Fig. 43.1
Image of a lung abscess in the segment 6 left lower lobe
The first significant step in the study of lung abscess was the cardinal observation of D.T. Smith that the bacteria found in the walls of the abscess at autopsy resembled the bacteria noted in the gingival crevice. He postulated that aspiration of oral bacteria was the mechanism of the infection of lung abscess. The next cornerstone in the understanding of lung abscess came from the demonstration of bacterial synergy, as no single microbe reproduced this disease. Smith was able to produce typical lung abscess with an inoculum containing four microbes (an anaerobic spirochete, Fusobacterium nucleatum, Peptostreptococcus spp., and a Gram-negative anaerobe, possibly Prevotella melaninogenica), multiple cavities, and failure of clinical improvement after 7 days of antibiotics.
Other reports of lung abscess isolates included Klebsiella pneumoniae, Legionella micdadei, and Legionella pneumophila types. Others have reported co-isolation of two or more potential pathogens. Nocardia asteroides and Cryptococcus neoformans were isolated from a lung abscess in a patient receiving high-dose corticosteroids.
Management of Lung Abscess
Most patients with primary lung abscess improve with antibiotics, with cure rates documented at 90–95%. Host factors associated with a poor prognosis include advanced age, debilitation, malnutrition, human immunodeficiency virus infection or other forms of immunosuppression, malignancy, and duration of symptoms greater than 8 weeks. The mortality rate for patients with underlying immunocompromised status or bronchial obstruction who develop lung abscess may be as high as 75%.
Medical therapy including antimicrobials remains the cornerstone of therapy. Co-isolation of two or more pathogens from the same specimen may require antimicrobial therapy directed at both potential pathogens. Although the duration of therapy is not well established, most clinicians generally prescribe antibiotic therapy for 4–6 weeks. Expert opinion suggests that antibiotic treatment should be continued until the chest radiograph has shown either the resolution of lung abscess or the presence of a small stable lesion. The rationale for extended treatment maintains that risk of relapse exists with a shorter antibiotic regimen.
In the absence of clinical response, antimicrobial therapy may be combined with tube thoracotomy drainage. Surgical management is considered in cases of large lung abscesses, especially when associated with hemoptysis. Surgery is very rarely required for patients with uncomplicated lung abscesses. The usual indications for surgery are failure to respond to medical management, cases of large lung abscesses, especially when associated with hemoptysis, suspected neoplasm, or congenital lung malformation. The surgical procedure performed is either lobectomy or pneumonectomy.
When conventional therapy fails, either percutaneous catheter drainage or surgical resection is usually considered. Surgical options as video-assisted thoracoscopic surgery (VATS) or open surgery are currently usually reserved for patients with refractory to the antibiotic therapy or acute complications as severe hemoptysis or uncontrolled necrotic pneumonia. However, these approaches, lung resection as the definitive procedure cannot be frequently performed because of septic complications.
These surgical procedures achieved cure rates of 90% but with concomitant mortality rates of 11–28%. In the past two decades, percutaneous catheter drainage has proven effective in appropriately selected adult and pediatric patients. Endoscopic lung abscess drainage is considered if an airway connection to the cavity can be demonstrated. Success of this treatment represents an additional option other than percutaneous catheter drainage or surgical resection. Antibiotic therapy in combination with diagnostic bronchoscopy and postural drainage where indicated is curative in most cases. If this regimen fails, drainage or resection options are usually considered. Pneumonostomy or cavernostomy with direct drainage (Monaldi procedure) (Fig. 43.2) can achieve this goal but is only possible when the pleural space is obliterated. Lung resection as the definitive procedure cannot be frequently performed because of septic complications. These surgical procedures achieved cure rates of 90% but with concomitant mortality rates of 11–28%.
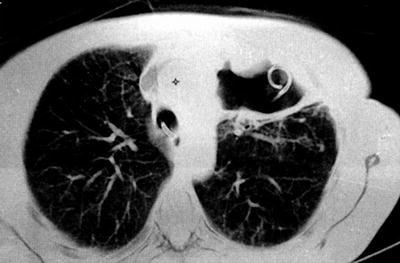
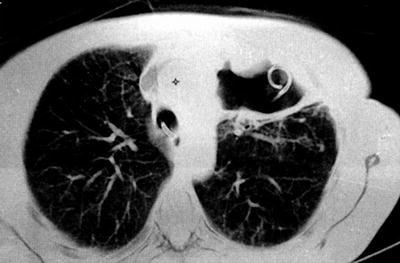
Fig. 43.2
Monaldi procedure
Bronchoscopy is usually performed for sampling purposes as well as to exclude obstructive lesions within the airways. If airway abnormalities associated with the abscess are present, bronchoscopy can also be undertaken therapeutically for relief of the stenosis. Endoscopic abscess drainage is commonly performed in other organs, such as the pancreas, but rarely in the lungs. It has been estimated that drainage is required in 11–21% of patients with lung abscesses in whom medical therapy is unsuccessful. Commonly in these cases, the first consideration is for percutaneous drainage under CT guidance. This approach may be problematic in patients with coagulopathies, if a significant amount of lung tissue needs to be traversed and if other anatomic structures do not allow for unimpeded access to the cavity. Additionally, there is always a concern for soiling the pleural space with abscess contents. Another consideration if percutaneous drainage appears problematic is for surgical resection of the diseased lung and the abscess.
Endoscopic drainage may be a valuable minimally invasive addition to the armamentarium of the chest physician dealing with patients with a lung abscess. It can be considered in selected patients who have an airway connection to the abscess or in whom an endobronchial obstruction preventing drainage is present. It does not carry the risk of soiling the pleural space and is less invasive and not associated with the loss of lung parenchyma as in a surgical resection.
Endoscopic drainage of parenchymal abscess cavities was first reported by Metras and Chapin in 1954. Three more reports have been published between 1975 and 1988. Altogether, 16 cases with five failures of the endoscopic intervention have been described prior to the largest report, including 42 patients.
Endoscopic Lung Drainage
Flexible bronchoscopy through a nasal approach is performed in a standard fashion. After inspection of the airways, the suspected segment is intubated. Under fluoroscopic control, a guide wire has to be introduced into the cavity through the working channel of a flexible bronchoscope. In case of the successful entering of the cavity, the guide wire will be wind up, which can be observed with the help of the fluoroscopy. In some patients, selective bronchography has to be performed first to identify the airway leading into the cavity. Therefore, a BAL catheter is moved forward in the suspected area, and a water-soluble contrast agent is injected to identify the right segment, which lead to the abscess.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


