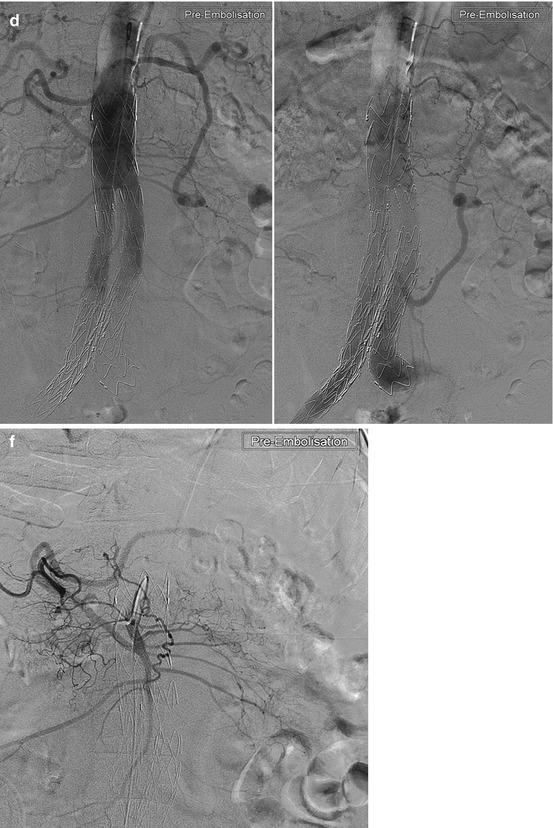
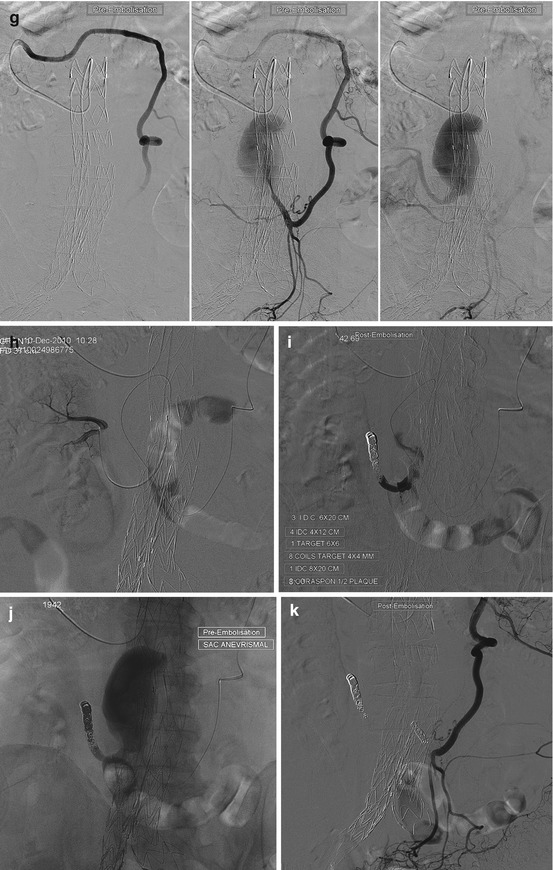
Fig. 17.1
A 69-year-old patient, with end-stage renal failure, under hemodialysis for several years. An infrarenal abdominal aortic aneurysm was treated by stent graft (EVAR) 2 years ago. Due to the oligo-anuric renal failure, it was accepted to cover a right accessory renal artery, originating low in the aorta (L4) follow-up of the aneurysmal sac after EVAR showed an increase in size (10 mm in 6 months). (a) Arterial phase CT: extra-prosthetic intra-saccular enhancement. (b) MIP reconstruction in the sagittal plane, showing a massive enhancement of the sac, from a type 2 endoleak involving the arcade of Riolan. (c) MPR reconstruction. (d) Aortography, early phase (from a right femoral catheterization): the arcade of Riolan is very early injected. (e) Selective catheterization of the middle colic artery (branch of the SMA) (early phase). (f) Selective catheterization, via the arcade of Riolan, of the IMA and of the extra-prosthetic sac and then of the low lumbar right renal artery. (g) Control after occlusion by coils of the low lumbar right renal artery. (h) Exclusion of the sac by glue embolization (Histoacryl). (i) Control after coiling at the origin of the IMA, whose branches stay perfused by the arcade of Riolan
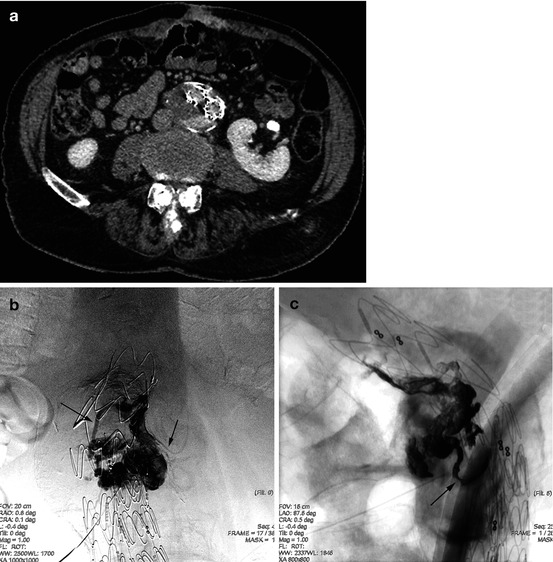
Fig. 17.2
