Evaluation and Treatment of Femoral Pseudoaneurysms
R. Eugene Zierler
Watson B. Smith
An arterial aneurysm is generally defined as a focal dilatation that involves either the whole or a part of the vessel circumference. In true aneurysms, the dilatation includes all layers of the arterial wall, and flowing blood is entirely contained within the vessel lumen. With false aneurysms or pseudoaneurysms, there is a defect in the arterial wall, and blood flows outside the arterial lumen but is contained by the perivascular tissues. A dissecting aneurysm is a dilatation of an artery associated with penetration of blood into the layers of the arterial wall. Table 32.1 presents a classification of arterial aneurysms by etiology. Pseudoaneurysms typically result from disruption of the arterial wall related to blunt or penetrating trauma, open surgical procedures, or percutaneous arterial interventions. One common mechanism for pseudoaneurysms is a gradual breakdown of the anastomosis between a prosthetic graft and a native artery. These anastomotic pseudoaneurysms typically involve the common femoral, deep femoral, or proximal superficial femoral arteries and have been found in 2% to 5% of patients undergoing aortofemoral or femoropopliteal bypass grafting.1,2 The incidence of femoral pseudoaneurysms related to percutaneous arterial puncture is increasing owing to the use of groin artery catheterization for cardiac, peripheral arterial, and carotid interventions.
CLINICAL PRESENTATION
With the growing emphasis on “minimally invasive” treatment of cardiovascular diseases, there has been a marked increase in the use of percutaneous diagnostic and therapeutic procedures. The most frequently used arterial access site is the common femoral artery, and the reported prevalence of femoral pseudoaneurysms is in the range of 0.05% to 4%.3,4,5 Some devices for catheter-based interventions require large sheath sizes as well as aggressive use of anticoagulants and antiplatelet agents; these factors appear to increase the risk for pseudoaneurysms. The method used to achieve hemostasis after sheath removal may also contribute to this risk. These developments have increased the incidence of other complications related to percutaneous femoral artery puncture, including groin hematomas, retroperitoneal bleeding, and arteriovenous fistulas.
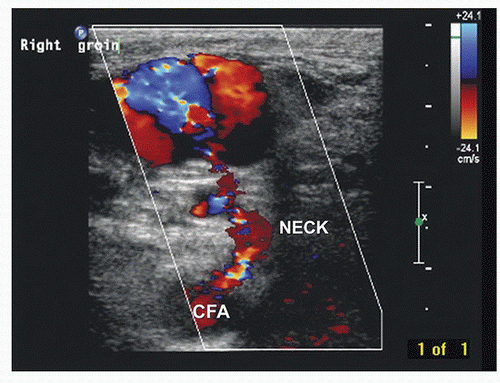
Femoral pseudoaneurysms usually originate at the arterial puncture site from the wall of the artery closest to the skin surface. This is most often at the level of the common femoral artery but may involve any segment from the distal external iliac to the proximal superficial femoral or deep femoral artery. A pseudoaneurysm forms when the puncture site fails to seal and a cavity filled with arterial blood forms adjacent to the arterial wall. This cavity is connected to the arterial lumen by a “neck” of variable length and often contains both flowing blood and laminated thrombus (Fig. 32.1). Pseudoaneurysm cavities are typically in the range of 1 to 3 cm in diameter when first detected, and some consist of multiple interconnected lobes. Rarely, a femoral pseudoaneurysm is associated with an arteriovenous fistula originating from a separate puncture site. Although the natural history of femoral pseudoaneurysms is unpredictable, those with flow-filled cavities less than 2 cm in maximum diameter are more likely to thrombose spontaneously than are those with larger cavities.
A femoral pseudoaneurysm should be suspected whenever an enlarging hematoma is noted adjacent to a puncture site within hours to days after a percutaneous arterial procedure. Many patients report a “popping” sensation and pain in the catheterized groin. These signs and symptoms are typically accompanied by extensive ecchymosis of the overlying skin; however, bruising is common in this setting, even in the absence of a pseudoaneurysm. A palpable thrill or continuous bruit over the groin suggests the presence of an arteriovenous fistula, with or without an associated pseudoaneurysm. Palpation usually reveals a tender pulsatile mass, but it is often difficult to distinguish between true pulsatility and transmitted pulsation through a hematoma. Therefore, the diagnosis should always be confirmed by duplex ultrasound evaluation.
