9 Epiaortic Ultrasonography and Epicardial Echocardiography
Surface Imaging
Probe Orientation
Probe orientation marker is important for surface imaging techniques.
• Conventional imaging planes are based on transthoracic echocardiography (TTE), because orientation is most similar to TTE windows. As with transesophageal echocardiography (TEE), images on the left side of the monitor screen are on the patient’s right and images on the right side are on the patient’s left.
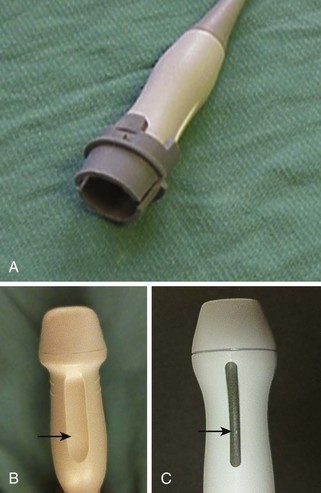
• The probe marker is a raised line, indentation, or mark on the probe (Figure 9-1). It is easily hidden by the standoff in the sheath. Thus, alternative methods to identify orientation are frequently needed.
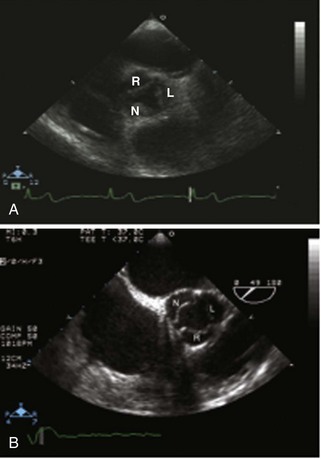
• Images will appear left to right inverted if probe orientation is incorrect (Figure 9-2). Imaging the left ventricle (LV) in reverse could lead to misdiagnosis of regional wall motion abnormalities. An incorrect diagnosis of dextrocardia could be made if images are inverted.
• Within a given image sector, structures progressively appear from anterior (near-field) to posterior (far-field), as opposed to TEE views that start posterior and progress anterior. For example, on epicardial imaging, the right coronary cusp of the aortic valve will be closest to the transducer instead of farthest away (Figure 9-3).
Probe Options
• Use a probe that provides a transducer frequency of at least 7.5 MHz. Standard TTE probes are no more than 5 MHz, so a dedicated probe is needed. Pediatric TTE probes have higher resolution than equivalent adult probes.
• Linear array probes are typically used for central venous access and work well for epicardial echocardiography (ECE) imaging.
• Image depth is rarely greater than 12 cm for ECE examinations, whereas the optimal depth for epiaortic ultrasound (EAU) is often in the range of 8 cm. Surrounding structures can be used to confirm proper probe orientation.
• Images for all EAU and ECE studies should be acquired at the highest possible resolution. ECE images of the mitral valve (MV), in particular, may not have as high a resolution as the corresponding TEE images.
• A standoff is strongly recommended for EAU examinations with a phased array probe. Most manufacturers do not sell a standoff for phased array, but the hard plastic or rubber component of a disposable airway circuit reservoir bag can be used on some probes.
Image Acquisition and Optimization
• The images are acquired through an open chest; vigilance is necessary to avoid disturbing the surgical field; and sterile procedure skills are mandatory.
• The probe marker for the phased array transducer cannot be seen easily through the sterile sheath. Therefore, the probe should be marked or on-screen imaging can be used to guide orientation.
• Orientation for the linear array probe can be determined by tapping on one end of the probe while simultaneously reviewing the screen to first determine which side is medial or lateral and then reorienting as needed.
• Artifacts may be present on EUA and ECE images similar to TTE and TEE and other surface ultrasound-based images.
• Filling the chest cavity with warm (body temperature) saline can improve imaging and decrease artifacts, especially side lobes. Avoid overly hot or cold saline that can cause arrhythmias or hypertension.
• Linear array probes have a narrow imaging sector that limits simultaneously viewing of the full width and depth of the adult aorta. Therefore, the examination should be performed twice, once with adequate depth and once with adequate width.
Maintaining a Sterile Field
• The sterile sheath should be filled with sterile saline or ultrasonic gel by the scrub technician. The echocardiographer at the head of the bed inserts the probe into the sheath opening. The echocardiographer should ensure that the standoff is at an acceptable depth (~1 cm) before inserting the probe (Figure 9-4).
• Air can be trapped in the standoff and will impair optimal image resolution. The probe operator should invert the apparatus under fluid to remove the air.
• Once the examination is complete and the probe is no longer needed, the probe and sheath are removed from the surgical field together before the sheath is discarded.
• Available probes cannot be sterilized to perform these examinations. Therefore, it is important to strictly follow the maintenance instructions provided by the vendor. Probes should not be submersed for long periods of time and should be allowed to dry thoroughly between examinations.
Epiaortic Ultrasonography
Prevention of Stroke
Key Points
• TEE examination of the ascending aorta is not as sensitive or specific as EAU imaging for identifying pathology. A significant portion of the ascending aorta cannot be seen with TEE owing to air-filled bronchi between the esophagus and the aorta, thus preventing ultrasound beam transmission.
• High-grade atherosclerosis of the descending aorta seen on TEE is often associated with an increased risk of ascending aortic disease.
• Cardiac surgical patients are at increased risk of perioperative stroke due to direct manipulation of the ascending aorta and subsequent risk of atherosclerotic embolization.
Standard Views and 12-Segment Nomenclature
Key Points
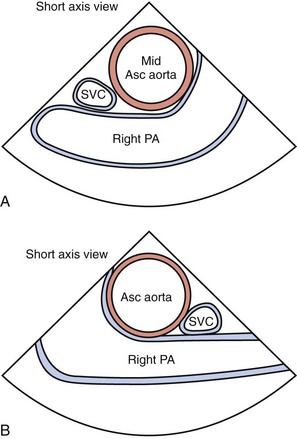
• The ascending aorta is divided into three segments: proximal, mid, and distal. The segment adjacent to the right pulmonary artery (PA) is the mid portion. The proximal segment is from the sinotubular junction (STJ) to the PA. The distal segment is from the PA to the takeoff of the innominate artery (Figure 9-5).
• Each segment of the aorta is then divided into four regions: left, right, anterior, and posterior. The right PA is adjacent to the left side, the superior vena cava (SVC) is adjacent to the right side, the anterior wall is closest to the transducer, and the posterior wall is farthest away.
• Determining the location of atherosclerotic plaques using EAU is critical. The aortic cannula is typically placed in the distal ascending aorta, slightly left of anterior, while the cross-clamp is typically placed at the level of the PA. Thus, the distal left and anterior walls and entire mid segment are key areas of focus during a comprehensive EAU examination.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree