Endovascular Treatment of the SFA (Angioplasty & Stent, Subintimal Angioplasty, Atherectomy)
George H. Meier
Introduction
While limited efforts were made to treat superficial femoral artery atherosclerosis in the early 1900s, it wasn’t until 1948 that Kunlin performed the first vein bypass for superficial femoral artery disease. Working with Leriche and dos Santos in Paris, Kunlin had begun to utilize heparin for vascular surgery and it was in this context that Kunlin performed his bypass. This technique rapidly spread around the world and for the next 40 years surgery for superficial femoral artery atherosclerosis was the standard of care.
An interventional radiologist based in Oregon, Charles Dotter began to experiment with wire-based treatments that did not require surgery. These minimally invasive techniques evolved from the initial treatment in 1964 and are continuing to evolve today. The focus of these treatments is percutaneous access to introduce a device that can leverage and enlarge the arterial lumen to improve blood flow beyond the blockage. While these initial efforts that opening diseased arteries was crewed by today’s standards, it is this basis that has led us to the endovascular revolution of lower extremity treatment.
Endovascular treatment is fundamentally different than conventional surgery. Whereas surgical bypass is designed to reroute blood flow around areas of obstruction or stenosis using an alternative conduit different from the native artery, endovascular treatment relies on the use of the diseased conduit by modifying the stenosis to allow improved distal blood flow. Intrinsically this is quite different from a surgical bypass and the focus is on improving the native artery to a sufficient level to provide distal blood flow.
There is no question that replacing the diseased conduit completely has an intrinsic benefit over the modification of that same conduit in an attempt to improve blood flow. Being able to reset the disease process by surgical bypass is an attractive initial undertaking to modify atherosclerotic plaque that has developed. Unfortunately, as surgical bypass became more commonplace, not only for peripheral vascular disease but also for coronary disease, adequate single segment vein conduit was more and more difficult to
find for bypass surgery. Additionally, the same risk factors associated with peripheral atherosclerosis are also associated with coronary atherosclerosis. As a result, the greatest risk for an operation on a patient with SFA disease is the risk of a coronary event, potentially life-threatening after bypass surgery. Thus, as patients with peripheral vascular disease survive to a more advanced age, the need for endovascular treatment continues to increase due to a lack of autogenous vein conduit and the presence of coronary disease and it was this demand that ultimately fueled the endovascular treatment of lower extremity atherosclerosis. Since the first treatment in 1965, the field of endovascular SFA treatment has exploded with new technologies appearing almost on a daily basis.
find for bypass surgery. Additionally, the same risk factors associated with peripheral atherosclerosis are also associated with coronary atherosclerosis. As a result, the greatest risk for an operation on a patient with SFA disease is the risk of a coronary event, potentially life-threatening after bypass surgery. Thus, as patients with peripheral vascular disease survive to a more advanced age, the need for endovascular treatment continues to increase due to a lack of autogenous vein conduit and the presence of coronary disease and it was this demand that ultimately fueled the endovascular treatment of lower extremity atherosclerosis. Since the first treatment in 1965, the field of endovascular SFA treatment has exploded with new technologies appearing almost on a daily basis.
 Figure 38.1 Trauma to the arterial wall from balloon angioplasty of atherosclerotic plaque. After plaque dissection, a larger lumen results for the plaque healing. |
The main disadvantage of endovascular treatment is in the need to modify the preexisting artery to allow for improved distal flow. Inherently, this results in an injury to the vessel that will require healing for it to be durable (Fig. 38.1). The severity of the injury as well as the extent of the damage can lead to scar tissue formation within the lumen of the artery and it is this intimal hyperplasia that results that ultimately threatens the patency of any endovascular therapy. While vein grafts can suffer from intimal hyperplasia as well, these conduits have already functioned in the venous system efficiently and without thrombus formation in most cases. Therefore the only areas at high risk for intimal hyperplasia in a bypass graft are the anastomoses where trauma is imparted in by the creation of the suture line.
The use of endovascular intervention is generally complementary to that of open surgery. In fact, endovascular treatment has allowed patients with limitations that prevent open surgery to be treated for their SFA disease. Typically, the risk of the surgical procedure as well as the available vein conduit for open surgical treatment colors the judgment relative to endovascular versus open surgery. If the patient is high surgical risk or if autogenous conduit is not readily available, then endovascular treatment may be the preferred method.