DIAGNOSIS
Scanning Technique
With the patient supine and the ipsilateral leg externally rotated, initially evaluate the distal external iliac, common femoral, deep femoral, and proximal superficial femoral arteries and veins in a standard fashion for stenosis, aneurysm, or thrombosis. This is typically done with a 5- to 7-MHz linear array
transducer. However, B-mode resolution is often poor owing to extravasated blood in the tissue, and a lower-frequency transducer may be needed for adequate depth penetration. A curved array is useful if a large field of view is required, whereas a phased array is best if there is a small acoustic window or deep inguinal crease. After the native vessels have been assessed, scan the surrounding area for masses. Color-flow imaging is helpful for distinguishing between pseudoaneurysms and nonvascularized masses such as hematomas, seromas, or enlarged lymph nodes. Although pseudoaneurysms are the most frequently suspected postcatheterization vascular problem, other abnormalities that may be present include intimal flaps, arterial thrombosis, arterial dissections, arteriovenous fistulas, extrinsic compression of veins, and deep vein thrombosis.
transducer. However, B-mode resolution is often poor owing to extravasated blood in the tissue, and a lower-frequency transducer may be needed for adequate depth penetration. A curved array is useful if a large field of view is required, whereas a phased array is best if there is a small acoustic window or deep inguinal crease. After the native vessels have been assessed, scan the surrounding area for masses. Color-flow imaging is helpful for distinguishing between pseudoaneurysms and nonvascularized masses such as hematomas, seromas, or enlarged lymph nodes. Although pseudoaneurysms are the most frequently suspected postcatheterization vascular problem, other abnormalities that may be present include intimal flaps, arterial thrombosis, arterial dissections, arteriovenous fistulas, extrinsic compression of veins, and deep vein thrombosis.
TABLE 32.1 CLASSIFICATION OF ARTERIAL ANEURYSMS BY ETIOLOGY | ||
|---|---|---|
|
Ultrasound Findings
The key features of a pseudoaneurysm on duplex ultrasound are a vascularized cavity connected to the adjacent artery by a neck that exhibits a characteristic “to-and-fro” spectral waveform pattern, representing arterial flow in and out of the pseudoaneurysm (Fig. 32.2). Radial pulsations are usually visible in or around the cavity on B-mode imaging, and arterial flow is detectable within the cavity by both pulsed and color-flow Doppler. A distinctive “yin-yang” pattern is often seen on the color-flow image (Fig. 32.3). Document the size and location of the pseudoaneurysm, and follow the neck to locate the exact point of origin. Also measure the length of the neck between the arterial defect and the vascularized cavity. Whereas the true size of a pseudoaneurysm includes both the active or vascularized portion and any surrounding thrombus, the most important feature is the size of the vascularized cavity. Images and reports should clearly distinguish between these measurements.
Arteriovenous fistulas occur when both the artery and the adjacent vein have been punctured, resulting in a persistent high-flow connection between the two vessels. These lesions usually produce a striking image on color-flow Doppler in the area of the communicating channel, with a prominent “color bruit” (Fig. 32.4). Elevated peak velocities and aliasing are typically found at the site of the fistula, with a characteristic high-velocity/low-pulsatility waveform (Fig. 32.5). Arteriovenous fistulas can also be located by identifying increased systolic and diastolic velocities in the artery proximal to the lesion that normalize distally (Fig. 32.6). Venous segments proximal (central) to the fistula contain turbulent and pulsatile flow patterns (Fig. 32.7).
APPROACHES TO TREATMENT
Based on the risk of progressive enlargement and rupture, most pseudoaneurysms should be treated at the time of diagnosis. However, small asymptomatic pseudoaneurysms with
vascularized cavities less than 2 cm in diameter may be followed by serial ultrasound evaluations and treated if they do not thrombose spontaneously. Patients on antiplatelet agents or anticoagulants are less likely to show spontaneous thrombosis. Options for treatment include direct open surgical repair, ultrasound-guided compression, and ultrasound-guided thrombin injection. Open surgery requires exposure of the puncture site through a groin incision and direct repair of the arterial defect by simple suture or patch angioplasty. Any concomitant arterial defects such as intimal flaps or fistulas can also be repaired using this approach. Although direct surgical repair is highly effective and relatively safe, many patients with femoral pseudoaneurysm have significant medical comorbidities that make a less invasive approach preferable.
vascularized cavities less than 2 cm in diameter may be followed by serial ultrasound evaluations and treated if they do not thrombose spontaneously. Patients on antiplatelet agents or anticoagulants are less likely to show spontaneous thrombosis. Options for treatment include direct open surgical repair, ultrasound-guided compression, and ultrasound-guided thrombin injection. Open surgery requires exposure of the puncture site through a groin incision and direct repair of the arterial defect by simple suture or patch angioplasty. Any concomitant arterial defects such as intimal flaps or fistulas can also be repaired using this approach. Although direct surgical repair is highly effective and relatively safe, many patients with femoral pseudoaneurysm have significant medical comorbidities that make a less invasive approach preferable.
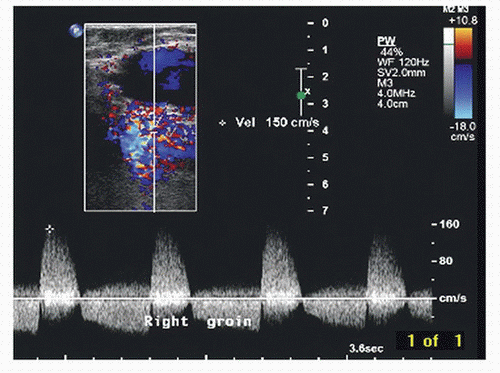 FIGURE 32.2. Pulsed Doppler spectral waveform shows the typical “to-and-fro” flow pattern found in a pseudoaneurysm neck. Note both forward (positive) and reverse (negative) velocity components.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|