A. Immediate delivery
B. No need for any intervention
C. Atenolol
D. Digoxin
E. Adenosine IV to the mother
2. A 9-year-old young boy after being evaluated by an ophthalmologist for drooping eyelids is noted to have a first degree atrioventricular (AV) block, a right bundle branch block, and a left anterior vesicular block on a 12-lead electrocardiogram. What would be the most logical next step?
A. Implant a pacemaker
B. Implant an implantable cardioverter defibrillation (ICD)
C. Perform an electrophysiologic study
D. Initiate medical therapy with theophylline
E. IV steroid administration
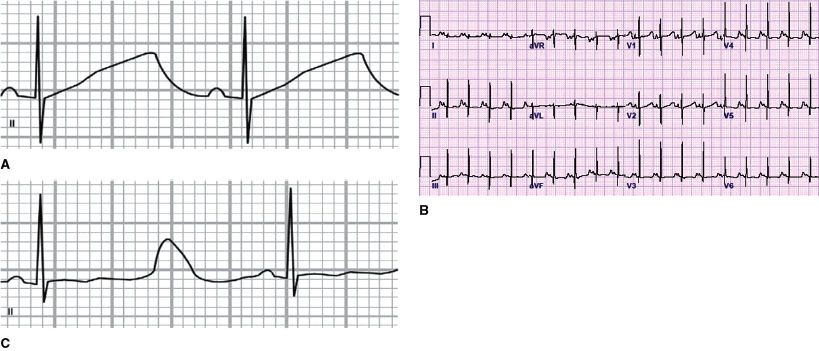
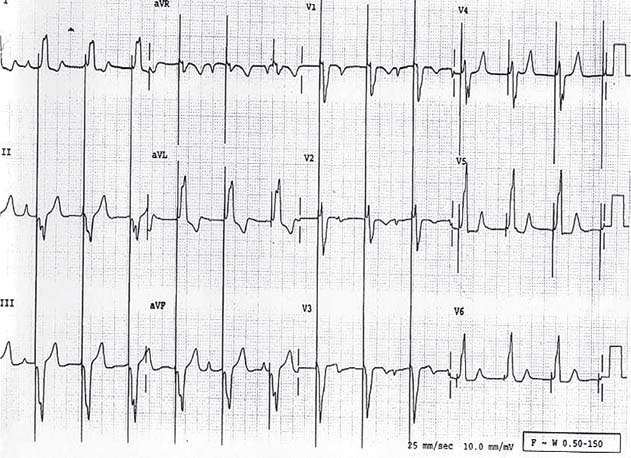
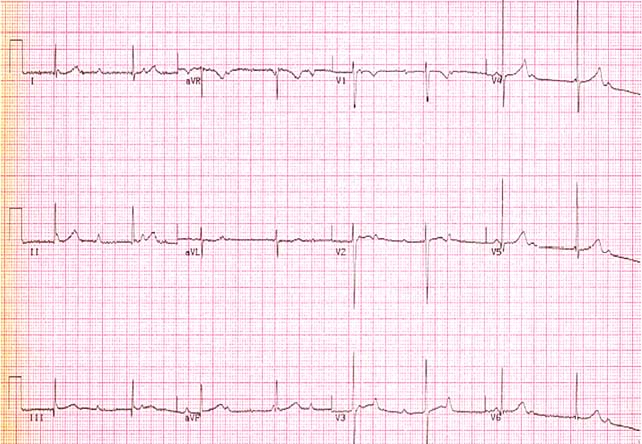
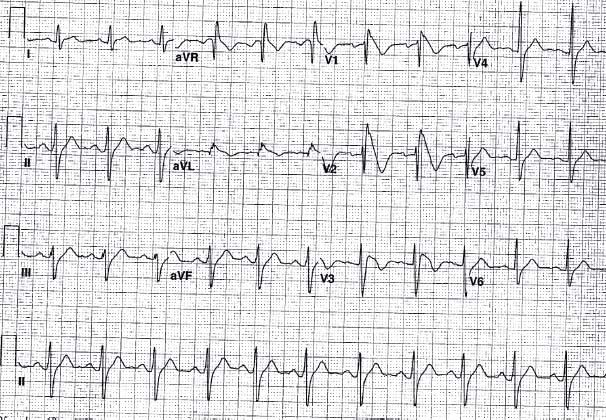
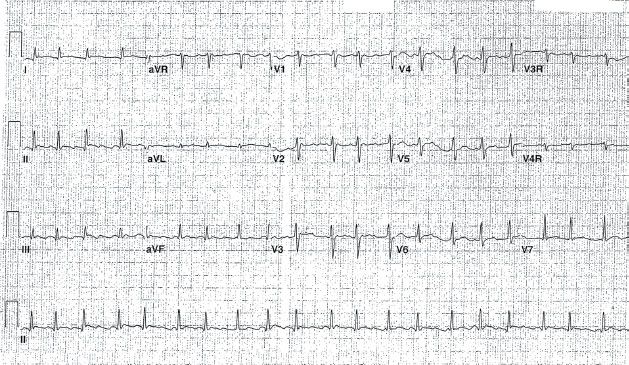
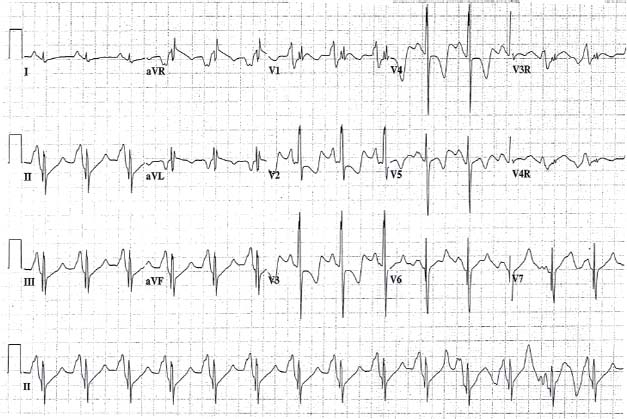
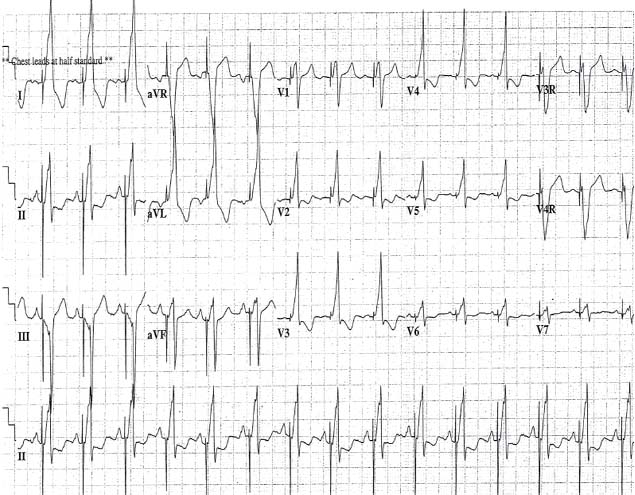
3. A 6-year-old child presents after a sudden cardiac arrest. An electrocardiogram obtained after he has made a full recovery showed the findings in Figure 6.2. What would be the most appropriate therapy?
A. Implant an ICD
B.Begin β-blocker therapy and follow up in 2 weeks
C. Perform an electrophysiology study
D. Start amiodarone
E. Implant a pacemaker
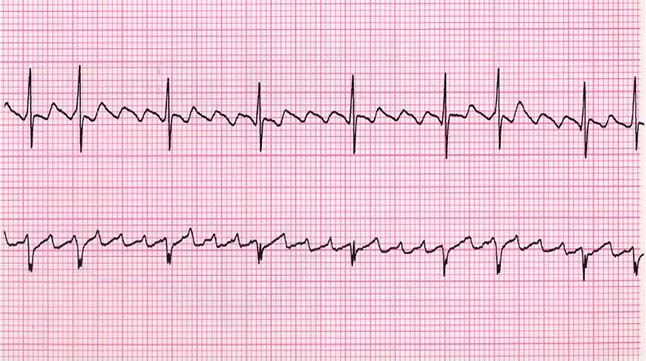
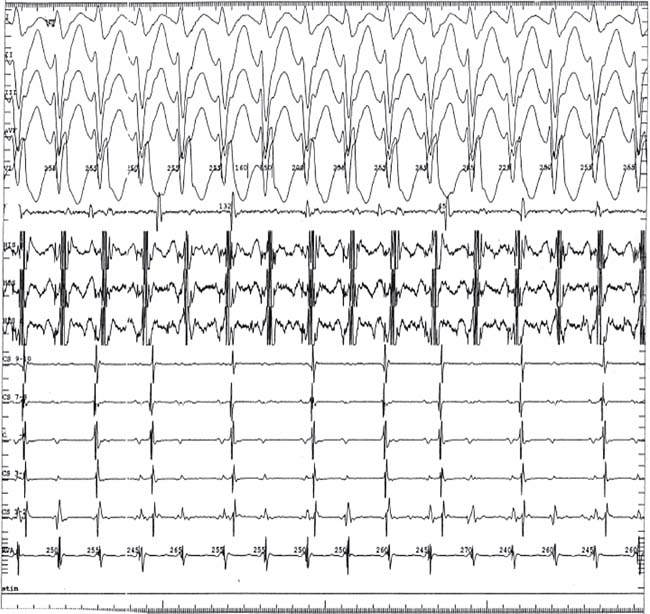
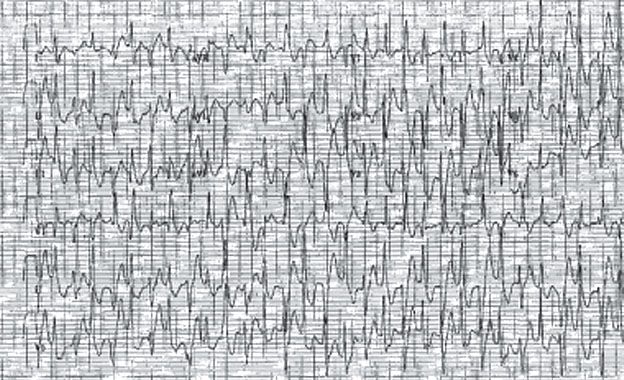
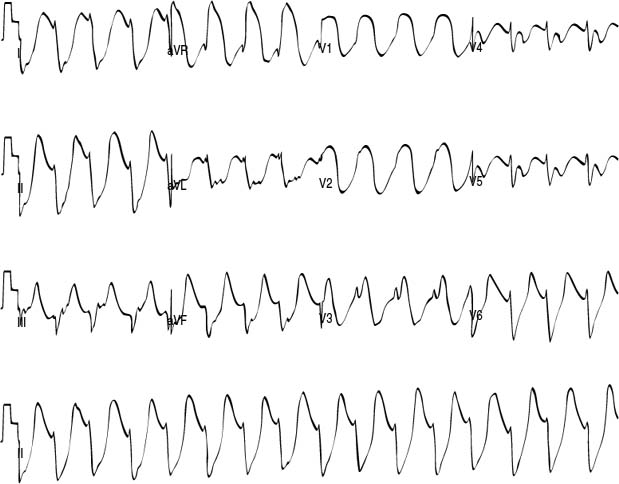
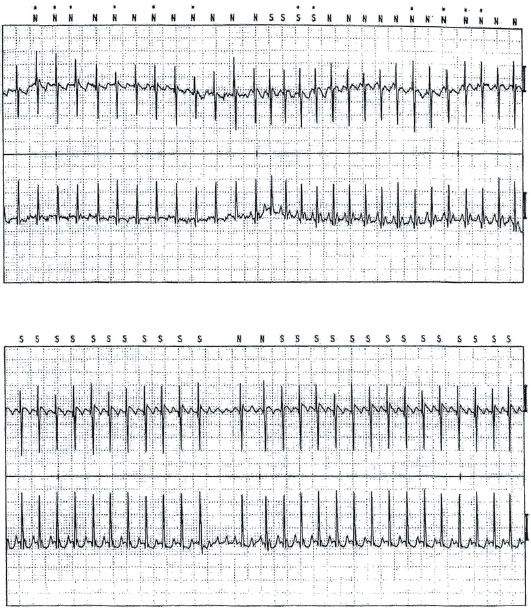
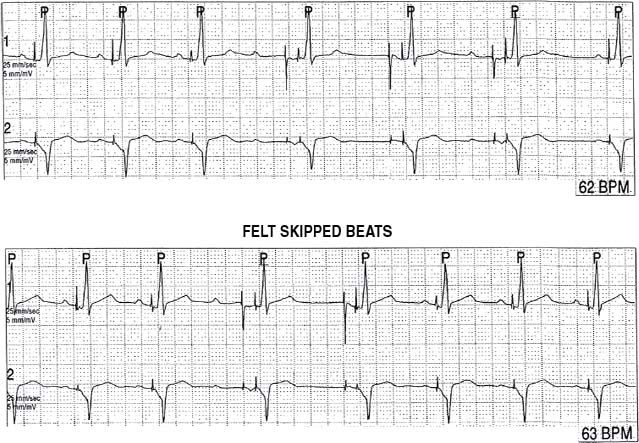
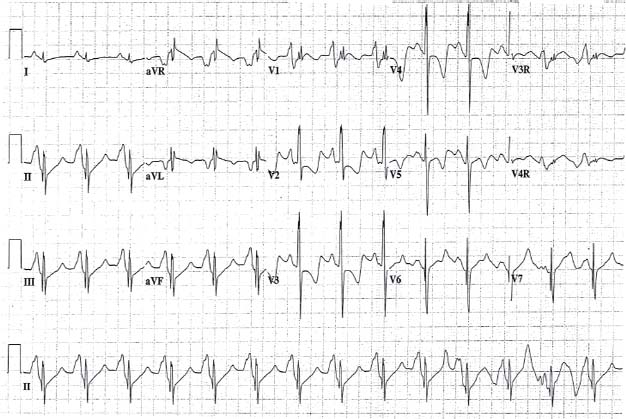
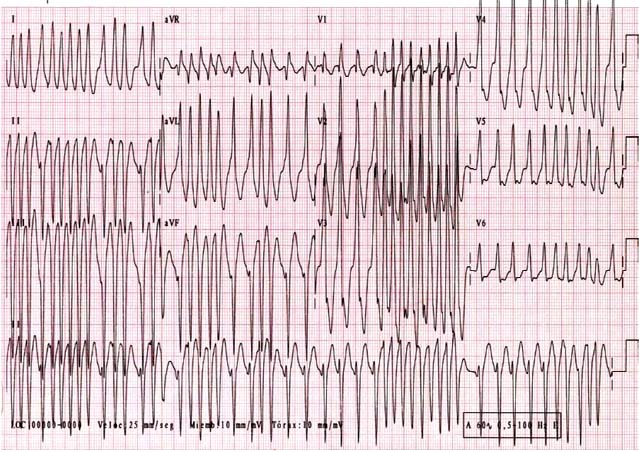
4. A newborn presents with a narrow complex tachycardia. Adenosine is given and a change in the heart rate noted as seen in the rhythm strip in Figure 6.3. What is the most effective method for terminating the tachycardia?