A 67-year-old, with increasing abdominal aortic aneurism diameter 18 months after EVAR (aorto-bi-iliac stent graft). Follow-up CT showed a type II lumbar endoleak, inaccessible to an endovascular treatment. (a) CT showing posterior endoleak fed by a lumbar artery. (b) (AP) and (c) (lateral): Periprosthetic endosaccular access via a CT-guided transparietal puncture: injection of Onyx. Note the opacification of two lumbar arteries (arrows)
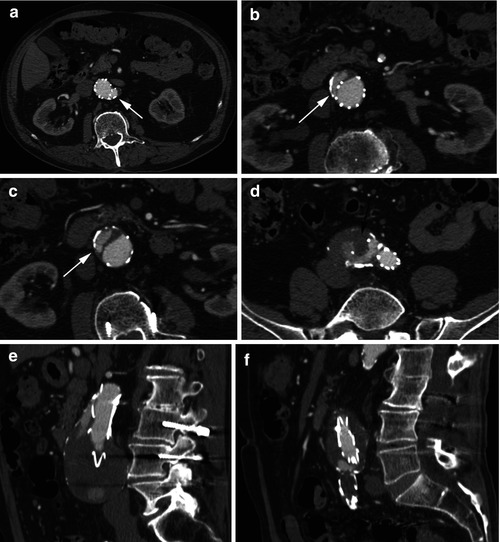
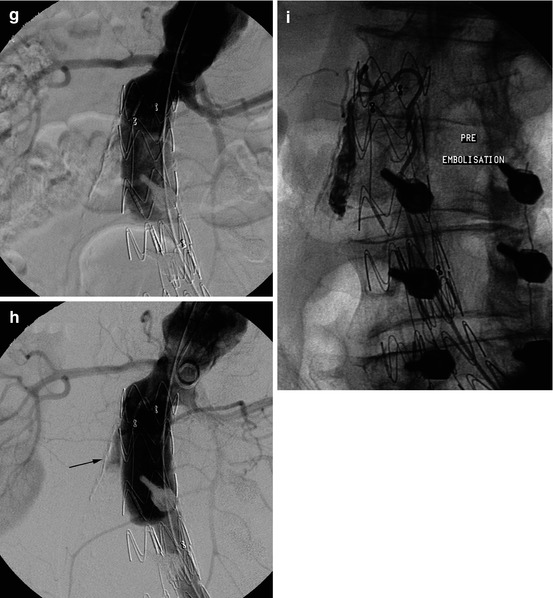
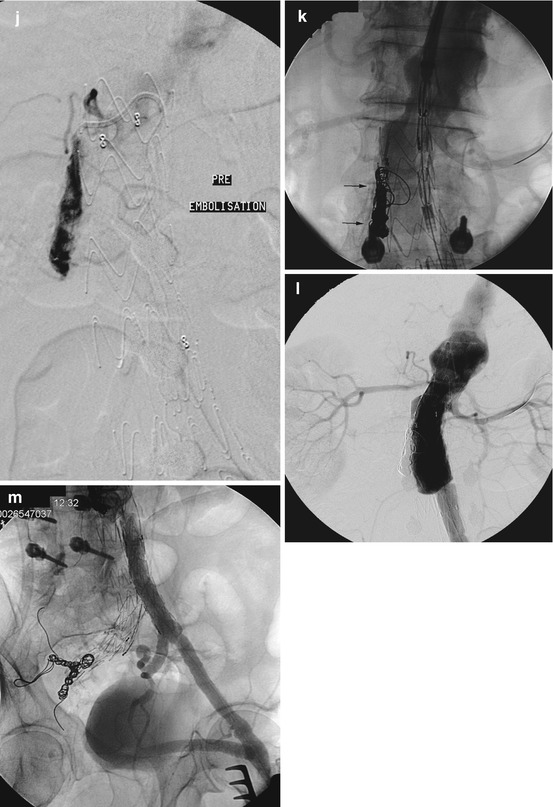

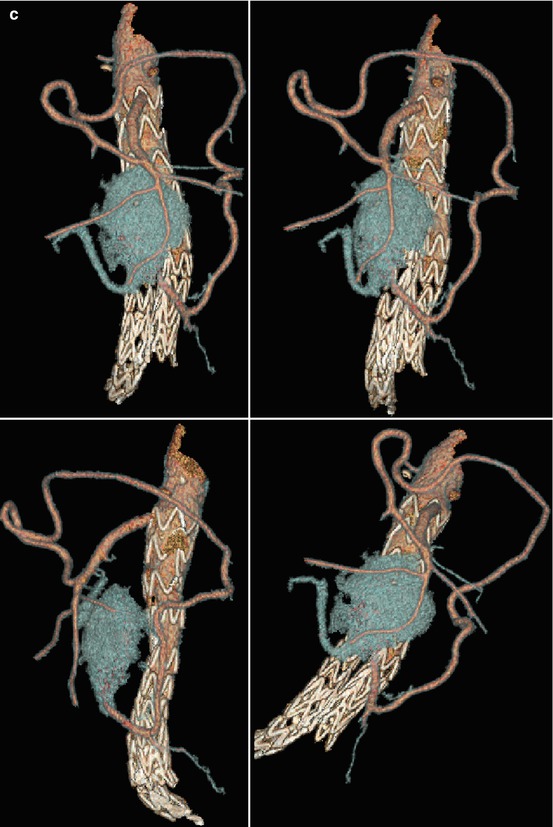
Fig. 17.3
A 83-year-old M, EVAR (aortoiliac stent graft) 3 years ago to treat an infrarenal aortic abdominal aneurysm. An occlusion of the right leg after few weeks had led to a suprapubic left-right cross bypass. Annual CT follow-up has shown an increase in size of the sac. Which was caused by various endoleaks: type 1, due to a continuous growth in diameter of aorta above the stentgraft; type 2, via lumbar arteries, which seemed contingent; and finally suspected type 3 endoleak due to the imperfect coaptation between the aortic piece and the left iliac leg of the stent graft. (a) CT scan at the upper extremity of the stent graft, at the level of the ostium of the left renal artery (arrow). (b–d) Scans below the previous: endosaccular extra-prosthetic anterior enhancement (arrows), occluded right leg of the endoprosthesis (black arrow). (e, f) Sagittal CT reconstruction: type 1 endoleak; reconstruction passing through the right leg (3–6): type 3 endoleak. (g) Aortography conducted via