14
Endocarditis
Transthoracic Echocardiography
Diagnostic Accuracy of Echocardiography for the Detection of Vegetations
Functional Valvular Abnormalities Due to Endocarditis
Other Echocardiographic Findings
LIMITATIONS AND TECHNICAL CONSIDERATIONS
Active versus Healed Vegetations
Nonbacterial Thrombotic Endocarditis
Diagnosis of Vegetations with Underlying Valve Disease
Basic Principles
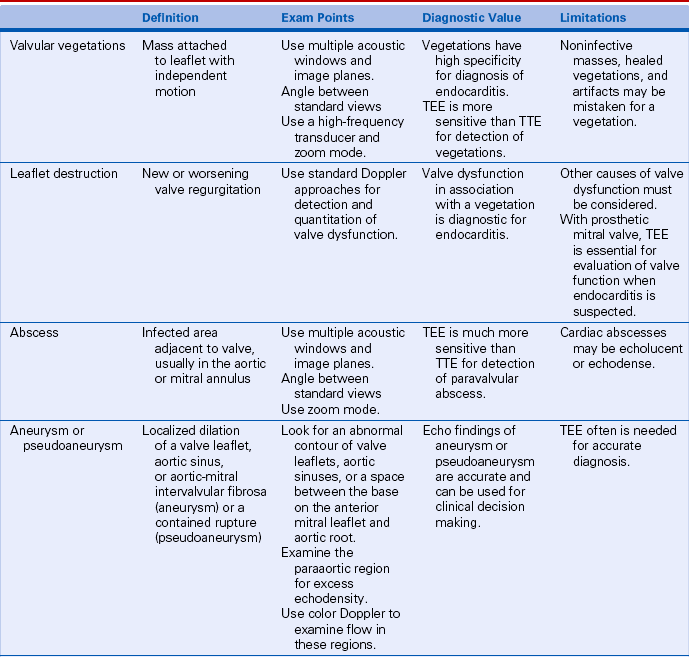
The diagnosis of endocarditis is most secure when there is pathologic confirmation of a valvular vegetation with active infection, local tissue destruction, and/or paravalvular abscess formation. In the clinical setting, endocarditis is diagnosed based on a combination of echocardiographic, laboratory, and physical examination findings as detailed in Table 14-1. The major criteria for the diagnosis of endocarditis are persistent bacteremia with typical organisms and echocardiographic evidence of endocardial involvement. Minor criteria include less specific bacteriologic and echocardiographic findings, factors predisposing to endocarditis (such as preexisting valve disease or intravenous drug use), vascular events (such as pulmonary or systemic emboli), immunologic phenomena (such as glomerulonephritis), and signs of systemic infection (such as fever).
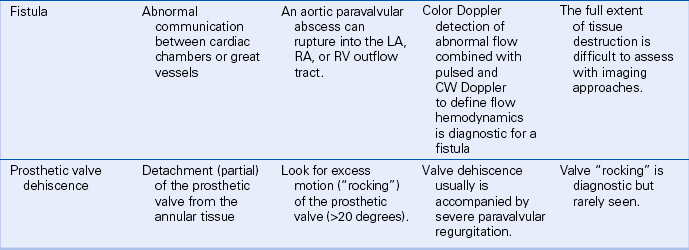
TABLE 14-1
Modified Duke Criteria for Infective Endocarditis
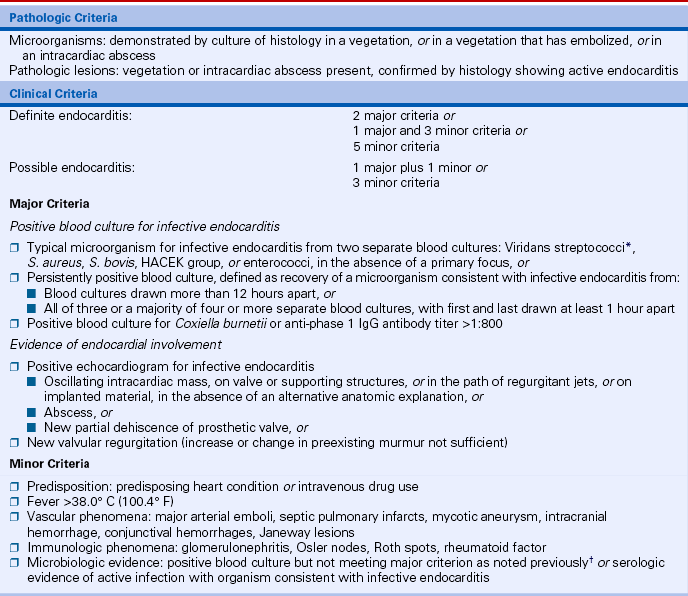
∗Including nutritional variant strains.