A. Oral amiodarone
B. Oral digoxin
C. Intravenous amiodarone
D. Oral propranolol
E. Direct current cardioversion
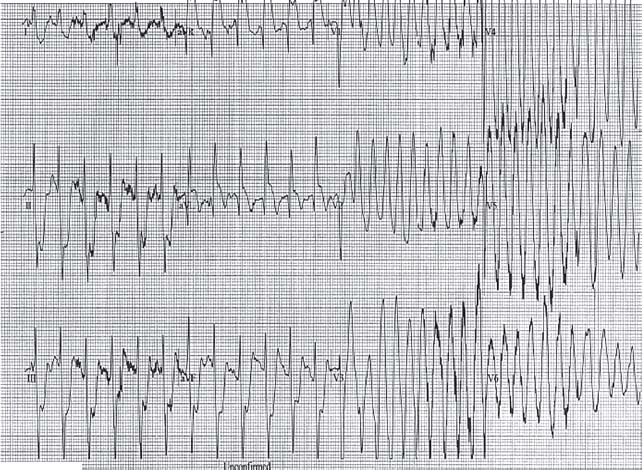
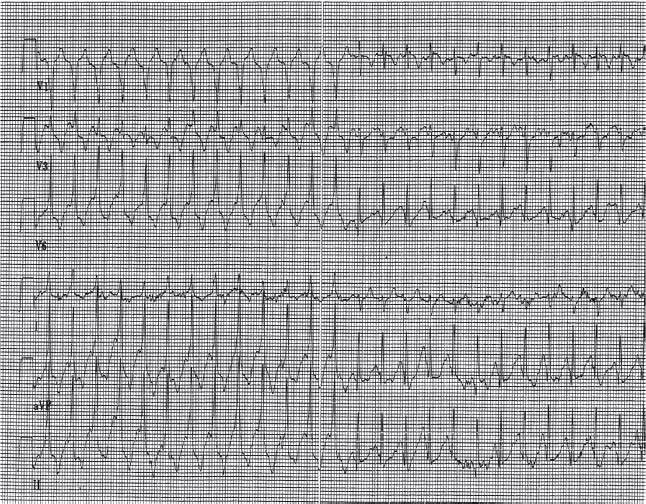
5. A 2-year-old patient with DiGeorge syndrome presents with hypocalcemia, seizure, and the rhythm strip in Figure 6.4. Which of the following choices is the most likely cause of his erratic rhythm?

A. Ventricular fibrillation
B. Ventricular flutter
C. Atrial fibrillation
D. Movement artifact
E. Supraventricular tachycardia
6. A patient who presents for a routine sports physical is noted to have left ventricular (LV) septal hypertrophy on his echocardiogram consistent with hypertrophic cardiomyopathy. Which of the following additional factors most increases the risk of sudden death?
A. Marked LV hypertrophy on the ECG
B. LV septal thickness of 1.7 cm
C. LV outflow gradient of 20 mm Hg.
D. Family history of multiple sudden deaths
E. Chest pain with exercise
7. A 12-year-old patient with dilated cardiomyopathy is on digoxin, furosemide, and enalapril for his heart failure. He is now starting to have frequent episodes of supraventricular tachycardia (SVT) and you would like to start him on amiodarone. What medications do you have to adjust?
A. Decrease the dose of Digoxin
B. Increase the dose of Digoxin
C. Increase the dose of furosemide
D. Decrease the dose of enalapril
E. Make no changes in any of the medications
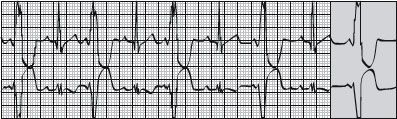
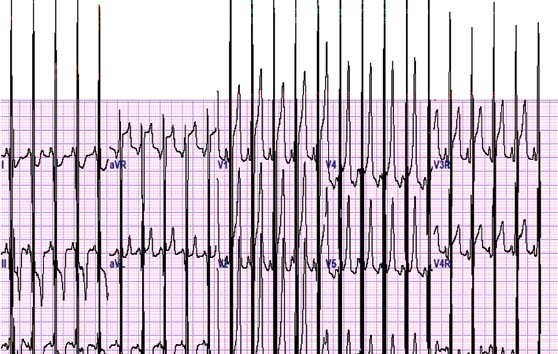
8. A 6-year-old boy has been complaining of episodes of fast heart rates lasting 15 to 20 min. These typically occur at rest. He has one such episode every 3 months. A 24-hour Holter monitor shows variability in the QRS morphology as shown in Figure 6.5. The etiology of his symptoms is most likely to be which of the following?
A. Ventricular tachycardia
B. Junctional tachycardia
C. Reentrant supraventricular tachycardia
D. Atrial flutter
E. Automatic focus atrial tachycardia
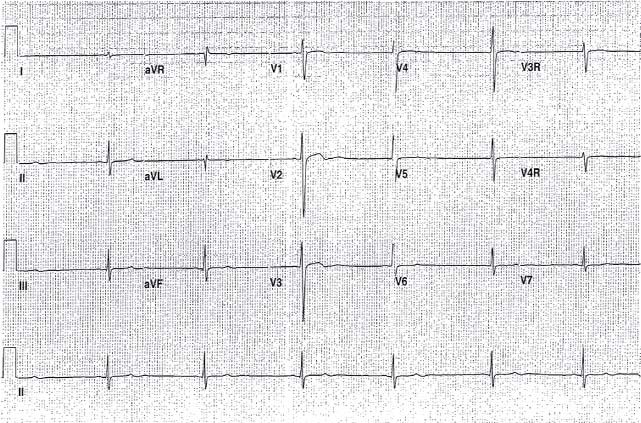
9. A 12-year-old boy presents with a rash with central clearing, some nonspecific joint pain, and the electrocardiogram shown in Figure 6.6. What disease process will most appropriately explain these findings?
A. Rheumatic fever
B. Lyme disease
C. Rocky mountain spotted fever
D. Kawasaki’s disease
E. Systemic lupus erythematosus
10. A 14-year-old patient presents with a syncopal episode. Upon further investigation, you find out that he had been standing on a hot day in church and felt lightheaded before passing out. The event was witnessed and parents describe brief seizure-like activity when he was syncopal. ECG and examination were normal. What is the next step?
A. Implantable loop recorder placement
B. 24-hour ambulatory monitoring
C. Recommend increased fluid intake
D. EP study
E. Neurology referral
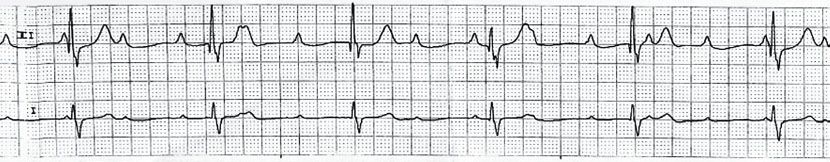
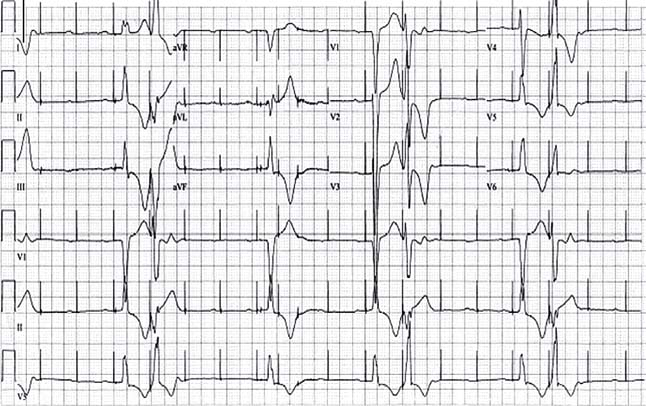
11. A 16-year-old football player comes to you for evaluation of palpitations and dizziness. The ECG shown in Figure 6.7. is obtained. What would you do?
A. Perform a 24-hour cardioscan monitor. If there are no arrhythmias, let him play
B. Permanently disqualify him from all competitive sports based on the ECG
C. Let him play as the ECG findings are a normal variant
D. Not let him play until evaluation including an echocardiogram is performed
E. Let him play and repeat the ECG in 6 months
12. A 12-year-old patient presents with premature atrial contractions on an ECG that was performed after an irregular heart beat was noted on a pre-participation sports physical. There is no significant murmur and a normal examination. Doppler velocity by echo is 2 m/s. What would you let him do?
A. He can participate in all sports
B. No competitive sports
C. He may participate in all sports if his premature atrial contractions can be suppressed by an antiarrhythmic medication
D. He may participate in all sports if he undergoes a successful ablation procedure
E. Mild recreational activities such as golf
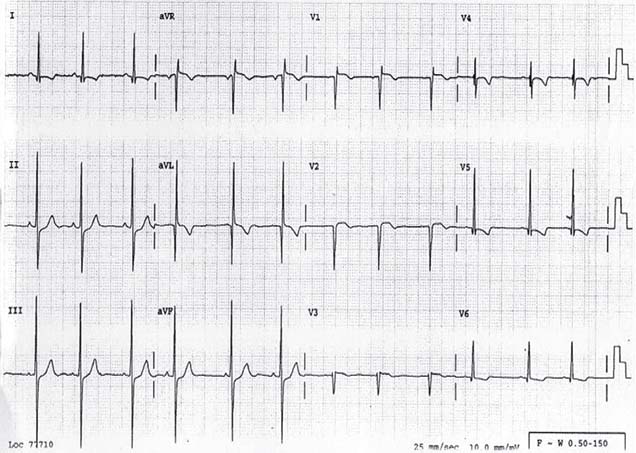
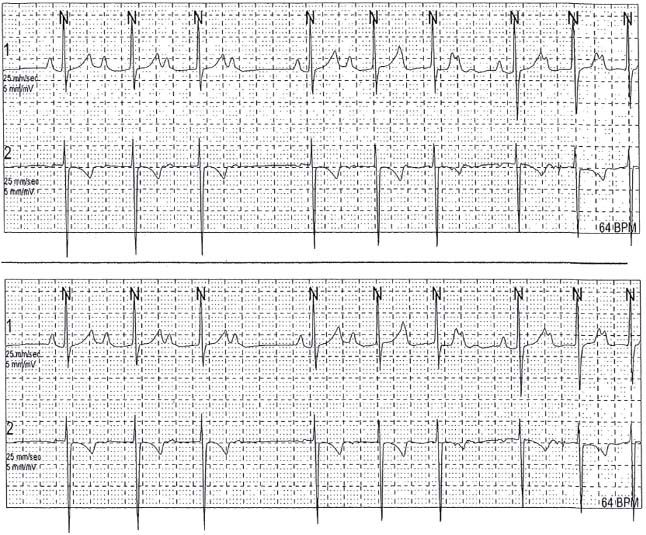
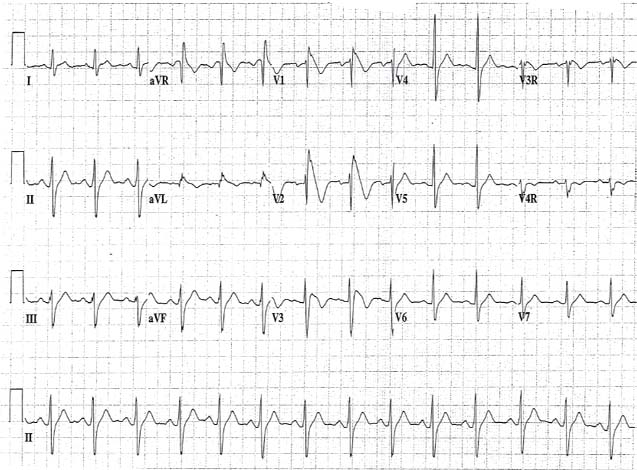
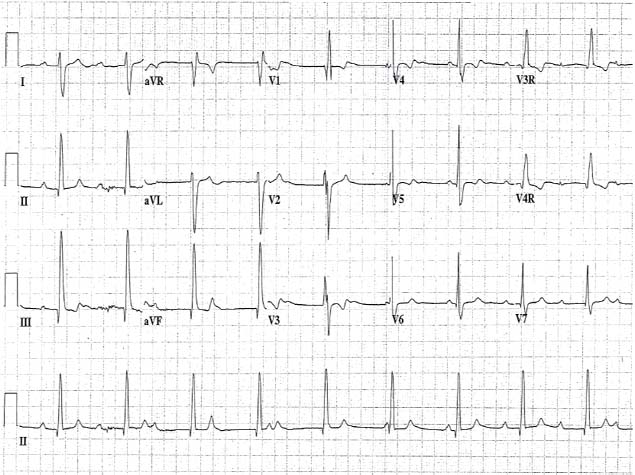
13. A 1-week-old child gets a 12-lead ECG for bradycardia. The ECG recordings are shown in Figure 6.8. The patient is asymptomatic with a good blood pressure, but the corrected QT interval is 503 ms. How would you treat him?
A.Initiation of a β-blocker only
B. Pacemaker placement
C. Follow up in 2 months with a repeat ECG and 24-hour cardioscan monitor
D. Isoproterenol drip
E. Initiation of amiodarone
14. What is the relationship of conduction system lay in a patient with an AV canal?
A. Posterior and superior to the ventricular septal defect
B. Posterior and inferior to the ventricular septal defect
C. Anterior and superior to the ventricular septal defect
D. Anterior and inferior to the ventricular septal defect
E. On the left side of the heart
15. Which of the following findings at 37-week gestation is cause for greatest immediate concern?
A. Fetal heart rate of 110 bpm with no variability on internal fetal monitoring
B. Fetal heart rate of 110 bpm during obstetrical visit
C. Fetal heart rate of 90 per minute heard during an office visit with pulsatile umbilical artery flow
D. Fetal heart rate that decelerates early and synchronously with uterine contractions
E. Fetal heart rate that varies randomly between 120 and 150 per minute during labor
16. Risk of sudden death in patients who have had repair of Tetralogy of Fallot is highest in those with which of the following?
A. QRS duration of 190 ms with residual right ventricular hypertension
B. Frequent premature ventricular contractions
C. Atrial tachycardia on 24-hour cardioscan monitoring
D. Neonatal primary repair with right ventricular outflow tract patch
E. Sinus node dysfunction with right bundle branch block and left anterior hemi block
17. On an ECG in a 10-year-old child with polyarthritis, the PR interval is 220 ms with a heart rate of 108 bpm. This:
A. Makes progression to second-degree AV block likely
B. Supports the diagnosis of acute rheumatic fever
C. Is of no significance unless the QTC interval or QRS duration is abnormal
D. Is a normal finding
E. Is an indication for IVIG therapy
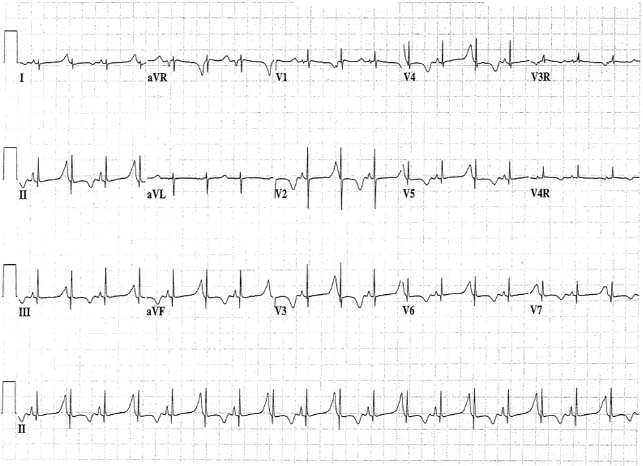
18. Irregular fetal heart sounds are heard during a routine prenatal visit at 32 weeks gestation. Results of fetal ultrasonography suggest appropriate fetal size and development, no evidence of ascites or pleural fluid, and normal fetal scalp thickness. A fetal echocardiographic M-mode tracing is shown in Figure 6.9. The most appropriate management is which of the following?
A. Maternal digoxin therapy
B. Maternal sotalol therapy
C. Maternal flecainide therapy
D. Immediate delivery
E. Observation only
19. A 3-year-old boy has had three episodes of SVT in the past month. Apart from some apprehension and mild pallor, his condition is stable. Heart rate is 240/min. Tachycardia is terminated by one dose of adenosine, intravenously. The electrocardiogram in Figure 6.10. is obtained while the heart is in sinus rhythm. Which of the following drugs should be recommended to prevent a recurrence?
A. Verapamil
B. Oral amiodarone to be taken only after tachycardia starts
C. Digoxin
D. Mexiletine
E. Propranolol
20. Which of the following statements most accurately describes the normal maturation of change in the electrocardiogram during the first week of birth?
A. An increase in the size of the R wave in lead V1
B. A shift in the QRS frontal plane axis from greater than +135 degrees to less than +50 degrees
C. A change in T-wave polarity from positive to negative in lead V1
D. Development of a Q wave in lead V1
E. Shortening of the PR interval
21. In an 8-year-old girl who has persistent junctional reciprocating tachycardia, electrocardiography during an episode of tachycardia would most likely show a P-wave axis of which of the following?
A. −90 degrees
B. 0 degrees
C. 30 degrees
D. +90 degrees
E. +180 degrees
22. A 5-year-old child with diabetes ketoacidosis with a heart rate of 140 bpm. Serum potassium concentration is 8.5 meg/L. The ECG rhythm strip would be expected to demonstrate which of the following?
A. Low amplitude T wave
B. Prominent Q wave
C. Prolonged QRS duration
D. Short PR interval
E. High amplitude P wave
23. A rhythm strip demonstrates a narrow complex tachycardia fluctuating between 180 bpm and 240 bpm with AV dissociation. The patient is 1 day post-op after Tetralogy of Fallot repair. Which of the following is the most likely diagnosis?
A. Atrial flutter with variable AV conduction
B. AV node reentry tachycardia
C. Re-entry supraventricular tachycardia using an accessory pathway
D. Ectopic atrial tachycardia
E. Junctional ectopic tachycardia
24. Which of the following coronary artery abnormalities is most likely to be presented in an asymptomatic 18-year-old high school athlete who dies suddenly on the court during a basketball game?
A. Left circumflex coronary artery arising from the right coronary artery
B. Right coronary artery arising from the pulmonary artery
C. Left main coronary artery originating from the right sinus of Valsalva and passing between the aorta and the pulmonary artery
D. Right coronary artery dominant circulation
E. Anterior descending coronary artery arising from the right coronary artery
25. Which of the following is most likely a result of maternal treatment with amiodarone during pregnancy?
A. Neonatal hypothyroidism
B. Neonatal jaundice
C. Neonatal pulmonary fibrosis
D. Neonatal cataracts
E. Neonatal renal dysfunction
26. Which of the following findings is most likely in a 2.9-kg male infant born to a 36-year-old mother with untreated hyperthyroidism?
A. Sinus tachycardia
B. Junctional tachycardia
C. Complete AV block
D. Ventricular tachycardia
E. Wolff—Parkinson–White syndrome
27. You would advise caution when using which of the following drugs in a patient with long QT syndrome (LQTS)?
A. Lidocaine
B. Amoxicillin with clavulanate
C. Verapamil
D. Erythromycin
E. Metoprolol
28. On a routine physical examination, a 1-month-old infant has a resting heart rate of 220 bpm. There is no murmur and heart size is normal. There is no tachypnea, and blood pressure and perfusion are normal. ECG documents tachycardia with a normal QRS duration and an unvarying RR interval. Ice is applied to the infant’s face without change in the cardiac rhythm. In addition to hospitalization, the most appropriate next step in management would be which of the following?
A. DC cardioversion
B. IV verapamil
C. IV adenosine
D. IV propranolol
E. IV digoxin
29. A 3-week-old infant has had lethargy and poor feeding for 48 hours. On physical examination, the infant is pale and lethargic. Heart rate is 300 bpm, respiratory rate is 60 per minute and blood pressure is not obtainable. Heart sounds are distant, and there is a gallop rhythm. The extremities are cool. Which of the following is the most appropriate initial treatment for this patient?
A. IV amiodarone
B. DC cardioversion
C. IV diltiazem
D. Oral digoxin
E. IV procainamide
30. Which of the following ECG findings constitutes a class I indication for cardiac pacemaker implantation in a 1-day-old male infant with complete AV block, no structural heart disease and normal cardiac function?
A. Ventricular rate of 75 bpm and a QRS duration of 60 ms
B. Atrial rate of 80 bpm and ventricular rate of 65 bpm
C. Atrial rate of 140 bpm and ventricular rate of 65 bpm
D. Ventricular rate of 75 bpm and a corrected QT interval of 440 ms
E. Ventricular rate of 75 bpm and a QRS duration of 120 ms
31. A 14-year-old previously healthy girl collapses while playing soccer. Following successful cardiopulmonary resuscitation, the ECG in Figure 6.11. was obtained. Which of the following is the most likely test to define her diagnosis?
A. Cardiac MRI
B. Measurement of AH and HV intervals on intracardiac electrophysiology study
C. Echocardiogram
D. Genetic testing for KCNQ1 mutation
E. Administration of adenosine
32. In order for re-entry to occur in cardiac muscle and to result in dysrhythmia, which of the following must also be present?
