Evaluation of Prosthetic Valves
Jose A. Madrazo
High-Yield Concepts
Whenever possible, know the type, size, and age of the prosthesis being evaluated.
Serial echocardiographic evaluation of prosthetic valves should be referenced to a baseline study performed early after implantation.
High gradients across a valve may be due to:
Valve dysfunction/obstruction
Increased flow:
Regurgitation
High output states
Patient-prosthesis mismatch
The ultrasound beam cannot penetrate the dense material of prosthetic valves. Multiple views are required to allow the beam to interrogate chambers without interference from prosthesis-related artifact. In patients with multiple prosthetic valves, TEE is often necessary if clinical suspicion of prosthetic valve dysfunction is high.
Key Points
The following should raise concern for severe prosthesis malfunction:
Aortic valves:
Stenosis
Peak velocity >4 m/s
Mean gradient >35 mmHg
LVOT/AoV velocity or VTI ratio <0.25
Aortic acceleration time >100 ms (rounded velocity contour)
Regurgitation
Regurgitant jet width ≥65% of LVOT (at Nyquist limit = 50 to 60 cm/s)
Dense regurgitant jet with PHT <200 ms
Regurgitant volume >60 mL/beat; regurgitant fraction >50%
LVOT TVI ≫ RVOT TVI
Prominent holodiastolic flow reversal in the descending aorta
Mitral valves:
Stenosis
Peak velocity ≥2.5 m/s
Mean gradient >10 mmHg
MV inflow PHT >200 ms
Regurgitation
Dense early, peaking jet (triangular)
EROA ≥0.5 cm2
Regurgitant jet of ≥8 cm2 area
Vena contracta ≥0.6 cm
Regurgitant volume ≥60 mL/beat; regurgitant fraction >50%
Pulmonary vein systolic flow reversal in one or more veins
MV/LVOT TVI ratio >2.5
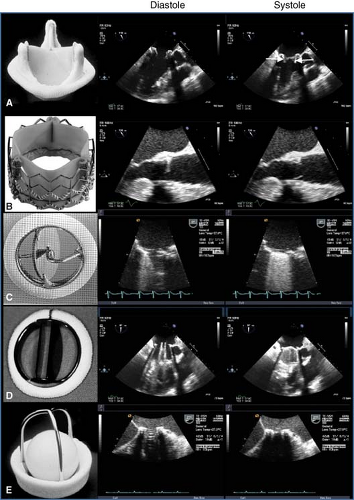
The echocardiographic evaluation of prosthetic valves is a challenging task as there are many different types of prostheses and they frequently impart imaging artifacts and shadowing (Fig. 13-1).
Understanding the types of valves available helps determine the expected appearance, gradients, and physiologic regurgitation.
Valves are generally divided into bioprosthetic or mechanical.
Bioprosthetic valves may be stented (higher profile), stentless, homografts, or heterografts.
Mechanical valves may be ball-cage or tilting disk (single or double).
Regurgitation
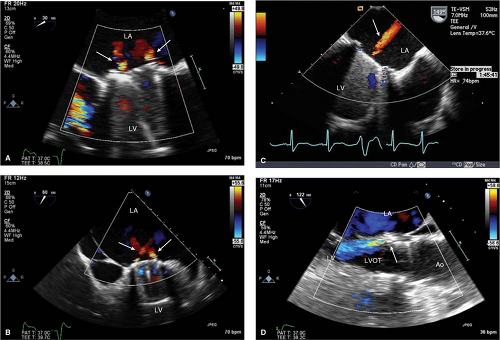
Most mechanical valves will have some built in “physiologic” regurgitation (Fig. 13-2). Knowing the type of valve will help determine the expected pattern of regurgitation. Some common examples:
Bileaflet tilting disk valves will have two small lateral (and one small central for St. Jude’s) jets of regurgitation that are angled inward.
Single tilting disk valves will have a central area of regurgitation around the hinge-point (that is larger than what is seen in bileaflet valves).
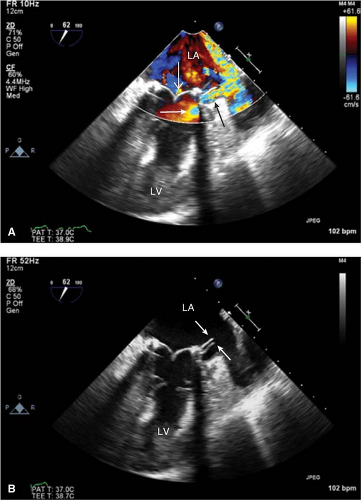
Perivalvular leak (typically unilateral, eccentric, turbulent jet) is in contrast pathologic (Fig. 13-3) and occurs most often in redo valve replacement surgery or when extensive calcium debridement is required prior to valve implantation (newer percutaneously inserted valves will not uncommonly have a small perivalvular regurgitant jet).
Start your evaluation by identifying the valve and confirming the expected appearance. Look for stability of the valve and ring. Excessive movement of the entire prosthesis (“rocking”) suggests dehiscence. Evaluate leaflet/disk motion when they are visible. Pay attention to the presence of calcifications, thrombi, or vegetations.
Prosthetic valves will cause shadowing distal to the ultrasound beam and make those areas difficult to inspect visually. Standard and off-axis views should be selected to interrogate areas of interest first and then the prosthesis to minimize shadowing (e.g., for evaluating MR for a mitral prosthesis the PLAX and subcostal images can visualize the LA without significant artifact compared to the apical four-chamber view). TEE is often necessary when clinical suspicion of prosthetic valve dysfunction is high especially when multiple prostheses are present (Fig. 13-4).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree