Fig. 5.1
Pulmonary pedicle (pulmonary arteries)
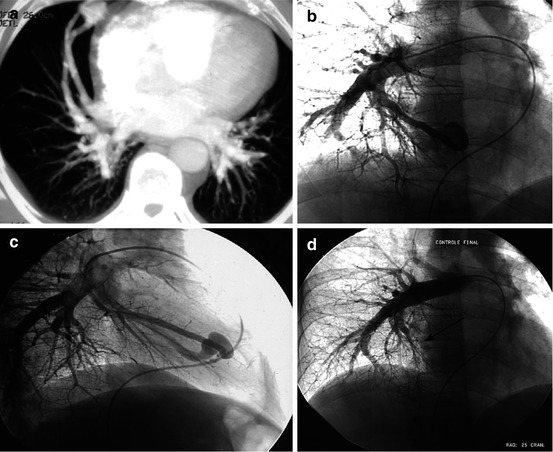
Fig. 5.2
Repeated hemoptysis, consequence of a bleeding single right basal PAVM. (a) Axial MIP thick CT scan: voluminous PAVM, with indentified afferent artery and efferent vein. (b, c) Pulmonary angiography (frontal (1–2) and lateral (1–3) views), well correlated with CT data: voluminous mediobasal feeding artery, large saccular aneurysm, and early venous flow. (d) Control angio after endovascular exclusion using AVP occluder, delivered just upstream the sac
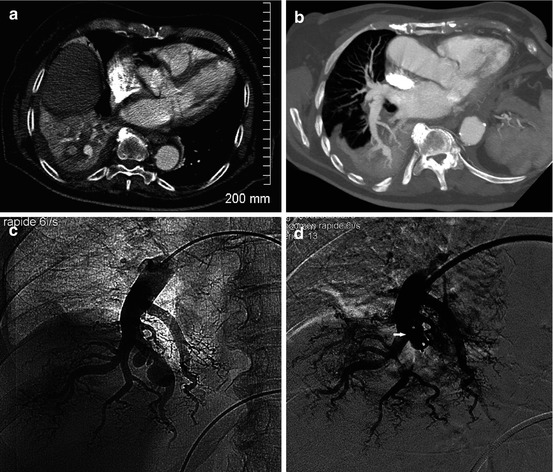
Fig. 5.3
Right basal bronchial cancer: massive hemoptysis. (a, b) CT: bleeding pulmonary, a false aneurysm. (c) Selective right pulmonary angiography: false aneurysm caused by tumoral erosion. (d) Exclusion with AVP (arrow)
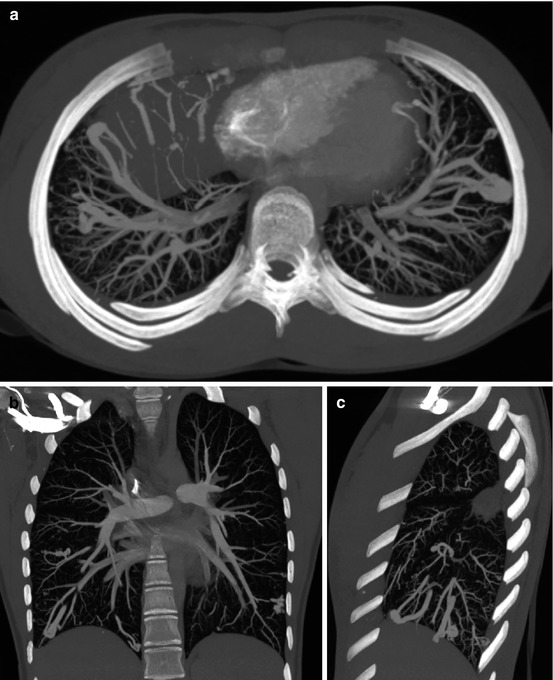
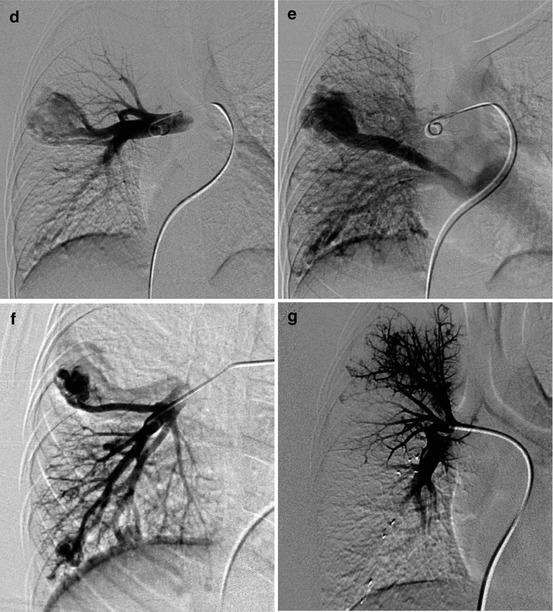
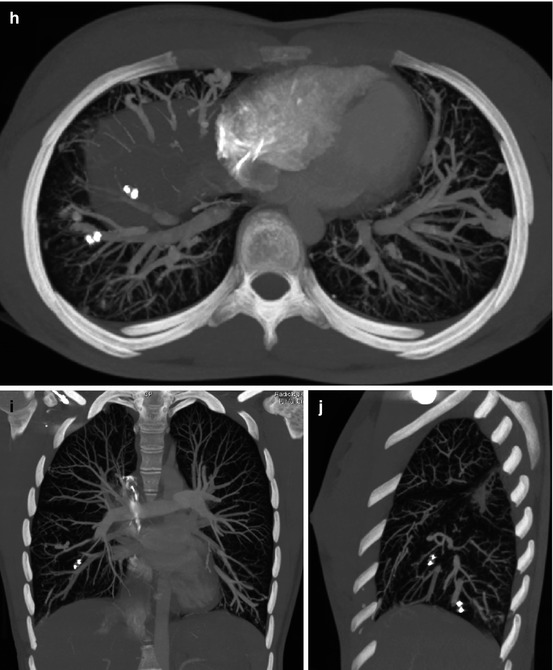
Fig. 5.4




16-year-old, family history of Rendu-Osler-Weber syndrome: hypoxia, severe left–right shunt, and pulmonary hypertension. (a–c) MIP: multiple PAVMs, of which the most voluminous in the right inferior lobe. (d, e) Right selective pulmonary angio: large middle lobe PAVM. Arterial phase (d) and then massive early venous flow (e). (f) Selective right inferior lobar injection: at least 2 other PAVMs. (g) First session: middle lobe PAVM AVP exclusion. Left shunts have been secondarily treated (delay between the 2 procedures: 2 months). (h–j) Angio CT 6 months after the last embolization session
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