A. An area of conduction delay
B. Delayed depolarization
C. Entrainment
D. Triggered activity
E. Increased automaticity
33. A 6-year-old girl underwent closure of a VSD at 8 months of age. She then did well until the present examination when a slow irregular heart rate was noted. She and her mother report that she has had some dizziness, but no other symptoms. An ECG shows Mobitz type II block and a heart rate of 70 bpm. Which of the following is most appropriate management for this patient’s condition?
A. Theophylline therapy
B. Amiodarone therapy
C. Digoxin therapy
D. Permanent pacemaker placement
E. Observation
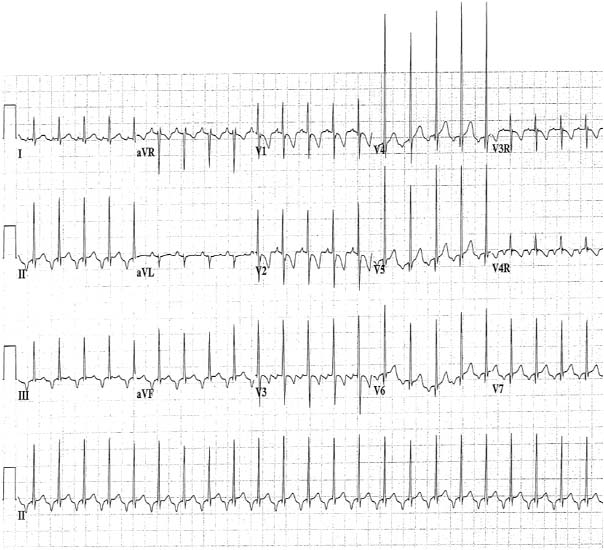
34. A 13-year-old boy presents with the rhythm in Figure 6.12. He underwent an atrial septal defect repair 1 day ago. Blood pressure is 90/56. Which of the following will most likely terminate this arrhythmia?
A. IV adenosine
B. IV labetalol
C. Rapid atrial pacing through atrial pacing wires
D. Oral propranolol
E. Correction of hypokalemia
35. A 9-year-old boy who has a pacemaker is being evaluated by you for the first time. He had previously undergone closure of the VSD. Complete AV block developed post-op. His ECG demonstrates 100% pacing in the ventricular demand VVI mode at the rate of 65 bpm. His parents tell you that his pacemaker has been DDD at a rate of 75 bpm for the past 5 years. Which of the following is the most probable cause for this rate change?
A. Intrinsic variation in the operation of a normal pacemaker
B. Rate responsive pacing
C. Intermittent failure of the pacemaker to capture
D. Spontaneous elective replacement indicator (ERI) of the pacemaker
E. Unintentional reprogramming of the pacemaker
36. Cardiovascular manifestations of hyperthyroidism include which of the following?
A. Heart block
B. Atrial fibrillation
C. Narrow pulse pressures
D. Decrease ejection fraction
E. Low voltage on ECG
37. In pediatric patients, sick sinus syndrome is most likely to be associated with which of the following?
A. Surgery for congenital heart disease
B. Lyme disease
C. Maternal SLE
D. Cardiomyopathy
E. Myocarditis
38. A 12-year-old patient presents for follow-up several years after a sinus venosus atrial septal defect (SVASD) that was repaired surgically. The patient has signs and symptoms of intermittent dizziness. Which of the following is the patient at the highest risk for?
A. Complete AV block
B. Sinus bradycardia and atrial fibrillation
C. Ventricular tachycardia
D. Junctional tachycardia
E. Mobitz type II second degree AV block
39. A 7-year-old patient has a VSD implanted for complete heart block after his surgery. A dual chamber pacemaker is implanted with DDD rate of 60. On examination, you note the patient’s heart rate to be 85 bpm. What is the most likely working mode of this pacemaker at this time?
A. A sense – V sense
B. A sense – V pace
C. A pace – V sense
D. A pace – V pace
E. End-of-life (EOL) battery parameter
40. Which of the following is the most likely side effect of β-blocker therapy in children?
A. Hypothyroidism
B. Behavioral changes
C. Rash
D. Headache
E. Weight loss
41. An 8-month-old patient has the ECG shown in Figure 6.13. with a short PR interval and LV hypertrophy on his ECG. Which of the following is the most likely metabolic disorder?
A. Hunter
B. Hurler
C. Pompe’s disease
D. Phenylketonuria
E. Maple syrup urine disease
42. A 12-year-old patient has corrected transposition (L-transposition) of the great arteries but has not undergone any surgical intervention. This patient is at most risk for which of the following?
A. Sinus node dysfunction
B. Complete AV block
C. Junctional ectopic tachycardia
D. Atrial flutter
E. Torsades de pointes (TdP)
43. It is standard practice to measure the baseline conduction intervals at the beginning and the end of every electrophysiology study. A normal HV interval is usually between which of the following?
A. 120 ms and 200 ms
B. 40 ms and 100 ms
C. 50 ms and 140 ms
D. 35 ms and 55 ms
E. 0 ms and 100 ms
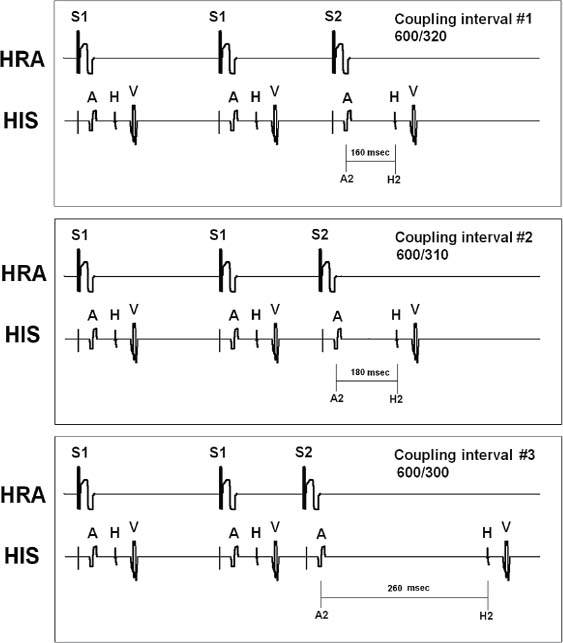
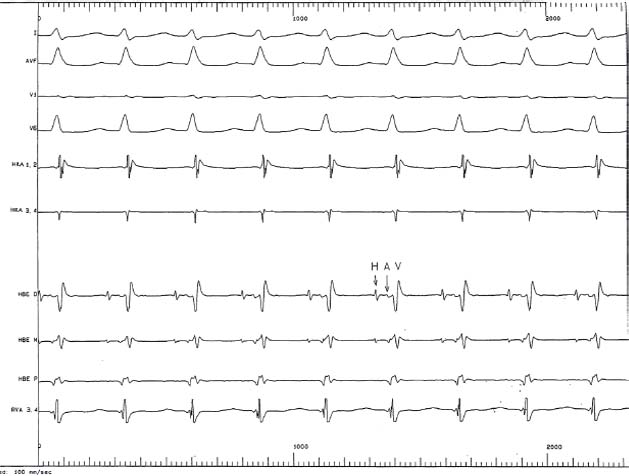
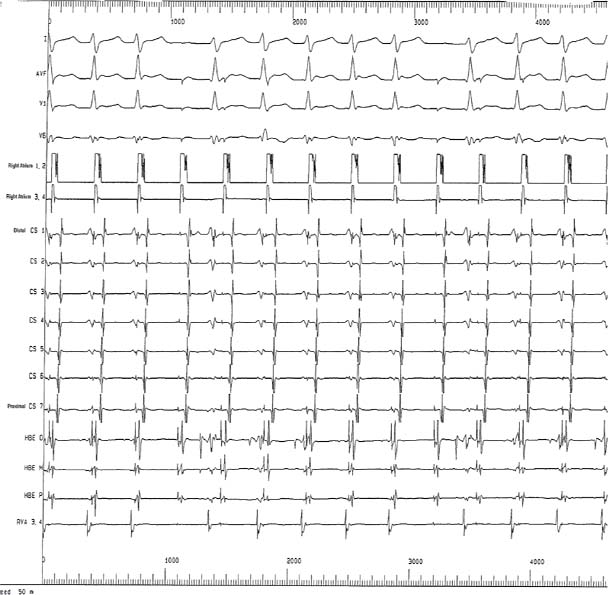
44. During an electrophysiology study, a train of 8 paced beats in the atrium at 600 ms (S1) is followed by a premature beat (S2) at sequentially decreasing cycle lengths. The AH interval is measured after each prematurely paced (S2) beat. This sequence in Figure 6.14. demonstrates:
A. AV node effective refractory period (ERP)
B. A jump in the AH interval indicating dual AV nodal physiology
C. Atrial refractory period
D. Atrial tachycardia
E. Sinus node dysfunction
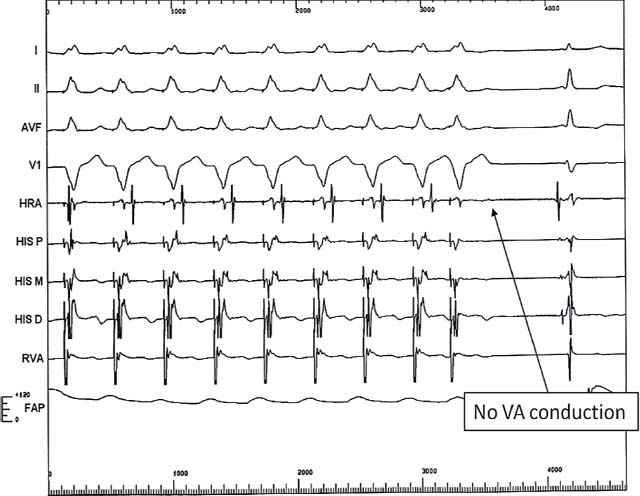
45. In Figure 6.15., a single ventricular extrastimulus protocol in being performed. This sequence shows evidence of what?
A. Ventricle to atrium (VA) ERP
B. Atrial muscle ERP
C. Sinus node recovery time
D. Atrium to ventricle ERP
E. Ventricular muscle ERP
46. The ECG in Figure 6.16. was obtained from a patient with a permanent pacemaker. According to the ECG, the pacemaker is working in what mode?
A. DDD
B. DDD
C. VVI
D. DOO
E. VDD
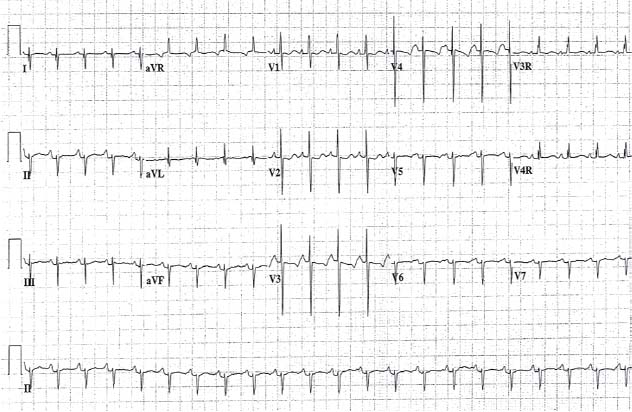
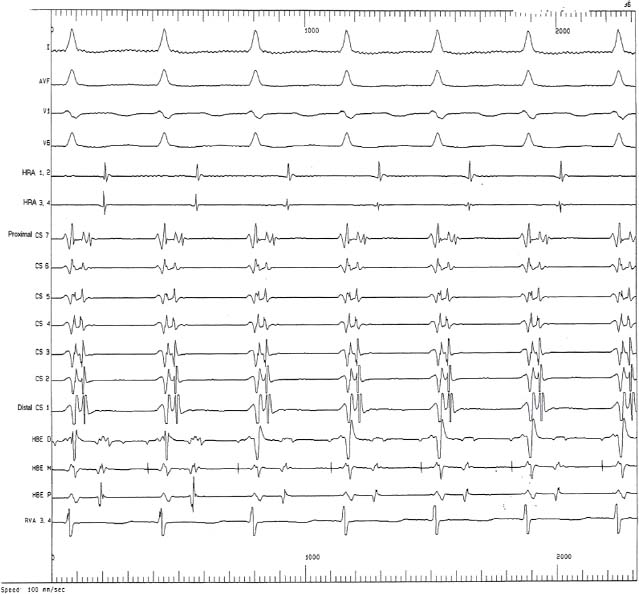
47. A 12-year-old boy has had documented heart rate of 250 bpm. He is brought to the EP lab where a tachycardia is induced with cardiac stimulation. The catheters are in the following positions: RV, right ventricular apex; CS, proximal coronary sinus (CS) with CS 9–10 in the right atrium outside the mouth of the CS; His, bundle of His. The intracardiac tracings in Figure 6.17. are recorded. These are most consistent with which of the following?