†Excluding single positive cultures for coagulase-negative staphylococci and organisms that do not cause endocarditis.
From Durack DT, Lukes AS, Bright DK: New criteria for diagnosis of infective endocarditis: Utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med 96:200-209, 1994. With a modification by Li JS, Sexton DJ, Mick N, et al: Proposed modification to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 30:633-638, 2000.
 Presence, location, size, and number of valvular vegetations
Presence, location, size, and number of valvular vegetations
 Functional abnormalities of the affected valve(s), especially valvular regurgitation
Functional abnormalities of the affected valve(s), especially valvular regurgitation
 Underlying anatomy of the affected valve(s) and any coincident valvular disease
Underlying anatomy of the affected valve(s) and any coincident valvular disease
 Impact of valvular dysfunction on left ventricle (LV) size and systolic function
Impact of valvular dysfunction on left ventricle (LV) size and systolic function
 Other complications of endocarditis (e.g., paravalvular abscess, pericardial effusion)
Other complications of endocarditis (e.g., paravalvular abscess, pericardial effusion)
In addition, echocardiographic findings provide prognostic data on the anticipated clinical course, risk of systemic embolization, and potential need for surgical intervention.
 The identification of any valvular vegetations
The identification of any valvular vegetations
 The assessment of valve anatomy and function with respect to anatomic or physiologic factors that increase the likelihood of endocarditis (e.g., bicuspid aortic valve, myxomatous mitral valve)
The assessment of valve anatomy and function with respect to anatomic or physiologic factors that increase the likelihood of endocarditis (e.g., bicuspid aortic valve, myxomatous mitral valve)
Echocardiographic Approach
Transthoracic Echocardiography
On echocardiographic imaging, the features that typify a valvular vegetation (Table 14-2) are:
For example, an aortic valve vegetation prolapses into the LV outflow tract in diastole and extends into the aortic root in systole (Fig. 14-1). The mass is attached to the LV side of the valve leaflet but shows motion in excess of normal valve excursion with rapid oscillations in diastole (best appreciated on M-mode recordings). A mitral valve vegetation is attached on the atrial side of the valve, prolapses into the left atrium (LA) in systole, and moves into the LV, beyond the normal range of mitral valve opening, in diastole (Fig. 14-2).
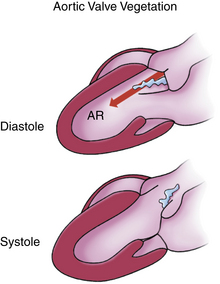
Figure 14–1 Schematic diagram of an aortic valve vegetation.
An irregularly shaped mobile mass is attached to the ventricular side of the leaflet with prolapse into the LV outflow tract in diastole. AR, aortic regurgitation.
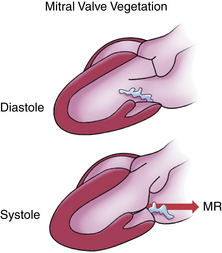
Figure 14–2 Schematic diagram of a mitral valve vegetation.
An irregularly shaped mobile mass is attached to the atrial side of the leaflet with prolapse into the LA in systole. MR, mitral regurgitation.
