Essential Echocardiographic Images in Adult Congenital Heart Disease
Congenital heart disease is by definition an abnormality in cardiac structure that is present at birth, even if it is not diagnosed until later in life. These defects are usually the result of altered embryonic development of a normal structure or failure of development. Four categories of etiologic agents may be responsible for this abnormal development, and these are the same influences that may cause cancers. They include hereditary and chromosomal defects (Table 24.1), viruses (rubella with patent ductus arteriosus [PDA]), chemicals (thalidomide with truncus arteriosus or tetralogy of Fallot), and radiation (x-irradiation with ventricular septal defects [VSDs]). Although these agents cause certain known defects, most defects have no specific cause and the etiology may in fact be multifactorial. The incidence of congenital heart disease (excluding bicuspid aortic valve and myxomatous mitral valve (MV) disease with mitral valve prolapse [MVP]) is approximately 0.5% to 0.8% of live births. Congenital cardiac malformations are much more common in stillbirths than in live births. Some congenital lesions have a high rate of survival without surgery and may be seen in the unoperated adult with different relative frequencies (Table 24.2). Other lesions, with worse prognosis, are usually not seen in adults. However, as both diagnosis and treatment (both medical and surgical) improve, more of these patients are surviving into adulthood and are more likely to be seen in a cardiology office as adults. Thus, all cardiologists should be familiar with the lesions discussed in this chapter.
TABLE
24.1 Chromosomal Anomalies and Their Congenital Syndromes Associated with Heart Defects
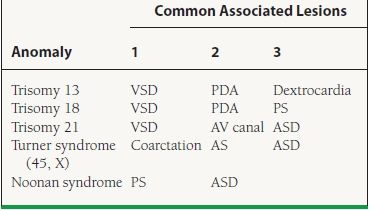
VSD, ventricular septal defect; PDA, patent ductus arteriosus; PS, pulmonic stenosis; AV atrioventricular; AS, aortic stenosis; ASD, atrial septal defect.
TABLE
24.2 Congenital Heart Defects in the Unoperated Adult
ATRIAL SEPTAL DEFECTS
Atrial septal defect (ASD) accounts for 22% of adult congenital defects. Excluding bicuspid aortic valves and MVP, ASDs are the most common form of adult congenital heart disease. They make up 10% of all congenital heart defects and demonstrate a female-to-male preponderance of 3:2. Diagnosis of ASD is aided by the following features:
 On auscultation, a wide fixed split S2 with a pulmonary flow murmur is heard.
On auscultation, a wide fixed split S2 with a pulmonary flow murmur is heard.
 On electrocardiogram (ECG), ostium primum (OP) ASD shows marked left-axis or right bundle branch block (RBBB) with signs of right ventricular (RV) enlargement. There may be first-degree atrioventricular (AV) block. Ostium secundum (OS) ASD is marked by RSR or rSR in V1, QRS <0.11 seconds, right axis deviation, right ventricular hypertrophy (RVH), and possibly first-degree AV block and right atrial enlargement (RAE).
On electrocardiogram (ECG), ostium primum (OP) ASD shows marked left-axis or right bundle branch block (RBBB) with signs of right ventricular (RV) enlargement. There may be first-degree atrioventricular (AV) block. Ostium secundum (OS) ASD is marked by RSR or rSR in V1, QRS <0.11 seconds, right axis deviation, right ventricular hypertrophy (RVH), and possibly first-degree AV block and right atrial enlargement (RAE).
 Shunt can be visualized by echocardiography with color Doppler and agitated saline contrast.
Shunt can be visualized by echocardiography with color Doppler and agitated saline contrast.
 Shunt at the atrial level is a potential source of paradoxical embolus.
Shunt at the atrial level is a potential source of paradoxical embolus.
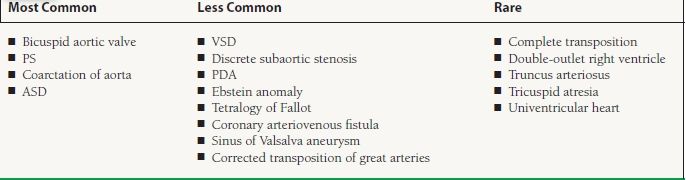
The locations of types of ASD are shown in Figure 24.1. The four types of ASD are:
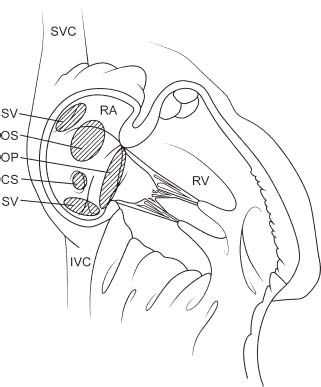
FIGURE 24.1 Location of types of ASD. SV, sinus venosus ASD; OP, ostium primum ASD; OS, ostium secundum ASD; CS, coronary sinus ASD.
 Primum ASD
Primum ASD
 Secundum ASD
Secundum ASD
 Sinus venosus (SV)
Sinus venosus (SV)
 Unroofed coronary sinus (CS)
Unroofed coronary sinus (CS)
Primum Atrial Septal Defect
Primum ASD accounts for 20% of cases of ASD (Fig. 24.2A–C) and is part of an AV canal defect in which embryonic endocardial cushions fail to meet normally and partition the heart (Figs. 24.3 and 24.4).
FIGURE 24.2 A: Apical four-chamber view of a patient with AV canal defect. Note the primum ASD (arrow) and the dilated right side. B: Magnified apical four-chamber view with color Doppler demonstrating the left-to-right flow (arrow) across the primum ASD. C: Parasternal short axis-view demonstrating the cleft anterior mitral leaflet with a gap (arrow) representing the cleft in the anterior mitral leaflet (AML).
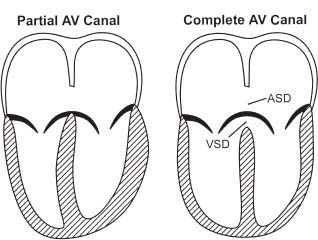
FIGURE 24.3 Apical four-chamber view of partial AV canal defect (left) and complete AV canal defect (right). The partial AV canal defect has a primum ASD, cleft MV, and widened anteroseptal tricuspid commissure. The complete AV canal defect has all of these and a VSD.
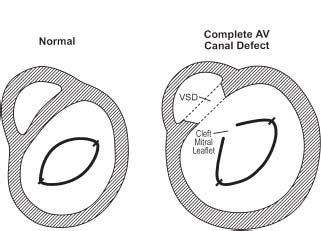
FIGURE 24.4 Parasternal short-axis view showing complete AV canal defect (right) compared to a normal heart (left). Note the cleft anterior mitral leaflet and VSD in the complete AV canal defect.
A complete AV canal defect consists of four components:
 Inlet VSD
Inlet VSD
 Primum ASD
Primum ASD
 Cleft MV
Cleft MV
 Widened anteroseptal tricuspid commissure
Widened anteroseptal tricuspid commissure
A partial AV canal defect is as above without the VSD.