A. Ventricular tachycardia
B. AV re-entry tachycardia using an accessory pathway
C. AV nodal re-entry tachycardia
D. Ectopic atrial tachycardia
E. Complete AV block
48. A 12-year-old boy is undergoing a stress test for frequent ectopy at baseline. The echocardiogram at rest was normal. You notice the rhythm in Figure 6.18. at stage 5 of the standard Bruce protocol. The diagnosis is most consistent with which of the following?
A. Brugada syndrome
B. Catecholaminergic polymorphic ventricular tachycardia (CPVT)
C. Long QT type 3
D. Myocarditis
E. Artifact
49. A 12-lead ECG is obtained on this patient with a permanent pacemaker (Fig. 6.19). No information is available on the pacemaker. You conclude that the pacemaker is most likely programmed in which of the following mode?
A. DDD
B. VVI
C. AAI
D. VOO
E. DOO
50. A 3-year-old boy is noted to be bradycardic in the immediate postoperative period after a VSD repair. He is otherwise stable and his blood pressure is within the normal range. The ECG in the Figure 6.20. is obtained. You would advise which of the following?
A. Start epinephrine
B. Start isoproterenol
C. Implant a permanent epicardial pacemaker
D. Use the temporary epicardial pacemaker and observe for at least 7 days.
E. Discharge home with follow-up in 2 weeks
51. Which of the following is an indication for placement of a permanent pacemaker in a patient with no symptoms?
A. PR interval of 250 ms
B. Progressive prolongation of the PR interval followed by a dropped beat
C. No change in the PR interval followed by a dropped beat
D. Sinus rate of 40 bpm
E. Left bundle branch block with a QRS duration of 200 ms
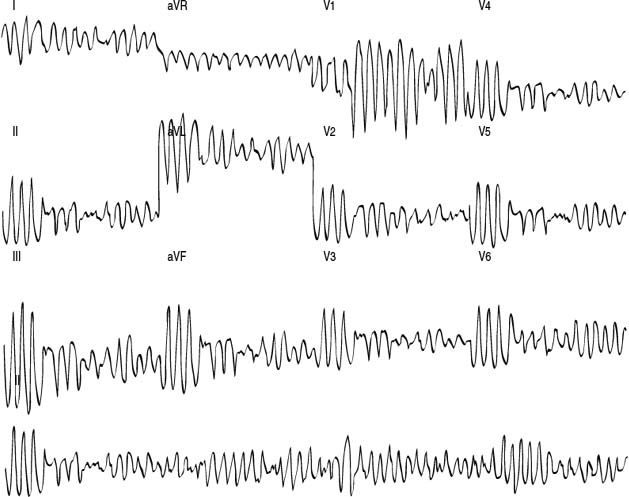
52. A 12-year-old boy has a cardiac arrest while riding his bicycle. He is appropriately resuscitated and brought to the intensive care unit. You notice the rhythm in Figure 6.21. with agitation. His diagnosis is most consistent with which of the following?
A. LQTS
B. CPVT
C. Arrhythmogenic right ventricular dysplasia
D. Brugada syndrome
E. Hypertrophic cardiomyopathy
53. A 2-year-old child with Down’s syndrome had repair of a VSD at 6 months of age and subsequently developed complete heart block. A permanent epicardial pacemaker was implanted. He now presents with irritability and decreased oral intake for 1 day. You obtain the ECG in Figure 6.22. This ECG is most consistent with which of the following?
A. Oversensing
B. Magnet placement over the pacemaker
C. Pacemaker at ERI
D. Pacemaker self-test
E. Intermittent capture of ventricular lead
54. A 16-year-old patient is being started on Amiodarone. The family asks you about potential side effects with this medicine. You would advice them that potential adverse effects of amiodarone include all the following except which one?
A. Photosensitivity
B. Thyroid dysfunction
C. Peripheral neuropathy
D. Corneal micro deposits
E. Kidney dysfunction
55. A 4-year-old child has SVT at rate of 240 bpm and a grade 3/6 holosystolic murmur best heard at the right lower sternal border. EKG in sinus rhythm shows delta wave. What is the most likely underlying heart disease?
A. Ventricular septal defect
B. Ebstein’s anomaly
C. Pulmonary stenosis
D. Corrected transposition of the great arteries
E. Dilated cardiomyopathy
56. A 16-year-old girl presents with dizziness with postural changes, but no syncope. On Holter monitoring, you document a 3.5-s pause during a documented episode of dizziness. The rest of her evaluation including echocardiography and baseline electrocardiogram is normal. What do you do next?
A. Electrophysiology study
B. Tilt table testing
C. Liberalize fluid intake in addition to regular exercise
D. Recommend pacemaker implantation
E. Recommend ICD implantation
57. A 4-year-old child presents with digoxin toxicity and 2:1 heart block. You would consider all the following in the management of this patient except which one?
A. Discontinue digoxin
B. Correct hypokalemia
C. Fab fragments of purified digitalis antibodies
D. Esmolol for ventricular arrhythmias
E. Implantation of permanent pacemaker for life-threatening heart block
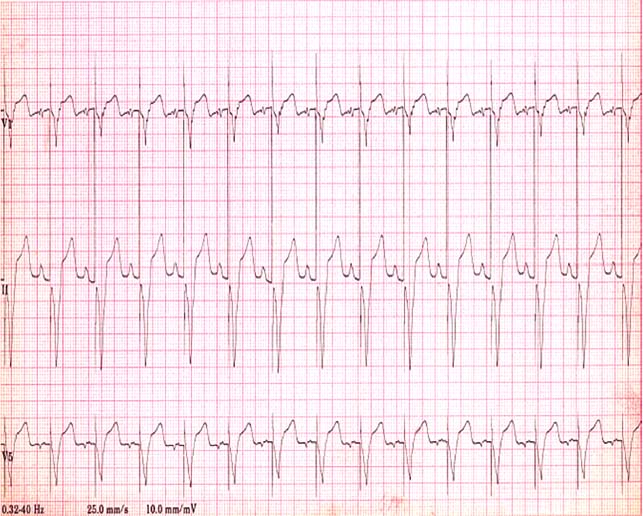
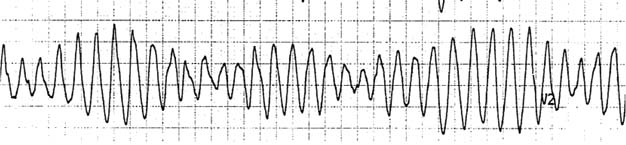
58. An 18-year-old man en route to the hospital by ambulance following his collapse in the street has the rhythm in Figure 6.23. In addition to defibrillation, what would you consider?
A. Digoxin IV
B. Atropine IV
C. Magnesium sulfate IV
D. Potassium IV
E. Adenosine IV
59. Advantages of exercise testing using a cycle ergometer over a treadmill include all the following except which one?
A. It is less prone to cause injury
B.Can obtain higher VO2 max
C. It is easier to obtain blood pressures
D. It is easier to quantify work performed.
E. There is less motion artifact on ECG
60. What does the “R” in DDDR, VVIR, or AAIR represent?
A. Automatic reprogram
B. Mode regulation
C. Reverse polarity
D. Rate response
E. Rapid pacing
61. What would be an appropriate indication for programming a pacemaker AAIR?
A. Third-degree heart block
B. Second-degree heart block
C. Sinus node dysfunction (sick sinus syndrome)
D. First-degree heart block
E. Intermittent third-degree heart block
62. A patient’s implantable cardioverter defibrillator (ICD) is programmed at VVI with a lower rate limit of 80 bpm with a ventricular fibrillation zone of 180 bpm; shock therapy is on. When will the patient receive a defibrillation shock?
A. The heart rate drops below 80 bpm
B. A wide complex rhythm is detected at a rate >80 bpm
C. Sinus tachycardia occurs at 190 bpm
D. Ventricular tachycardia occurs at a rate of 160 bpm
E. Atrial flutter occurs with a rate of 220 bpm and 2 to 1 AV conduction
63. A 13-year-old patient with a pacemaker for complete heart block and no underlying escape rhythm is undergoing surgery for resection of a mass in the abdomen. The surgeon anticipates use of electrocautery during the procedure. A recommendation is made to place a magnet over the pacemaker during the procedure. Which of the following is the reason for making this recommendation?
A. Improves sensing during the procedure
B. Avoids inappropriate pacemaker inhibition due to oversensing from electrocautery during surgery
C. Makes the pacemaker more rate responsive during surgery
D. Deflects the electrical energy from entering the pacemaker generator
E. Prevents overheating of the pacemaker generator
64. A 16-year-old patient has an ICD for hypertrophic cardiomyopathy and cardiac arrest. When asked about the effects of placement of a magnet over an ICD, you would advice that all following are correct except which one?
A. Disables all shock therapy
B. It enables asynchronous pacing in programmed mode
C. Avoids inappropriate shocks due to oversensing from electrocautery during surgery
D. Stops appropriate shock delivery due to ventricular tachycardias including VT/VF
E. The effects are temporary and there only as long as the magnet is placed over the ICD
65. A 15-year-old male collapses while playing basketball. An AED is placed and he is in ventricular fibrillation and receives an appropriate shock which converts him into normal sinus rhythm. His ECG, EST, echo, cardiac MRI, and neurologic exam are normal. His drug screen is negative as is the rest of his evaluation. Which of the following is the next MOST appropriate step?
A. Discharge with follow up in 1 week
B.Discharge on β-blocker therapy
C. Hemodynamic catheterization
D. Placement of an implantable loop recorder
E. ICD place
66. A 17-year-old patient presents after two episodes of syncope and has the ECG in Figure 6.24.
What would be the next most appropriate step?
A.Initiation of a β-blocker
B. Implantation of an ICD
C. Tilt table testing
D. Initiation of amiodarone
E. Implantation of a pacemaker
67. A newborn baby presents with complete AV block. Which of the following is the most likely finding in the mother?
A. Serum potassium of 8
B. Ventricular septal defect
C. Low platelet count
D. Positive rheumatoid factor
E. Ro (SSA) and La (SSB) antibodies
68. The most likely electrolyte abnormality with the ECG in Figure 6.25. is:
A. Sodium
B. Potassium
C. Calcium
D. Magnesium
E. Iron
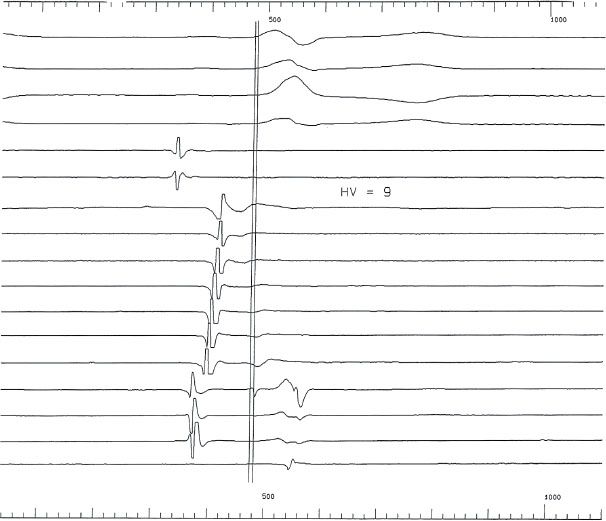
69. The intracardiac electrogram in Figure 6.26. shows an HV of 9 msec. What does this indicate?
A. First-degree AV block
B. Second-degree AV block
C. Infra-Hisian conduction delay
D. Pre-excitation
E. Bundle branch block
70. A 6-year-old boy presents with the ECG shown in Figure 6.27. He is defibrillated back into sinus rhythm. Which drug should be avoided in the future in the patient who presented with this ECG?