Multiple acoustic windows and two-dimensional (2D) or three-dimensional (3D) views are needed for the detection of a valvular vegetation. Because the vegetation is a discrete structure, it may be seen only in certain tomographic planes. With 2D imaging, slow scanning between the standard image planes—for example, between the parasternal long-axis view and the right ventricular (RV) inflow view—increases the likelihood of identifying a valvular vegetation. Orthogonal views further ensure that all segments of the valve leaflets are examined. In a patient with suspected endocarditis, a complete examination is needed with scanning from parasternal, apical, subcostal, and suprasternal notch views for careful evaluation of each valve. The reported sensitivity of TTE for the detection of valvular vegetations ranges from less than 50% to as high as 90% (Table 14-3). To some extent, the reported sensitivity of TTE increased as echocardiographic image quality has improved. It is possible that 3D imaging will provide further improvements in the accuracy of TTE echocardiography for the detection of vegetations, but this has not yet been demonstrated.
TABLE 14-3
Accuracy of Echocardiographic Diagnosis of Valvular Vegetations (Selected Studies)
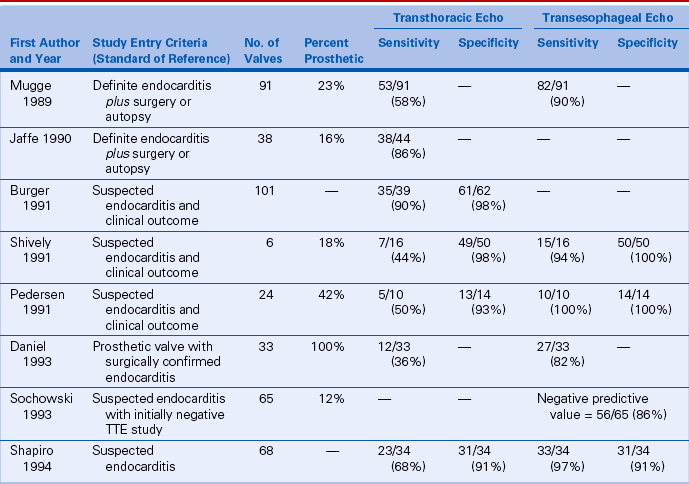
Data from Mugge et al: J Am Coll Cardiol 14:631-638, 1989; Jaffe et al: J Am Coll Cardiol 15:1227-1233, 1990; Burger et al: Angiology 42:552-560, 1991; Shiveley et al: J Am Coll Cardiol 18:391-397, 1991; Pedersen et al: Chest 100:351-356, 1991; Daniel et al: Am J Cardiol 71:210-215, 1993; Sochowski, et al: J Am Coll Cardiol 21:216-221, 1993; Shapiro et al: Chest 105:377, 1994.
Aortic Valve
Aortic valve vegetations most often are detected in parasternal long- and short-axis views. Careful angulation from medial to lateral in the long-axis plane and from inferior to superior in the short-axis plane is needed, because vegetations often are eccentrically located. Image quality is optimized by use of a minimum depth setting and adjustment of gain and processing parameters. An echogenic mass attached to the ventricular side of the leaflet with independent motion and prolapse into the outflow tract in diastole is diagnostic for a valvular vegetation (Fig. 14-3). Rapid oscillating motion may be best appreciated on an M-mode recording.
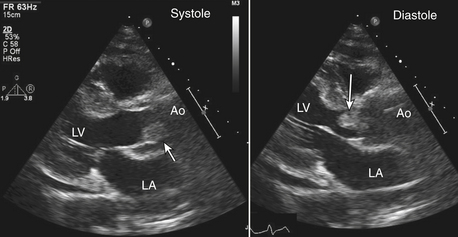
Figure 14–3 ![]() Aortic valve vegetation.
Aortic valve vegetation.
In a TTE parasternal long-axis view, a large echodensity (arrow) is seen in the aorta attached to the posterior aortic valve leaflet in systole with prolapse into the LV outflow tract in diastole. In addition to moving with the leaflet, the mass showed rapid oscillating motion typical of a vegetation.
Less typically, a vegetation may be attached to the aortic side of the leaflet or may show little independent motion. A definitive diagnosis may be difficult if the underlying valve anatomy is abnormal. For example, a vegetation on a calcified aortic valve may be difficult to diagnose because of shadowing and reverberations by the leaflet calcification. In these cases, the findings of independent motion and prolapse into the LV in diastole are particularly helpful signs. Comparison with previous echocardiograms may allow recognition of recent changes, increasing the likelihood of valve infection, or may show no significant difference, decreasing the likelihood of an acute process.
Findings that may be mistaken for an aortic valve vegetation include beam-width artifact related to a calcified nodule, a prosthetic valve, the normal leaflet apposition zone, or the normal leaflet thickening at the central coaptation region (the nodule of Arantius). Occasionally, a linear echo representing a normal variant called a Lambl excrescence is seen. These small fibroelastic protrusions from the ventricular side of the leaflet closure zone occur with increasing frequency with age and are present in a high percentage of patients (Fig. 14-4).
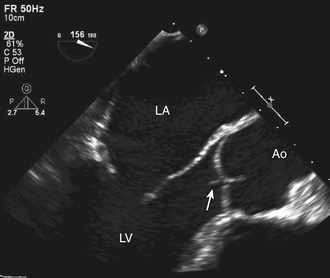
Figure 14–4 ![]() Lambl excrescence.
Lambl excrescence.
TEE long-axis view showing a thin, linear echodensity at the aortic closure line that might be mistaken for a valvular vegetation.
Mitral Valve
Mitral valve vegetations typically are located on the atrial side of the leaflets. Diagnostic features include rapid independent motion, prolapse into the LA in systole, and functional evidence of valve dysfunction. Parasternal long- and short-axis views with careful scanning across the valve apparatus in both image planes allows assessment of the presence, size, and location of any vegetation (Fig. 14-5). Apical four-chamber, two-chamber, and long-axis views again are helpful both in visualizing valve and vegetation anatomy and in distinguishing a true valve mass from an ultrasound artifact.
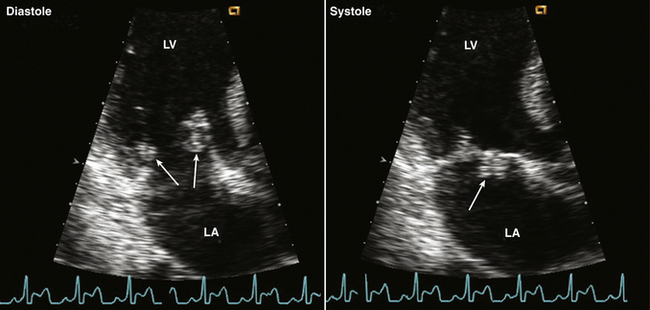
Figure 14–5 ![]() Mitral valve vegetation.
Mitral valve vegetation.
Typical-appearing mitral valve vegetations (arrows) seen in an apical long-axis view in diastole attached to the atrial side of the anterior and posterior mitral valve leaflets (left). In systole (right), the anterior leaflet mass prolapses into the LA with motion in real time independent of valve leaflet motion.
As for the aortic valve, beam-width artifacts can be mistaken for a vegetation. A particular artifact to be aware of is the appearance of a “mass” on the atrial side of the anterior mitral leaflet in the apical four-chamber view due to beam-width artifact from a calcified or prosthetic aortic valve. Other types of mitral valve pathology may be difficult to distinguish from a valvular vegetation, including a severely myxomatous leaflet, a partial flail leaflet, or a ruptured papillary muscle. Comparison with previous studies may help differentiate an acute process from chronic underlying valve disease. Endocarditis also can occur on an anatomically normal valve (Fig. 14-6). With mitral valve endocarditis, mitral regurgitation often, but not invariably, is present.
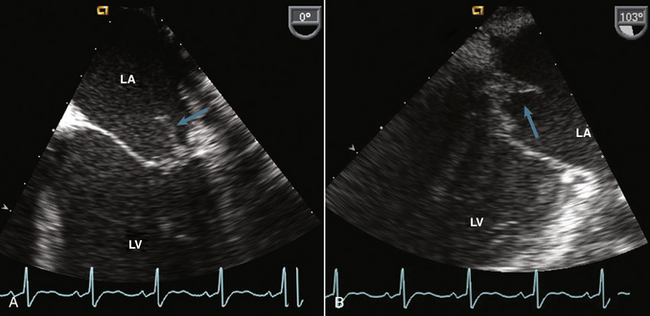
Figure 14–6 ![]() TEE imaging of a mitral valve vegetation.