a left humeral access (pigtail), a guidewire was also led via a left femoral access. Late phase (h): right endosaccular extra-prosthetic enhancement (arrow) (note the presence of a bone screw, from a previous spine surgery). (i, j) The type 1 endoleak was confirmed by selective catheterization, using a Mikaelsson catheter inserted between the proximal uncovered petals of the stent graft. (k) Coils (arrows) were positioned in the flowing phase of the endoleak; then a cuff (short cylindrical stent graft) was deployed at the upper neck. On this image, before the release of the cuff, note the ostium of the left renal artery catheterized by a guidewire brought via the humeral access. (l) Control after coiling and expansion of the cuff: exclusion of the type 1endoleak. (m, n) Type 3 endoleak is not clearly shown by the injections at the lower part of the aorta; occlusion of the left prosthetic branch; coils in the right hypogastric artery (that preceded the stent grafting implantation, to avoid reinjection); good patency of the left hypogastric artery, downstream of the stent graft; suprapubic left-right cross bypass. However, a complementary left iliac stent graft was deployed to cover the prosthetic aortoiliac anastomosis. (o, p) Final control opacification
References
1.
Becquemin JP, et al. Outcomes of secondary interventions after abdominal aortic aneurysm endovascular repair. J Vasc Surg. 2004;39(2):298–305.PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