A. Propranolol
B. Aspirin
C. Coumadin
D. Lidocaine
E. Erythromycin
71. The next most appropriate step for the newborn patient with the ECG in Figure 6.28. is which of the following?
A. Cardioversion
B. Adenosine
C. Ventricular pacing
D. Lidocaine
E. Verapamil
72. The neonate with the ECG in Figure 6.28 most likely has:
A. Complete AV canal
B. Ventricular septal defect
C. Electrolyte abnormality
D. No structural heart disease
E. Absence of the radius on radiograph
73. The patient with the ECG in Figure 6.29. is most at risk for which of the following?
A. Stroke
B. Torsade de pointes
C. Liver failure
D. Complete AV block
E. Pulmonary fibrosis
74. An asymptomatic 14-year-old patient with a normal examination and resting ECG has a 24-hour cardioscan monitor showing the finding in Figure 6.30. while sleeping. The rest of the Holter is normal. Which of the following is the next most appropriate step?
A. EP study
B. Exercise treadmill test
C. Reassurance
D.Initiation of a β-blocker
E. Pacemaker implantation
75. An asymptomatic 10-year-old patient has the ECG shown in Figure 6.31. during an exercise treadmill test. His resting ECG shows pre-excitation. What does this tracing indicate?
A. The patient is at low risk for sudden death
B. The patient is at high risk for sudden death
C. The patient is at low risk for supraventricular tachycardia
D. The patient is at high risk for supraventricular tachycardia
E. The patient has ventricular tachycardia rather than pre-excitation
76. The patient with the tracing in Figure 6.32. likely has which of the following?
A. Normally functioning DDD pacemaker
B. Atrial lead dysfunction
C. Ventricular lead dysfunction
D. Atrial and ventricular lead dysfunction
E. Bi-ventricular pacemaker
77. The underlying diagnosis in the patient in Figure 6.33. is most likely to be which of the following?
A. Wolff–Parkinson–White
B. Renal failure
C. Atrial septal defect
D. Thyroid storm
E. Anorexia nervosa
78. The intracardiac tracing in Figure 6.34. shows which of the following?
A. Atrial flutter with 2:1 conduction
B. SVT using an accessory pathway
C. Atypical AV node reentry tachycardia
D. Typical AV node reentry tachycardia
E. Normal sinus rhythm
79. A newborn infant presents with abnormal facies and the ECG in Figure 6.35. Which of the following is the most likely cardiac diagnosis?
A. Truncus arteriosus
B. Total anomalous pulmonary venous return
C. Tetralogy of Fallot
D. Coarctation of the aorta
E. Complete AV canal
80. The patient with the ECG in Figure 6.36. is most at risk for which of the following?
A. Pulmonary hypertension
B. AV node reentry tachycardia
C. Intracranial tumor
D. Polysplenia
E. Aortic regurgitation
81. The patient with the ECG in Figure 6.37. most likely will have which of the following?
A. Hypertonia
B. Hepatomegaly
C. Widely spaced nipples
D. Aniridia
E. Hematuria
82. A 17-year-old patient presents with two episodes syncope with no warning signs and no underlying discernable cause. He has the ECG shown in the Figure 6.38. What is the next most appropriate step?
A. Cardiac catheterization with coronary angiography
B. Initiation of atenolol
C. ICD
D. Initiation of amiodarone
E. Reassurance and discharge from clinic
83. The most likely genetic defect with the ECG in Figure 6.38 is which of the following?
A. HERG mutation
B. KCNQ1 mutation
C. 22Q11 deletion
D. Trisomy 21
E. SCN-5A mutation
84. Which of the following is the drug most likely to bring out this finding on ECG (Fig. 6.38)?
A. Epinephrine
B. Lidocaine
C. Esmolol
D. Adenosine
E. Procainamide
85. The intracardiac tracing in Figure 6.39., performed during atrial pacing in the high right atrium (HRA), shows which of the following?
A. Wenckebach (Mobitz type I second degree AV block)
B. Initiation of supraventricular tachycardia
C. AH jump (ERP of the fast pathway of the AV node)
D. Loss of pre-excitation
E. Initiation of atrial fibrillation
86. A patient has a pacemaker set with a lower rate limit of 60. The ECG tracing in Figure 6.40. shows which of the following?
A. Appropriate DDI pacemaker function
B. Inappropriate AAI pacemaker function
C. Inappropriate VVI pacemaker function
D. Appropriate DDD pacemaker function
E. Appropriate AAI pacemaker function
87. A previously asymptomatic patient presents with the ECG shown in Figure 6.41. The patient most likely has an underlying diagnosis of which of the following?
A. Ebstein’s anomaly
B. Atrial septal defect
C. LQTS
D. Arrhythmogenic right ventricular dysplasia
E. Truncus arteriosus
88. Which drug is relatively contraindicated with this ECG (Fig. 6.41)?
A. Amiodarone
B. Adenosine
C. Flecainide
D. Fentanyl
E. Diphenhydramine
89. A 13-year-old patient presents with fatigue and exercise intolerance with a normal echocardiogram. The presenting ECG is shown in Figure 6.42. This patient will most likely require which of the following?
A. Pacemaker
B. ICD
C.β-Blocker therapy
D. Left stellate ganglionectomy
E. Cardiac transplantation
90. Which of the following is NOT associated with the ECG in the Figure 6.42.?
A. Chagas disease
B. Congenitally corrected transposition of the great arteries
C. Maternal Ro and La antibodies
D. Hypertrophic cardiomyopathy
E. Endocarditis with abscess formation
91. With adenosine, the tachycardia in the ECG (Fig. 6.43) will likely:
A. Continue with only P waves in a saw tooth configuration
B. Terminate followed by several sinus beats then restart
C. Slow transiently, then speed up
D. Have no changes
E. Widen transiently, then narrow
92. Which of the following is NOT in the differential diagnosis for a long RP tachycardia?
A. Atypical AV node reentry tachycardia
B. Atrial tachycardia
C. Mahaim fiber tachycardia
D. Permanent form of junctional reciprocating tachycardia (PJRT)
E. Atrial flutter
93. The intracardiac tracing in Figure 6.44. was obtained in a patient after placement of catheters. The proximal CS catheter is placed 2 mm inside the mouth of the CS. The tracing shows which of the following?
A. Supraventricular tachycardia due to a right sided accessory pathway
B. Supraventricular tachycardia due to a left sided accessory pathway
C. Atypical AV node reentry tachycardia
D. Normal sinus rhythm
E. Wenckebach
94. Which of the following is NOT true in the patient with the ECG in Figure 6.45.?
A. Patient is at risk for sudden death
B. Patient should NOT be given methadone
C. Family members should be screened for the same condition
D. The underlying problem is likely due to a mutation in a calcium channel
E. The patient is at risk for 2:1 AV block
Answers
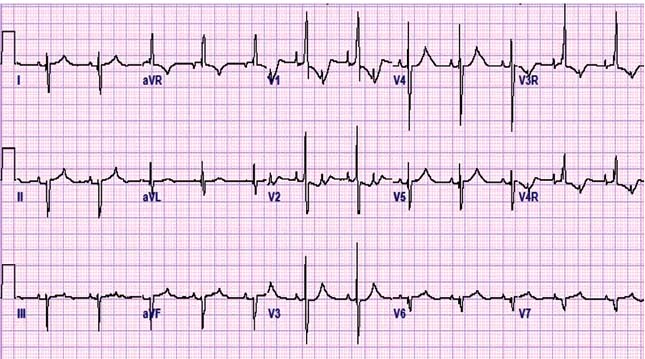
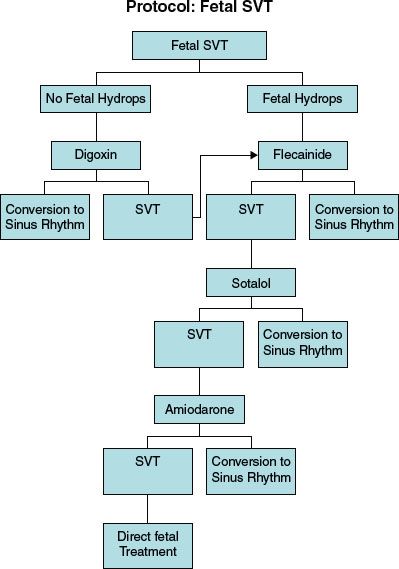
1. ANSWER: D. The M-mode tracings show an atrial flutter with two atrial contractions for every ventricular contraction. Treatment is recommended for sustained arrhythmia or evidence of hydrops (Fig. 6.46). Digoxin is usually first-line agent if no hydrops present with case series reports of 60% to 80% positive responders. Other agents used in the treatment of atrial flutter include flecainide, sotalol, and amiodarone. 1
2. ANSWER: A. The Kearns–Sayre syndrome (characterized by its onset before the age of 20 years, chronic ophthalmoplegia, pigmentary retinal degeneration and at least one of the following symptoms: ataxia, heart block, and high protein content in the cerebrospinal fluid) is a severe variant of chronic progressive external ophthalmoplegia with frequent rearrangements of the mitochondrial DNA (mtDNA). Patients typically present with a bundle branch block and prolonged QT interval that progress to complete heart block. Prophylactic pacemaker therapy is advisable in patients suffering from the Kearns–Sayre syndrome, who have bifascicular block on the precordial electrocardiogram as they may rapidly progress to complete AV block.2 Although they are at risk for AV block, there is no indication for a prophylactic ICD. Steroids or an electrophysiology study is of no benefit.
3. ANSWER: B. β-Blockers are the first-line therapy for LQTS. β-Blockers are useful for minimizing the adrenergic stimulation that results in rapid changes in heart rate with dispersion of repolarization across the myocardium and after depolarizations that are believed to be the inciting events for TdP. The efficacy and safety of ICDs in patients with LQTS have been shown in several studies, but the co-morbidity cannot be ignored, especially in children. Both inappropriate and appropriate shocks may produce severe emotional distress that may trigger additional arrhythmic events and ICD shocks causing an electrical storm. It is important to remember that ICDs are not a substitute for β-blockers that remain the primary treatment for LQTS.
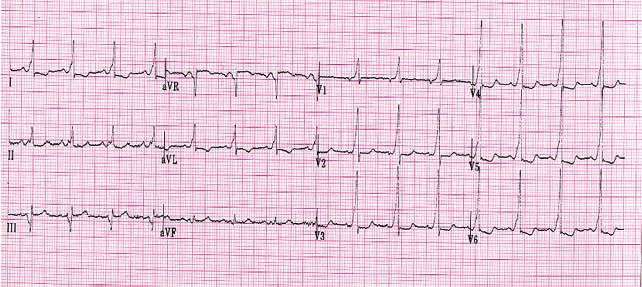
4. ANSWER: E. The rhythm strip demonstrates 2:1 atrial flutter converting to 4:1 atrial flutter with adenosine. Although digoxin can be used to slow the ventricular response with atrial flutter, direct current cardioversion is the most effective method for terminating this arrhythmia. Sotalol, β-blockers or amiodarone can be used, but in infants, this arrhythmia has a low incidence of recurrence, and these medications may take a period of time to be effective, cardioversion is the most reasonable option.
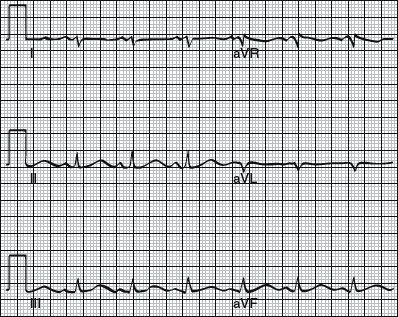
5. ANSWER: D. Children with DiGeorge syndrome and hypocalcemia are prone to having seizures from hypocalcemia. A rhythm strip during the seizure may have artifact that will appear as a supraventricular or ventricular tachycardia. Careful marching of the QRS complexes will show an underlying sinus rhythm.