TEE imaging of a mitral valve vegetation.
In this 22-year-old man with a history of intravenous drug use and bacteremia, the four-chamber view shows a vegetation (arrow) on a normal-appearing mitral valve (A). Rotation of the image plane to 103° (B) shows that the vegetation (cyan arrow) is attached at the base of the leaflet, raising concern for paravalvular abscess.
Tricuspid Valve
Tricuspid valve endocarditis occurs most often in intravenous drug users and is associated with large vegetations due to Staphylococcus aureus infection. The RV inflow view often is diagnostic, showing a large, mobile mass of echoes attached to the atrial side of the leaflet with prolapse into the right atrium (RA) in systole (Fig. 14-7). Given the range of excursion and mobility of these vegetations, it is not surprising that septic pulmonary emboli are a frequent complication of tricuspid valve endocarditis. The apical and subcostal four-chamber views allow further evaluation of the presence and extent of tricuspid valve infection. Assessment of tricuspid regurgitant severity and consequent RA and RV dilation also can be performed from these windows.
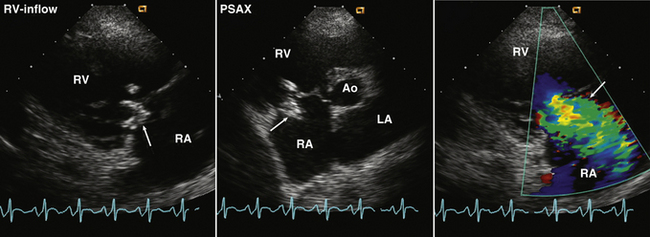
Figure 14–7 ![]() Tricuspid valve vegetation.
Tricuspid valve vegetation.
TTE imaging in an RV inflow view of a patient with a history of intravenous drug use and S. aureus tricuspid valve endocarditis. In an RV inflow view (left), the mass is seen at the leaflet coaptation (arrow). In a parasternal short-axis view (center), a mobile mass (arrow) is seen prolapsing into the RA attached to the tricuspid valve leaflet. Color flow Doppler (right) demonstrates a broad jet of reverse flow across the valve in systole (arrow) consistent with severe tricuspid regurgitation.
Transesophageal Imaging
From the TEE approach, the aortic valve is examined in multiple image planes including standard long-axis (typically at approximately 120° rotation) and short-axis (about 45° rotation) views. As with TTE imaging, careful scanning from medial to lateral in the long-axis view and from superior to inferior in the short-axis view is needed to fully evaluate valve anatomy and to achieve a high sensitivity for the detection of valvular vegetations (Figs. 14-8 and 14-9). When the image plane is oblique, an aortic leaflet may be seen en face, mimicking an aortic valve mass. Evaluation in more than one image plane and assessment of the pattern of motion (rapid oscillating independent motion versus motion with the valve) avoids this potential error. Image quality may be enhanced by the use of a higher-frequency transducer and magnification of the area of interest, but small, normal variants of valve anatomy should not be interpreted as abnormalities. Sometimes the aortic valve can be evaluated from a transgastric apical view; however, image quality may be no better than from a TTE approach because of the distance from the transducer to the aortic valve.
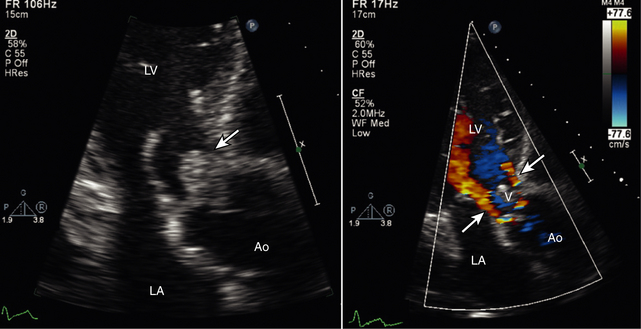
Figure 14–8 ![]() Aortic valve vegetation and regurgitation.
Aortic valve vegetation and regurgitation.
