
| XIENCE V (n = 963) | Taxus Express 2 (n = 463) | p Value | XIENCE V (n = 1,495) | Taxus Express 2 (n = 766) | p Value | XIENCE V | Taxus Express 2 | |
| Any CK-MB >1 × UNL | 18.0% | 24.5% | 0.01 | 17.4% | 21.0% | 0.07 | 0.76 | 0.21 |
| CK-MB >1 to <3 × UNL | 13.7% | 14.8% | 0.65 | 11.9% | 16.1% | 0.02 | 0.24 | 0.65 |
| CK-MB ≥3 to ≤5 × UNL | 2.3% | 3.8% | 0.18 | 2.6% | 2.6% | 1.00 | 0.76 | 0.34 |
| CK-MB >5 × UNL | 2.0% | 5.9% | 0.001 | 3.0% | 2.4% | 0.55 | 0.20 | 0.008 |
Side branch jailing with XIENCE V compared with Taxus Express 2 stents resulted in significantly lower rates of target lesion failure at 1 year (p = 0.0002) and 2 years (p = 0.001), driven by a significantly lower rate of both target vessel myocardial infarction and ischemia-driven target lesion revascularization. Significantly lower rates of 1- and 2-year major adverse cardiac events and stent thrombosis were also seen when side branch jailing followed XIENCE V compared with Taxus Express 2 stent implantation ( Table 3 ). Lesions with side branches compared to those without that were treated with Taxus Express 2 stents had significantly higher rates of target vessel myocardial infarction and stent thrombosis at 1 and 2 years, whereas treatment of a lesion with a side branch with the XIENCE V stent was not associated with an increase in adverse events ( Table 3 ).
| Variable | Target Lesions With Side Branches | Target Lesions Without Side Branches | p Value (With vs Without Side Branches) | |||||
|---|---|---|---|---|---|---|---|---|
| XIENCE V (n = 963) | Taxus Express 2 (n = 463) | p Value | XIENCE V (n = 1,495) | Taxus Express 2 (n = 766) | p Value | XIENCE V | Taxus Express 2 | |
| 1-yr results | ||||||||
| Target lesion failure | 3.6 | 8.5 | 0.0002 | 4.4 | 5.9 | 0.15 | 0.34 | 0.10 |
| Cardiac death | 0.5 | 0.7 | 0.72 | 0.3 | 0.3 | 1.00 | 0.53 | 0.37 |
| Target vessel myocardial infarction | 1.6 | 4.7 | 0.002 | 2.0 | 1.9 | 0.87 | 0.45 | 0.007 |
| Ischemia-driven target lesion revascularization | 1.9 | 5.1 | 0.002 | 2.7 | 4.4 | 0.03 | 0.27 | 0.57 |
| Major adverse cardiac events | 3.6 | 8.7 | 0.0001 | 4.5 | 5.9 | 0.18 | 0.30 | 0.06 |
| Stent thrombosis (Academic Research Consortium definite/probable) | 0.3 | 2.3 | 0.001 | 0.3 | 0.4 | 0.69 | 1.00 | 0.006 |
| 2-yr results | ||||||||
| Target lesion failure | 6.5 | 11.9 | 0.001 | 7.3 | 8.8 | 0.21 | 0.51 | 0.09 |
| Cardiac death | 1.0 | 1.4 | 0.58 | 0.9 | 1.2 | 0.50 | 0.83 | 0.80 |
| Target vessel myocardial infarction | 2.0 | 5.4 | 0.001 | 2.5 | 2.4 | 1.00 | 0.49 | 0.009 |
| Ischemia-driven target lesion revascularization | 4.1 | 7.9 | 0.004 | 4.7 | 6.3 | 0.11 | 0.54 | 0.34 |
| Major adverse cardiac events | 6.6 | 12.2 | 0.0008 | 7.6 | 9.0 | 0.25 | 0.42 | 0.09 |
| Stent thrombosis (Academic Research Consortium definite/probable) | 0.6 | 2.8 | 0.001 | 0.4 | 0.4 | 1.00 | 0.76 | 0.0009 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