6. ANSWER: D. A number of risk markers are used to assess the magnitude of risk for sudden death in patients with hypertrophic cardiomyopathy, including family history of premature sudden death; extreme LV hypertrophy (>30 mm) in young patients; nonsustained ventricular tachycardia on Holter electrocardiographic recording; unexplained (not neurally mediated) syncope, particularly in young patients; and blood pressure decrease or inadequate increase during upright exercise. Family history of multiple sudden deaths carries an increased risk of sudden death.3
7. ANSWER: A. Amiodarone increases warfarin effect, digoxin and phenytoin levels, and class I antiarrhythmic toxicity. Digoxin is excreted primarily by the kidneys. Digoxin dose should be reduced when given in conjunction with amiodarone. There is no significant interaction between ACE inhibitors or furosemide and amiodarone.
8. ANSWER: C. This patient is at risk for having episodes of supraventricular tachycardia. The Holter tracing shows a sinus beat alternating with a preexcited beat (short PR interval and delta wave). In patients with WPW the preexcitation can often be intermittent and picked up when monitoring for longer periods such as on a Holter monitor. Patients with WPW are at risk for having episodes of supraventricular tachycardia. Although it is possible that these are premature ventricular contractions, the PR interval is exactly the same on all the beats with the wider QRS complex, making pre-excitation much more likely. There is no evidence of an atrial arrhythmia.
9. ANSWER: B. In patients with Lyme disease, the incidence of cardiac involvement has been estimated to be 8% and usually occurs within a few weeks of the onset of the illness. The most common feature of Lyme carditis is AV block. The AV block usually resolves gradually with normalization of the PR interval in 1 to 2 weeks. Persistence of AV block requiring a pacemaker is unusual.4
10. ANSWER: C. Neurocardiogenic syncope is very common in the teenage years. These patients may have a seizure when syncopal. In the presence of a single episode and clear history suggesting neurocardiogenic syncope, no further workup may be necessary. Recommending liberalization of fluid intake may be adequate. A neurology referral is not necessary if history is strongly suggestive of neurocardiogenic syncope. Myoclonic jerks are occasionally seen with syncope.
11. ANSWER: D. T-wave inversion on an ECG may be a marker for abnormal ventricular myocardium. The ECG is most consistent with hypertrophic cardiomyopathy. T-wave inversion in the left precordial leads (V5 and V6) is almost always an abnormal finding. The forces are suggestive of increased LV hypertrophy (notice that the ECG is half standard in the precordial leads). A complete workup including an echocardiogram to evaluate the coronary arteries is necessary before clearing the patient for sports.
12. ANSWER: A. Premature atrial contractions are a benign finding and are present in many otherwise healthy adolescents. Although a very small percentage may have an atrial tachycardia, the finding of isolated premature atrial contractions does not require any restriction for athletic participation.
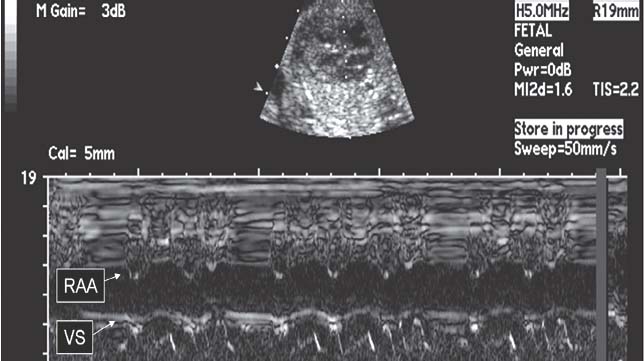
13. ANSWER: B. The ECG demonstrates pseudo 2:1 AV block that has been reported with LQTS. Two-to-one AVB seems preferentially associated with HERG mutations, either isolated or combined. LQTS with relative bradycardia attributable to 2:1 AVB has a poor prognosis during the first month of life. In contrast, sinus bradycardia seems to be associated with KCNQ1 mutations, with a good short-term prognosis under BB therapy. Mutations of cardiac ion channel genes cause LQTS, manifesting as increased risk of ventricular tachycardia and sudden death. Because of the bradycardia and severity of the phenotype, the prognosis is generally poor. β-blocker therapy alone can have serious side effects including enhancing the AV block. Hence, β-blocker therapy along with pacemaker implantation is recommended, although a β-blocker may be added to decrease the chance of ventricular arrhythmias.5 There is no indication for isoproterenol in a stable patient. Amiodarone may lengthen the QT interval and is relatively contraindicated in LQTS.
14. ANSWER: B. The course of the AV node and His purkinje system in endocardial cushion defects passes through the central fibrous body beneath the crest of the VSD. It is therefore displaced posteriorly and inferiorly. In the frontal plane, the initial QRS vector forces are usually directed inferiorly to the right, and the QRS loop moves counterclockwise, superiorly and to the left. The mean QRS axis in the frontal plane ranges between −30° and −120°, with most axis directed between −30° and −90°.6
15. ANSWER: A. The normal baseline heart rate of the human fetus falls between 120 and 160 bpm. Normal short-term variability consists of beat to beat variability of 2 to 3 bpm around the baseline. Long-term variability consists of fluctuations in baseline heart rate occurring 3 to 5 times per minute, with an amplitude of 5 to 20 bpm. Normally, an increase in fetal blood pressure (such as during labor) leads to bradycardia by initiating a vagal nerve reflex. Fetal hypoxemia can have a direct depressing effect on the function of the central nervous system and fetal myocardium, which can result in decrease or loss of fetal heart rate variability.7
16. ANSWER: A. Predictors of long-term survival after Tetralogy of Fallot repair include older age at operation, a higher ratio of right ventricular to LV systolic pressure after surgery, use of an outflow tract patch, a QRS duration >160 ms, and higher preoperative New York Heart Association class.8, 9 The presence of premature ventricular contractions does not increase the risk of sudden death.
17. ANSWER: B. A PR interval of 220 ms is prolonged. ECG evidence of PR interval prolongation in a 10-year-old child with polyarthritis is a minor criterion for Jones criteria for acute rheumatic fever. To make a diagnosis of acute rheumatic fever, you need two major or one major and two minor criteria. The clinical manifestations of acute rheumatic fever follow the inciting group A streptococcal infection after a period of latency of about 3 weeks. Rheumatic fever is a multisystem disease affecting primarily the heart, the joints, the brain, and the cutaneous and subcutaneous tissues. Carditis associated with acute rheumatic fever is seen in ~50% of the patients. Tachycardia is one of the early signs of myocarditis. Complete heart block is not usually seen in rheumatic carditis.10
18. ANSWER: E. Premature atrial beats are common in the fetus and the neonate and do not warrant any therapy. The incidence of premature beats detected in utero is approximately 2%, with <10% of these arrhythmias persisting in the newborn. In the fetus, PACs account for 80% to 90% of premature beats. In the newborn, premature ventricular contractions are recognized in ~30% of infants with extrasystoles.11, 12
19. ANSWER: E. The electrocardiogram demonstrates findings consistent with WPW. Propranolol is the first-line therapy for SVT in patients with WPW. Digoxin and verapamil are relatively contraindicated in the presence of WPW as it may increase the risk for ventricular fibrillation.13 Flecainide is a second-line agent if β-blockers are not responsive. Mexiletine is a class IB antiarrhythmic not indicated for SVT. Amiodarone has a very long half-life and takes several days to build up a therapeutic level orally. Therefore, a “pill in pocket” strategy will likely not be effective.
20. ANSWER: C. A change in T-wave polarity from positive to negative in the right precordial leads describes the normal maturation of change in the electrocardiogram during the first week of birth. The positive T-wave in lead V1 in the first days of life most likely results from early appearance of repolarization in the left ventricle and the late termination of depolarization in the right ventricle. An overall left ventricle to right ventricle sequence results, and this accounts for the upright T wave in lead V1 in the normal term infant.14 The axis will shift to the left, but not to less than 55°. There are decreased right ventricular forces so the R wave will typically get smaller in lead V1. The PR interval remains the same, although it will lengthen with age.
21. ANSWER: A. Permanent junctional reciprocating tachycardia (PJRT) with retrograde P waves will demonstrate P waves with a negative polarity in lead II. This will be closest to −90°. PJRT is an incessant variant of AV reciprocating tachycardia. It usually perpetuates continuously with only brief interruptions that often last for no more than a few sinus beats. The ECG pattern of a normal PR interval and inverted P waves in the inferior ECG leads (II, II aVF) is characteristic of PJRT.15
22. ANSWER: C. At K of 5.5 to 6.5 mEq/L, the T waves become tall and peaked. At serum K level above 6.6 mEq/L, QRS widening along with ST segment elevation is noted. Above 8.5 mEq/L the P waves disappear. At ~9 mEq/L, arrhythmias begin: AV block, ventricular tachycardia, and ventricular fibrillation.16
23. ANSWER: E. Junctional ectopic tachycardia is the most common arrhythmia in the acute postoperative period after congenital heart surgery. It is a focal tachycardia with gradual warm up and cool down and rate variability. The P waves may be within the QRS or dissociated. The rate generally fluctuates between 180 and 240 bpm.17
24. ANSWER: C. The most common coronary anomaly, accounting for one-third of all coronary anomalies is the origin of the left circumflex coronary artery from the right main coronary artery. This has no general clinical significance. Much less common (accounting for 1% to 3% of coronary anomalies) but of greater clinical significance is the origin of the left main coronary artery from the right sinus of valsalva. The LMCA can take four potential pathways: (1) posterior to the aorta, (2) anterior to the RVOT, (3) within the ventricular septum beneath the RV infundibulum, and (4) between the aorta and the pulmonary artery. When the LMCA passes between the aorta and the pulmonary artery, it is associated with sudden death.18
25. ANSWER: A. Neonatal thyroid abnormalities (hyperthyroidism or hypothyroidism) are the most common sequelae of maternal treatment with amiodarone. There is no significant impact to the neonatal liver, lungs, eyes, or kidneys.19
26. ANSWER: A. Sinus tachycardia is the most likely in an infant of mother with untreated hyperthyroidism. This is secondary to increased maternal TSH influencing the neonate.
27. ANSWER: D. Erythromycin is associated with prolongation of the QT interval. In patients with baseline prolonged QT intervals, care should be taken to avoid administration of any medications that have been implicated in drug induced TdP, including QT prolonging antiarrhythmic drugs, tricyclic antidepressants, erythromycin, terfenadine, and chloral hydrate.20
28. ANSWER: C. Adenosine has a half-life of 2 to 10 s and is an excellent drug for acute termination of reentry SVT or diagnosis of atrial arrhythmias such as atrial flutter. DC cardioversion would be indicated in a hemodynamically unstable patient. Verapamil is contraindicated in infants <1 year of age. Propranolol is used for long-term prevention of SVT. Amiodarone may be used when other first-line agents have failed or if the patient is unstable. IV digoxin may be proarrhythmic and is not generally given as a first-line agent.
29. ANSWER: B. DC cardioversion would be indicated in a hemodynamically unstable patient. It would be difficult and time consuming to try and obtain an IV in this patient for administration of amiodarone, digoxin, or procainamide, and these medications may take time to work, causing a further deterioration in the hemodynamic status. Diltiazem is a calcium channel blocker and contraindicated in children <1 year of age.
30. ANSWER: E. A wide QRS escape rhythm in a patient with complete heart block is a class 1 indication for a pacemaker. The class 1 recommendations for permanent pacing in children, adolescents, and patients with congenital heart disease are as follows21:
1. Advanced second- or third-degree AV block associated with symptomatic bradycardia, ventricular dysfunction, or low cardiac output.
2. Sinus node dysfunction with correlation of symptoms during age-inappropriate bradycardia. The definition of bradycardia varies with the patient’s age and expected heart rate.
3. Postoperative advanced second- or third-degree AV block that is not expected to resolve or persists at least 7 days after cardiac surgery.
4. Congenital third-degree AV block with a wide QRS escape rhythm, complex ventricular ectopy, or ventricular dysfunction.