Prior to deciding on endovascular treatment of SFA disease many considerations must be examined. First, the patient’s underlying risk of cardiovascular disease has to be factored into the treatment plan. Most patients with significant SFA disease have some degree of cardiovascular atherosclerosis. As a result, treatment of the peripheral vascular disease using open surgical techniques may result in a significant risk for a cardiac event. Generally, endovascular treatment offers a lower cardiovascular risk for the procedure, with some loss of durability since the underlying treatment is inevitably using the diseased artery as a conduit. Nonetheless, endovascular treatment may provide the only feasible therapy in many of the high-risk patients with SFA disease.
Similarly, an autogenous bypass with vein conduit is the gold standard to which endovascular therapy is compared. If single segment vein conduit of adequate caliber is not available, then endovascular treatment again may be favored.
There are very few contraindications for endovascular intervention. Most commonly, limitations in access to the arterial lumen can lead to an inability to treat the lesions found. This is most common when there is an alteration of the aortic bifurcation due to an aortic graft or an aortic endograft. In this situation, the bifurcation is too narrow to allow contralateral femoral access to succeed, limiting the patient to an alternative access
which has a lower chance of success. A careful history of the patient’s prior surgery and interventions on the arterial tree is absolutely crucial to the successful treatment of the vascular patient who often presents with recurrent or residual atherosclerosis. Nonetheless, usually adequate intra-arterial access can be achieved in almost any setting.
which has a lower chance of success. A careful history of the patient’s prior surgery and interventions on the arterial tree is absolutely crucial to the successful treatment of the vascular patient who often presents with recurrent or residual atherosclerosis. Nonetheless, usually adequate intra-arterial access can be achieved in almost any setting.
Other limitations for endovascular treatment are primarily an inability to cross the offending lesion. The presence of severe calcification in the arterial wall as is often seen in end-stage renal disease or diabetes may make treatment difficult or impossible (Fig. 38.2). Typically, the calcium in the wall of the artery forms a point of inflammatory adhesion between the intima, the media, and the adventitia since the calcium deposits in the wall are often transmural. Trying to separate the layers of the artery to allow successful endovascular treatment may be impossible. While there are no standards for their degree of calcification in the arterial wall, severe calcification is clearly a limitation to virtually every endovascular modality.
All interventions done through the arterial lumen as is the case with endovascular treatment require intra-arterial access. These accesses are not trivial and multiple accesses may be required for a single procedure (Table 38.1). Arterial access is the single most common source of complications in endovascular interventions.
Table 38.1 Types of Arterial Access Used for Arterial Interventions | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Contralateral retrograde femoral percutaneous access is the most common approach. In this technique a needle is passed into the femoral artery and using the Seldinger technique and access sheath is placed over a guidewire into the arterial lumen. Typically, these accesses range from 5- to 8-Fr in diameter. This retrograde femoral access can be used to treat the aorta, iliac arteries, or contralateral lower extremity arteries by placing a longer sheath up and over the aortic bifurcation.
The next most common access is the brachial retrograde. In this technique a puncture is placed into the brachial artery and an access sheath is passed into the artery using the Seldinger technique. The difficulty in the brachial access centers on the size of the blood vessel being accessed: The brachial artery often has a high bifurcation into the radial and ulnar arteries and this can impede sheath placement and lead to damage to the access artery. Additionally, working from the arm requires longer wires, catheters, and balloons to treat the SFA. This can increase the difficulty of the procedure significantly since working length of the devices used is critical to their successful deployment. Currently, radial artery access is used for many coronary interventions and as a result many more peripheral interventions are being done using this access. For the SFA this means much longer working lengths for the devices used, increasing technical difficulty.
In Europe, antegrade femoral access is commonly used for many distal lower extremity interventions. The advantage of using this access primarily centers on when the aortic bifurcation has been altered by previous endovascular or surgical treatment. Most commonly this relates to an aortic bifurcation graft or stent graft which has altered the anatomy making contralateral femoral access much more difficult. When this occurs, an alternative to retrograde contralateral femoral access is antegrade ipsilateral femoral access. The difficulty in this access is in trying to get into the vessel above the profunda femoris artery takeoff with enough working length to maintain the access. Typically this should be performed with a bright tip sheath so that the location of the sheath can be constantly imaged. Care also has to be taken when the sheaths are removed since pressure needs to be applied below the skin puncture site whereas a retrograde access will require pressure above the skin puncture site.
The final common access used for lower extremity arterial intervention is retrograde tibial vessel access. Typically this is performed in the dorsalis pedis or posterior tibial arteries (Fig. 38.3) although the peroneal artery can be accessed in some circumstances. This is almost always combined with femoral access, either contralateral or antegrade ipsilateral.
Plain Old Balloon Angioplasty
In the original intervention undertaken by Dotter in 1964, a wire was introduced across the lesion and sequential dilation was performed using larger and larger catheters. The
difficulty with this technique is that the puncture site needs to be of the same size as the final lumen achieved. This rapidly limits the treatment of larger arteries such as the SFA. While this was recognized as a fundamental limitation of the Dotter technique efforts immediately began to develop a balloon technology to try and overcome the limitations of sequential dilatation.
difficulty with this technique is that the puncture site needs to be of the same size as the final lumen achieved. This rapidly limits the treatment of larger arteries such as the SFA. While this was recognized as a fundamental limitation of the Dotter technique efforts immediately began to develop a balloon technology to try and overcome the limitations of sequential dilatation.
In an effort to give much more luminal gain compared to the access diameter, the logical solution was to develop an inflatable balloon which could provide sufficient force to stretch the diseased artery. What was necessary was the development of an inelastic balloon that would not stretch beyond a fixed diameter. While early attempts used latex balloons, it rapidly became apparent that noncompliant polyethylene terephthalate (PET) or nylon balloons provided a much better alternative. Performance characteristics of these balloons are such that they inflate to a predetermined fixed diameter and with increasing pressure do not enlarge further. This allows the force to be controlled within the diseased artery and prevents overexpansion.
Indications
Generally, balloon treatment starts by crossing the lesion in the diseased artery. In many cases lower extremity atherosclerotic disease, particularly superficial femoral artery disease, represents a complete occlusion rather than stenosis. With collateral circulation being provided by the profunda femoris artery, the SFA can functionally occlude and have no consequences at rest. It is only with exertion that SFA disease becomes apparent in the form of claudication, or calf pain with exertion. For this reason many lesions in the superficial femoral artery cannot be crossed in the true lumen, which has become occluded. In this situation traversal of the lesion is often subintimal leading to a dissection channel which is subsequently dilated outside the normal lumen of the artery. The technique of subintimal angioplasty (SIA) will be discussed more completely later in this chapter.
Technique
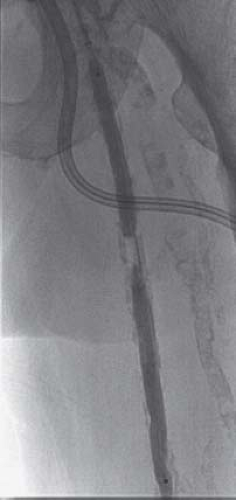
Once the lesion has been crossed with a wire then the balloon must be delivered across the lesion as well. Typically, modern balloons are tightly wrapped and the key is therefore in delivering the balloon to the distal extent of the lesion prior to initial deployment. Once the balloon has been inflated it generally has a somewhat larger profile and is more difficult to advance across tight lesions. Therefore treatment generally will begin distally with sequential overlapping inflations until the proximal lumen is reached. In the past, short balloons were the norm; today 200- or even 300-mm balloons are not uncommon (Fig. 38.4). These longer balloons and improved catheter designs allow crossing of lesions that even a few years ago were not possible to treat.
The successful endovascular treatment of an arterial stenosis or occlusion requires that the layers of the arterial wall be disrupted in some fashion. Typically, this results in a limited arterial dissection (Fig. 38.1) that in most cases will heal with a larger lumen than existed previously. This enlarged lumen relies on controlled healing without scar formation. The underlying facets of this injury and healing lead to the complications associated with plain old balloon angioplasty (POBA). First is the dissection itself. With the separation of the arterial wall layers, the control over the dissection is relatively limited and can lead to a more extensive arterial lesion than necessary. If this injury is sufficient, then thrombosis may develop in the early phases after initial treatment. For this reason, most patients would be kept on antiplatelet agents for a period of time after endovascular treatment. Second, the injury itself may result in a scarring process that leads to the development of an intraluminal lesion referred to as intimal hyperplasia. While no one understands this process fully, this scarring process clearly plays a role
in the recurrent atherosclerotic lesion and in the failure of endovascular treatment. A more in-depth knowledge of this process and its modification is critical to long-term success with endovascular treatment.
in the recurrent atherosclerotic lesion and in the failure of endovascular treatment. A more in-depth knowledge of this process and its modification is critical to long-term success with endovascular treatment.
Other Balloon Techniques
Subintimal Angioplasty
SIA is a technique of revascularization of an artery, where an alternate channel for blood flow is created via the subintimal space beneath the plaque, generally in complete occlusions. It was originally described by Bolia for the femoral-popliteal segment in 1989 but now has gained popularity in various other segments including the iliac and infrapopliteal arteries. Though originally used in high-risk patients for revascularization when surgical bypass was not an option, this technique is fast becoming a widespread treatment for superficial femoral artery occlusions due to its lower risk profile and adequate patency with comparable limb salvage rates.