Secundum ASD is an ASD at the fossa ovalis (Fig. 24.5A–D). It is the most common form of ASD (75% of cases). The following features distinguish a secundum ASD:
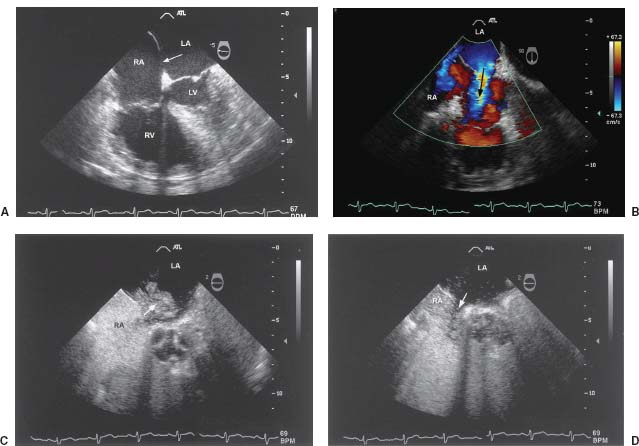
FIGURE 24.5 A: Four-chamber midesophageal view of a TEE demonstrating a secundum ASD (arrow). B: TEE with color Doppler demonstrating the left-to-right flow across the secundum ASD. Note that although there is one larger shunt, there are multiple defects with shunting through the atrial septum. C: TEE with agitated saline contrast demonstrating the intermittent right-to-left shunting across the secundum ASD. D: TEE with agitated saline contrast demonstrating the intermittent left-to-right shunting across the secundum ASD and the unopacified blood from the left side of the heart (specifically the leftatrium [LA]) displacing the contrastwithin the RA. The combination of this image and the prior image demonstrates the bidirectional shunting across this ASD.
 Left-to-right shunt, because the right ventricle (RV) is thin walled and fills more easily than the left ventricle and pulmonary vascular resistance is lower than systemic
Left-to-right shunt, because the right ventricle (RV) is thin walled and fills more easily than the left ventricle and pulmonary vascular resistance is lower than systemic
 Pulmonary blood flow is often two to four times normal.
Pulmonary blood flow is often two to four times normal.
 Dilated right side due to right atrial (RA) and RV volume overload
Dilated right side due to right atrial (RA) and RV volume overload
 The pulmonary artery (PA) is often dilated.
The pulmonary artery (PA) is often dilated.
Sinus Venosus Atrial Septal Defect
Sinus venosus ASD accounts for 5% of ASD (Fig. 24.6). The following are typical features:

FIGURE 24.6 Bicaval TEE view with color Doppler demonstrating a sinus venosus ASD with left-to-right shunting. This ASD is located near the connection between the SVC and the RA.
 Defect near the junction of the superior vena cava (SVC) or the inferior vena cava (IVC) with the RA (posterior to fossa ovalis)
Defect near the junction of the superior vena cava (SVC) or the inferior vena cava (IVC) with the RA (posterior to fossa ovalis)
 Often difficult to detect (typically requires transesophageal echocardiography [TEE])
Often difficult to detect (typically requires transesophageal echocardiography [TEE])
 If unexplained right-sided dilatation is seen on the echocardiogram, echocardiography should be performed with agitated saline contrast to look for a shunt, with follow-up TEE if needed.
If unexplained right-sided dilatation is seen on the echocardiogram, echocardiography should be performed with agitated saline contrast to look for a shunt, with follow-up TEE if needed.
 Superior sinus venosus ASD is almost always associated with partial anomalous pulmonary venous (PV) return: right PV to either SVC or high RA.
Superior sinus venosus ASD is almost always associated with partial anomalous pulmonary venous (PV) return: right PV to either SVC or high RA.
Coronary Sinus Atrial Septal Defect
Coronary sinus ASD is very rare. A distinguishing feature is that the roof of the CS is absent.
VENTRICULAR SEPTAL DEFECT
VSD is the most common form of congenital abnormality at birth but accounts for only 10% cases of congenital heart disease in adults (Fig. 24.7). Distinguishing features include the following:
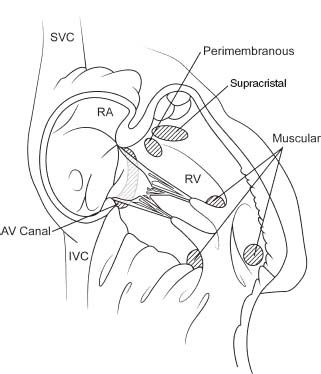
FIGURE 24.7 Locations of types of VSD: membranous, muscular (may be multiple), supracristal, or “subpulmonic” AV canal defects.
 At least 50% to 80% of VSDs close spontaneously.
At least 50% to 80% of VSDs close spontaneously.
 Perimembranous VSD is the most common form of VSD.
Perimembranous VSD is the most common form of VSD.
 VSD carries a risk of endocarditis.
VSD carries a risk of endocarditis.
 Perimembranous VSD is often associated with a ventricular septal aneurysm formed by septal leaflet of tricuspid valve (TV) closing defect (the defect may be larger than appears).
Perimembranous VSD is often associated with a ventricular septal aneurysm formed by septal leaflet of tricuspid valve (TV) closing defect (the defect may be larger than appears).
 Restrictive VSDs have high-velocity jets with a large pressure difference between the right and left ventricles (larger defects are associated with a low-velocity jet). Recall the modified Bernoulli equation: ΔP = 4V2.
Restrictive VSDs have high-velocity jets with a large pressure difference between the right and left ventricles (larger defects are associated with a low-velocity jet). Recall the modified Bernoulli equation: ΔP = 4V2.
Types of VSDs include the following:
 Membranous VSD: accounts for 80% of cases of congenital VSD, has the highest rate of spontaneous closure (Fig. 24.8A,B)
Membranous VSD: accounts for 80% of cases of congenital VSD, has the highest rate of spontaneous closure (Fig. 24.8A,B)
 Muscular VSD: accounts for 10% of VSD and may be multiple (Fig. 24.9)
Muscular VSD: accounts for 10% of VSD and may be multiple (Fig. 24.9)
 Supracristal VSD: accounts for 5% of VSD (Fig. 24.10A,B), involves left ventricular outflow track (LVOT)/right ventricular outflow track (RVOT), and carries a high incidence of aortic insufficiency (AI) due to prolapse of right coronary cusp (RCC) or left coronary cusp (LCC) into the VSD
Supracristal VSD: accounts for 5% of VSD (Fig. 24.10A,B), involves left ventricular outflow track (LVOT)/right ventricular outflow track (RVOT), and carries a high incidence of aortic insufficiency (AI) due to prolapse of right coronary cusp (RCC) or left coronary cusp (LCC) into the VSD
 AV canal defect: discussed in relation to ASD
AV canal defect: discussed in relation to ASD
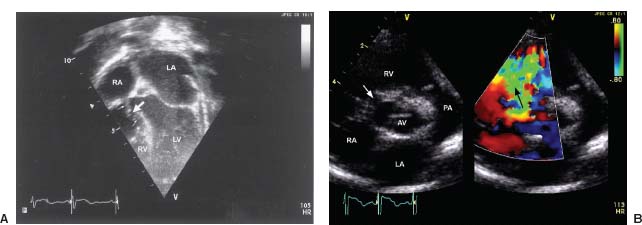
FIGURE 24.8 A Inverted apical four-chamber view (pediatric convention) demonstrating a perimembranous VSD with a ventricular septal aneurysm formed as the septal leaflet of the TV attempts to close the defect. The big arrow denotes the VSD and the region enclosed by the smaller arrows demonstrates the extent of the ventricular septal aneurysm. B: Parasternal short-axis views (two-dimensional (2-D) images on the left and color Doppler images on the right) demonstrate a perimembranous VSD with a 2-D defect noted near the RV inflow region near the TV, with left-to-right shunting seen in that location.
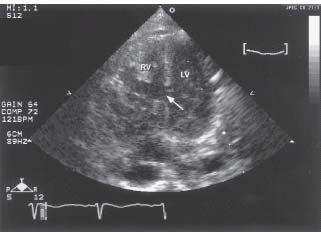
FIGURE 24.9 Apical four-chamber view demonstrating a large muscular VSD in the midseptum. Note the dilated right side as a result of long-term left-to-right shunting and right-sided volume overload.
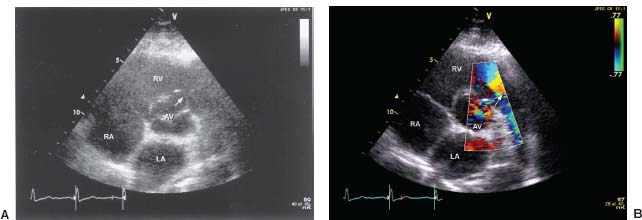
FIGURE 24.10 A: Parasternal short-axis view demonstrating the 2-D defect of a supracristal VSD located near the RVOT. B: Parasternal short-axis view with color Doppler demonstrating a fine jet of left-to-right flow through the supracristal VSD.
BICUSPID AORTIC VALVE
Bicuspid aortic valve occurs in 1% to 2% of the general population. The most common form is a fusion of the RCC and the LCC. Congenital abnormalities of aortic cusp anatomy are shown in Figure 24.11A–G. Characteristics of bicuspid aortic valve include the following:
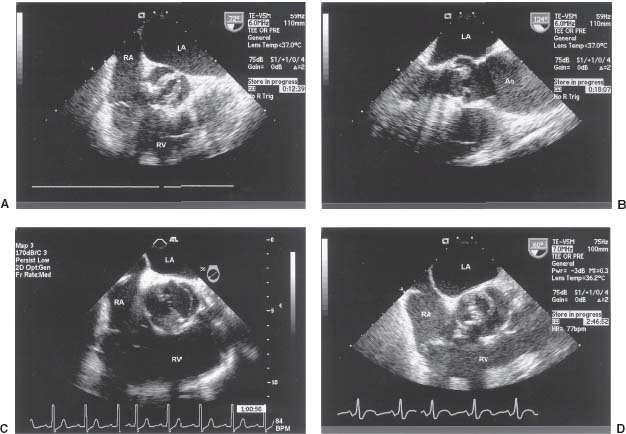
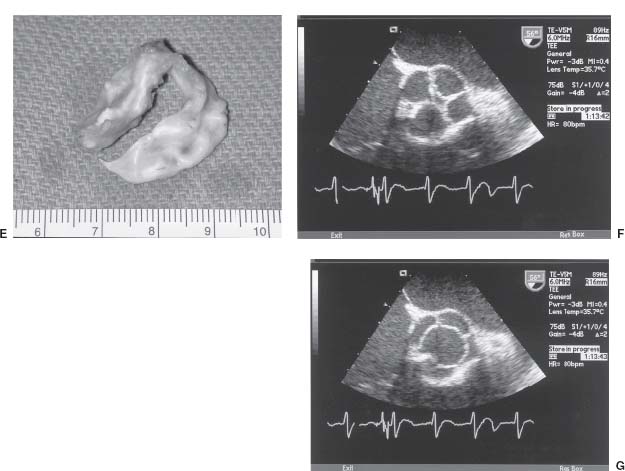
FIGURE 24.11 A: Midesophageal short-axis view of the aortic valve demonstrating a bicuspid aortic valve with fusion of the right coronary cusp (RCC) and the left coronary cusp (LCC). The leaflets are somewhat thickened and there is a combination of aortic regurgitation as well as a component of stenosis. B: Long-axis midesophageal view demonstrating doming of a bicuspid aortic valve. Because of the significant leaflet doming, it is very important to obtain an on-axis, short-axis view. Off-axis images may cause overestimation of a planimetered aortic valve area (therefore underestimating the degree of AS). C: Midesophageal short-axis view of the aortic valve demonstrating a bicuspid aortic valve with non-coronary cusp (NCC) and right coronary cusp (RCC) fusion. D: Midesophageal short-axis view of the aortic valve demonstrating a unicuspid aortic valve. Note the eccentric opening with a single commissure at the 11:00 position. E: Gross pathologic specimen of a unicuspid aortic valve. F: Magnified midesophageal short-axis view of the aortic valve demonstrating a quadricuspid valve in diastole. G: Magnified midesophageal short-axis view of the aortic valve demonstrating a quadricuspid valve in systole. Note the presence of four separate cusps.