In a TTE apical long-axis view (left), a large aortic valve vegetation is seen that nearly occludes the LV outflow tract in diastole. In the color Doppler image (right), two narrow jets of aortic regurgitation (arrows) are seen around the vegetation.
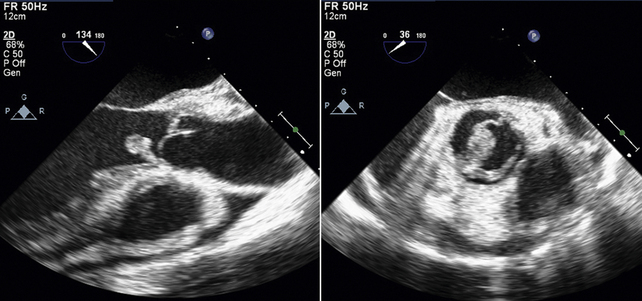
Figure 14–9 ![]() TEE aortic valve vegetation.
TEE aortic valve vegetation.
In the same patient as in Figure 14-8, the TEE long-axis view (left) shows the attachment of the vegetation at the base of the aortic valve. The short-axis view (right) shows that the underlying anatomy is a bicuspid valve with an additional vegetation (short arrow) attached to the more posterior valve leaflets. The increased echodensity posterior to the aortic valve (arrows) in the long-axis views raises concern for paravalvular abscess.
The mitral valve is well seen from a high esophageal position. Because the mitral valve plane is perpendicular to the ultrasound beam from this approach, excellent images can be obtained in multiple views by slowly rotating the multiplane transducer from 0° to 180°. Particular attention should be paid to standard four-chamber (at 0°), two-chamber (at 60°), and long-axis (at 120°) views. The degree of mitral regurgitation can be assessed with color flow imaging in these same views. Given the distance of the mitral valve from the chest wall in both parasternal and apical TTE views, TEE imaging often provides dramatically better images and important clinical data (Figs. 14-10 and 14-11).
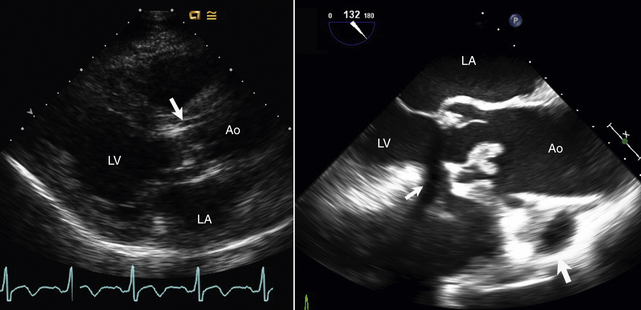
Figure 14–10 ![]() Fungal endocarditis.
Fungal endocarditis.
TTE (left) and TEE (right) imaging in a patient with fungal endocarditis. The unusual-appearing valvular vegetation (arrow) is seen on TTE imaging but is better defined on TEE imaging, with a dense spherical mass with some small attached areas of independent motion (arrows).
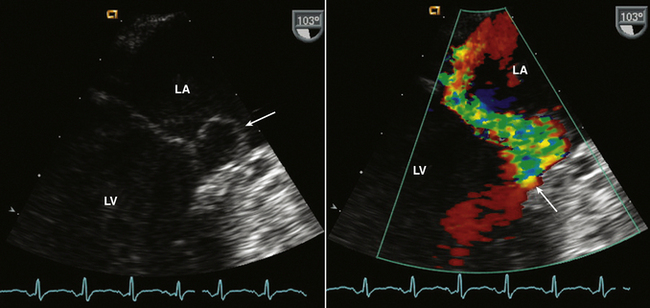
Figure 14–11 Mitral leaflet perforation.
TEE echocardiography in a 28-year-old man with systemic embolic events and blood culture results positive for S. aureus. There is an apparent prolapse of the lateral segment of the mitral leaflet in a two-chamber view (left). However, color flow Doppler (right) shows an eccentric jet of severe mitral regurgitation that goes through the base of the posterior leaflet, suggesting leaflet perforation due to infective endocarditis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree