Great interest has focused on pharmacotherapy to prevent periprocedural myocardial injury during elective percutaneous coronary intervention (PCI). The aim of the present trial was to investigate the benefits of preprocedural intracoronary administration of high-dose adenosine during elective PCI. This was a single-center, double-blind, randomized trial of patients undergoing elective PCI. The patients were randomized (1:1) by sealed envelops to intracoronary adenosine (120 μg for the right coronary artery and 180 μg for the left coronary artery) or placebo. The primary study end point was a periprocedural increase in troponin I >3 times the upper limit of normal. The secondary study end points were (1) the corrected Thrombolysis In Myocardial Infarction frame count; (2) troponin I release >10 times the upper limit of normal; (3) creatine kinase-MB mass release ≥3 times the upper limit of normal; and (4) the combined cumulative incidence of in-hospital death, periprocedural myocardial infarction, and in-hospital urgent target vessel revascularization. The safety end point was the occurrence of bradycardia and ventricular arrhythmias during study drug administration. From November 2009 to September 2010, we randomized 260 patients who were undergoing elective PCI to intracoronary adenosine (n = 130) or placebo (n = 130). A greater prevalence of calcified lesions was observed in the adenosine group (p = 0.002). In contrast, a greater prevalence of type C lesions (p = 0.091), chronic occlusions (p = 0.015), worse preprocedural Thrombolysis In Myocardial Infarction flow (p = 0.038), and more severely stenotic lesions (p = 0.005) were observed in the placebo group. No difference was found in the primary (67.7% vs 70%, p = 0.69) or secondary end points. No serious side effects were observed with adenosine. In conclusion, our randomized trial showed that preprocedural intracoronary administration of a single high-dose bolus of adenosine does not provide any benefit in terms of periprocedural myonecrosis in patients undergoing elective PCI.
Owing to several achievements in the past decades, coronary angioplasty currently represents the most used revascularization strategy in patients with coronary artery disease. However, percutaneous coronary intervention (PCI) is associated with a 30% occurrence of periprocedural myocardial necrosis, owing to several factors, including occlusions of side branches, coronary spasm, and distal embolization. A study has shown that pretreatment with selective intracoronary administration of adenosine might reduce the infarct size and improve survival in patients undergoing primary angioplasty. A recent study has shown that in patients undergoing elective coronary angioplasty, pretreatment with intracoronary adenosine prevents the risk of periprocedural myocardial infarction (MI). However, the dosage was relatively low (30 to 60 μg). It has been shown to have greater vasodilator effects on the microcirculation with a higher dosage (120 to 150 μg). Therefore, the aim of the present randomized trial was to evaluate the adjunctive benefits of high-dose intracoronary adenosine administration compared to placebo in patients undergoing elective PCI.
Methods
This was a single-center, double-blind, randomized trial (trial registration at Clinicaltrials.gov NCT01148147 ). Patients undergoing elective coronary angioplasty were randomly assigned (1:1) through sealed envelops to intracoronary administration of placebo or adenosine through the guiding catheter ( Figure 1 ) . All patients provided informed consent before the procedure. Our local ethical committee approved the study. The exclusion criteria were marked bradycardia (<40 beats/min); previous allergy to adenosine; inability or refusal to sign the informed consent form; asthma; elevated cardiac enzymes (troponin I or creatine kinase [CK]-MB). Open-label randomization was performed in the catheterization laboratory before angioplasty by the treating physician when the eligibility criteria were met. We used a computer-generated random permutation of a string of 260 treatment arm assignments consisting of 130 of each type (randomization 1:1), without blocking or stratification. The randomization process and preparation of the sealed envelopes containing information on the type of treatment provided to the patient (adenosine or placebo) was prepared by 2 residents who were not otherwise involved in the study. After knowing the treatment arm, a nurse not involved in the revascularization procedure prepared the adenosine (diluted to 10 ml with 0.9% NaCl solution at a concentration of 60 μg/ml) or placebo (10 ml of a 0.9% NaCl solution), both contained in a 10-ml syringe. Coronary angioplasty was performed using standard techniques. The use of stents, stent type, stent implantation techniques, rotational atherectomy, intravascular untrasound, and glycoprotein IIb/IIIa inhibitors was left to the discretion of the operators. All patients received, according to the guidelines, a high-dose bolus of clopidogrel (600 mg) at hospitalization or before angioplasty. The intracoronary administration of the study drug (adenosine) was through the guiding catheter at a dose of 120 μg (right coronary artery) or 180 μg (left coronary artery), just before crossing the lesion with the wire. In the case of a chronically occluded vessel, randomization was performed after initial successful dilation, with a Thrombolysis In Myocardial Infarction (TIMI) flow of ≥2. Cardiac enzymes were measured at 6, 12, and 24 hours after the procedure. The patients were clinically followed up to hospital discharge.
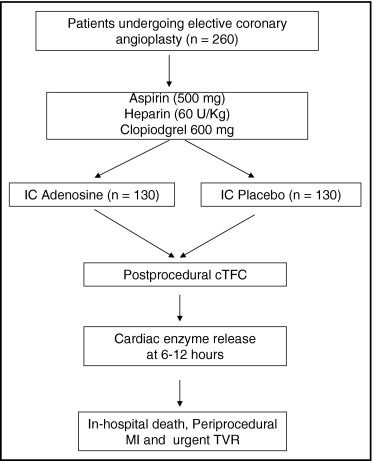
The primary study end point was periprocedural myonecrosis, defined as an increase (peak value) in troponin I ≥3 times the upper limit of normal (ULN). The secondary study end points were angiographic coronary flow, as evaluated by the corrected TIMI frame count ; troponin I release (peak value) ≥10 times the ULN; periprocedural MI defined as CK-MB mass release (peak value) ≥3 times the ULN; and the cumulative incidence of in-hospital death, periprocedural MI, and in-hospital urgent target vessel revascularization. The safety end point was the occurrence of bradycardia and ventricular arrhythmias during study drug administration. All the events were reviewed and adjudicated by 2 experienced cardiologists not involved in the study.
Statistical analysis was performed using the Statistical Package for Social Sciences, version 15.0 (SPSS, Chicago, Illinois). Continuous data are expressed as the mean ± SD and categorical data as percentages. Analysis of variance and the chi-square test (or Fisher exact test) were used for continuous and categorical variables, respectively. In the case of statistically significant differences (p <0.05) between the 2 groups in the baseline demographic, clinical, or angiographic characteristics, the results were adjusted for those differences using multiple regression analysis, with the variables of interest included in block in the regression model.
According to an expected 15% absolute reduction (60% relative reduction) in the incidence of periprocedural myonecrosis with intracoronary adenosine compared to placebo (from 25% to 10%), with an anticipated 2-sided test for differences in independent binomial proportions at 5.0% and a statistical power of 80%, a total 112 patients per group were needed. To avoid any effects from patient withdrawal, the enrollment was extended to 130 patients for each group.
Results
From November 2009 to September 2010, 260 of 395 patients undergoing elective coronary angioplasty were randomized to intracoronary adenosine (n = 130) or placebo (n = 130). The patients were ineligible to randomization mostly because of elevated cardiac enzymes at the procedure (n = 132).
The patient characteristics are reported in Table 1 . Similar baseline characteristics were observed in the 2 groups, except for a greater prevalence of calcified lesions in the adenosine group (p = 0.002) and a greater prevalence of type C lesions (p = 0.091), chronic occlusions (p = 0.035), worse preprocedural TIMI flow (p = 0.038), and more severely stenotic lesions (p = 0.005) in the placebo group ( Table 2 ).