5. Congenital third-degree AV block in the infant with a ventricular rate <50 to 55 bpm or with congenital heart disease and a ventricular rate <70 bpm.
6. Sustained pause-dependent VT, with or without prolonged QT, in which the efficacy of pacing is thoroughly documented.
31. ANSWER: D. Long QT 1, the most common form of long QT presents as syncope or arrhythmias with exercise. The ECG in this patient clearly shows a long QT interval. Genetic testing may reveal a cause in about 75% of patients with a high index of suspicion for LQTS. Echocardiogram and MRI are unlikely to reveal a cause, and there are typically no abnormalities of the AH or HV intervals in patients with LQTS.
32. ANSWER: A. For SVT to occur there need to be two pathways with differences in conduction properties and refractory periods. Entrainment is a form of mapping reentry tachycardias and triggered activity and increased automaticity are properties of focal tachycardias.
33. ANSWER: D. Postoperative heart block carries a high mortality if a pacemaker is not implanted. The postoperative heart block can be intermittent. In the presence of second-degree type II heart block and symptoms, a pacemaker is warranted.22 Digoxin and amiodarone may worsen AV conduction. There is no indication for theophylline therapy I treatment of AV block in the current era.
34. ANSWER: C. Atrial flutter has traditionally been characterized as a macro re-entrant arrhythmia with atrial rates between 240 and 400 bpm. The ECG usually demonstrates a regular rhythm, with P waves that can appear saw-toothed, also called flutter waves. Since the AV node cannot conduct at the same rate as the atrial activity, one commonly sees some form of conduction block, typically 2:1 or 4:1. This block may also be variable and cause atrial flutter to appear as an irregular rhythm. Atrial flutter is a common manifestation in patients having undergone atrial surgery. DC cardioversion is the most effective way to terminate atrial flutter and would be indicated in a patient with hemodynamic instability. An alternative to this is atrial overdrive pacing that may be done through atrial pacing wires in the postoperative setting, although there is a risk of inducing atrial fibrillation. Adenosine and digoxin will block the ventricular response, but not typically terminate the arrhythmia. Correction of hypokalemia is unlikely to terminate the arrhythmia.
35. ANSWER: D. The ERI is set when the battery voltage drops below a certain limit. From this point on, it paces at a rate lower than the set rate. The rate is different for each pacemaker. The pacemaker may change from dual chamber to a single chamber pacing mode as well to conserve battery life. From the point that the ERI is set, the pacemaker will operate at ERI conditions for at least 3 months. As the battery is further depleted, erratic pacing will ensue and the pacemaker is at EOL mode, and the pacemaker will further conserve battery life by turning off all actions except pacing. The patient should be scheduled for pacemaker replacement when the ERI is first reached.
36. ANSWER: B. Atrial fibrillation occurs in 10% to 15% of patients with hyperthyroidism. Low serum thyrotropin concentration is an independent risk factor for atrial fibrillation. Thyroid hormone contributes to arrhythmogenic activity by altering the electrophysiological characteristics of atrial myocytes by shortening the action potential duration, enhancing automaticity and triggered activity in the pulmonary vein cardio myocytes.23 Decreased voltages on an ECG can result from hypothyroidism. There is usually a hyperdynamic state with an increased pulse pressure and hypercontractile function.
37. ANSWER: A. Surgery within the atrium can result in damage to the sinus node. The risk for sinus node dysfunction is directly related to the extent of surgery within the atrium. Patients after an atrial switch or Fontan procedure are at greatest risk for sinus node dysfunction. Lyme disease, maternal SLE, and myocarditis are more commonly associated with AV block. Patients with cardiomyopathy may present with atrial and ventricular arrhythmias.
38. ANSWER: B. Sinus node dysfunction is the most common arrhythmia after ASD repair. SVASD differs from secundum atrial septal defect by its atrial septal location and its association with anomalous pulmonary venous connection. The SVASDs tend to have a higher incidence of sinus node dysfunction. In one study, at follow-up after SVASD repair, 6% of patients had sinus node dysfunction, a permanent pacemaker, or both, and 14% of patients had atrial fibrillation. Older age at repair was predictive of postoperative atrial fibrillation.24
39. ANSWER: B. The Heart Rhythm Society and the British Pacing and Electrophysiology Group (BPEG) have developed a code to describe various pacing modes. This is a series of letters used to describe how the pacemaker is programmed. The first position denotes the chamber(s) paced, and the second position denotes the chamber(s) sensed. The third position indicates the response of the pacemaker to a sensed event (I-inhibit or T-track). A DDD pacemaker paces both atrium and ventricle, senses both atrim and ventricle and both inhibits as well as tracks in response to a sensed event. As the heart rate of the patient is higher than the set rate limit of the pacemaker, the device is sensing the native atrial rate at a rate of 85 bpm and triggering the ventricle to pace at the same rate. This patient has complete AV block; hence, intrinsic conduction (V sense) is not likely.
40. ANSWER: B. Behavioral changes, depression, and mood swings are the most common side effects of β-blockers in children. Other less common side effects include lightheadedness, tiredness, headaches, nightmares, difficulty sleeping, heartburn, diarrhea, or constipation. Amiodarone, rather than β-blockers, causes hypothyroidism.
41. ANSWER: C. Pompe’s disease is a glycogen storage disease type II. It is the most severe and lethal form of hypertrophic cardiomyopathy being uniformly fatal within the first 2 years of life. These patients appear clinically well at birth, but within 6 months start developing hypotonia, severe cardiomegaly, hepatomegaly, poor weight gain, difficulty sucking, and an enlarged protruding tongue. ECG may show a short PR interval and extremely high QRS voltages suggestive of LV hypertrophy.
42. ANSWER: B. Patients with corrected transposition have a fragile conduction system. The basic anatomy dictates that the AV node cannot give rise to the penetrating AV conduction bundle. There is an anomalous AV node present interiorly underneath the pulmonary valve leaflets. It has a superficial course and sets the stage for development of spontaneous heart block. Approximately 10% of the patients may present in heart block. Spontaneous complete heart block occurs at a rate up to 2% per year in this population. These patients also have an increased risk for Wolff–Parkinson–White.
43. ANSWER: D. The normal HV interval is between 35–55 seconds. A shorter HV interval is seen with ventricular preexcitation (WPW) and a longer HV interval is suggestive of AV node or His purkinje disease.
44. ANSWER: B. By delivering premature atrial stimuli (S2 @ 320, 310, and 300 ms) after a pacing train (S1 @ 600 ms), there should be a small decremental change in the AH interval. However, if there is a large change (>50 ms) in the AH interval with a 10 ms change in the premature atrial stimulus (S2), it suggests dual AV node pathways that is a substrate for AV nodal reentry tachycardia.
45. ANSWER: A. The intracardiac electrocardiogram shows a train of pacing within the ventricle followed by a prematurely paced ventricular beat. The longest cycle length at which this last beat fails to conduct from the ventricle to the atrium is called the VA ERP. Atrial muscle ERP would be the longest cycle length at which the atrial stimulus fails to capture the atrium. Ventricular muscle ERP would be the longest cycle length at which the ventricular stimulus fails to capture the ventricle. AV ERP would be the longest cycle length at which the atrium fails to conduct to the ventricle. Sinus node recovery time measures the time for the first intrinsic sinus node to recover after a pacing train within the atrium is stopped.
46. ANSWER: C. The ECG demonstrates pacing in the VVI mode. The rate is ~70 bpm. The P waves have no relationship to the QRS complex (are dissociated), indicating that there is no sensing or capture of the atrium.
47. ANSWER: A. The surface tracings show a wide complex tachycardia. The atrial electrical signals have no relationship to (are dissociated from) the ventricular electrical signals, and the atrial rate is slower than the ventricular rate. This is therefore a ventricular tachycardia.
48. ANSWER: B. This patient develops polymorphic ventricular tachycardia with exercise. This can be seen with CPVT. Brugada syndrome and long QT type 3 can also result in polymorphic ventricular tachycardia, but this is generally at rest or during sleep. You would expect to see additional findings such as a decrease in cardiac function with myocarditis.
49. ANSWER: A. The ECG demonstrates atrial sensing followed by ventricular tracking and capture. This is a dual chamber pacemaker. The pacing mode is either DDD or VDD. The VDD mode is capable of atrial sensing but not pace in the atrium, and this mode is most useful for patients with isolated heart block and normal sinus node function.
50. ANSWER: D. AV conduction block continues to complicate 1% to 3% of surgical procedures. Unless treated with an implanted pacemaker, permanent postoperative heart block is associated with 28% to 100% mortality. Postoperative heart block often proves to be transient, typically resolving within 7 to 10 days of onset, and it is prudent to wait at least 7 days to determine whether AV nodal conduction will return. Once their AV node recovers, however, these patients should be monitored for long-term development of conduction abnormalities.25, 26
51. ANSWER: C. Mobitz type I second-degree AV block, also referred to as Wenckebach periodicity, is characterized by progressive PR prolongation, usually owing to changes in the AH interval (reflecting AV node delay), with eventual failure of conduction to the ventricle. In contrast, type II AV block refers to abrupt failure of AV conduction of one or more atrial impulses without prior PR prolongation. Type II block usually occurs below the AV node (HV interval block). In addition to the absence of progressive P-R prolongation before block, type II block may abruptly progress to third-degree block with an inadequate escape rhythm and is therefore an indication for a pacemaker, even in the absence of symptoms.27 Sinus bradycardia, Wenckebach, and a prolonged PR interval are not indications for a pacemaker in an asymptomatic patient. Left bundle branch block by itself is not an indication for pacemaker placement, regardless of QRS duration.
52. ANSWER: B. The ECG shows bidirectional ventricular tachycardia. This tachycardia is most consistent with CPVT.
Features of CPVT are as follows: (1) exercise- or emotion-induced severe ventricular tachyarrhythmias, (2) a typical pattern of bidirectional ventricular tachycardia with a normal resting ECG, and (3) a structurally normal heart. Recent reports suggest that CPTV is a genetic disease related to the mutation of two genes: mutations in cardiac ryanodine receptor gene (RYR2) or calsequestrin 2 gene (CASQ2).28
53. ANSWER: E. The findings on this ECG are consistent with intermittent capture of ventricular lead. There are pacing spikes with no capture, ventricular escape beats at a slow rate and intermittent capture of the ventricle by the pacemaker. This is most consistent with a partial fracture of the ventricular lead. The lead impedance will often be out of the normal range when interrogated. This patient will need to be admitted and most likely need a lead revision. Undersensing is the inability of the pacemaker to sense spontaneous myocardial depolarization that results in competition between paced complexes and the heart’s intrinsic rhythm, thus leading to inappropriate pacing. Oversensing refers to the pacemaker sensing artifacts and hence not pacing when indicated. ERI a point in the pacemaker battery life where replacement is voluntary but will continue to operate. Placing a magnet over a pacemaker typically causes it to pace asynchronously, but not lose capture. Typically when a pacemaker performs a testing feature, it will not allow loss of capture for even a single beat.
54. ANSWER: E. Adverse effects of amiodarone include photosensitivity, thyroid dysfunction, weakness, peripheral neuropathy, corneal micro deposits, and elevation of hepatic enzymes. Nausea is common at the initiation of therapy, but generally resolves over time. Photosensitivity is quite common, and patients should be instructed to cover their skin and use skin-blocking agents. Less common but serious side effects include proarrhythmia and pulmonary fibrosis.29 Kidney dysfunction is not a side effect of amiodarone.
55. ANSWER: B. WPW is associated with Ebstein’s disease and with the left-sided tricuspid valve in L-transposition. This association probably has its basis in the embryology of tricuspid valve formation. The leaflets of the AV valves normally develop through a process of undermining, or delamination, of the interior surface of the embryonic ventricular myocardium. Separation of the atrium from the ventricle occurs through completion of this process and encroachment of fibrous tissue from the AV sulcus. The mitral valve and the anterior leaflet of the tricuspid valve are fully delaminated early in development; however, the posterior and septal leaflets of the tricuspid valve are not fully formed even by 3 months’ gestation. Ebstein’s disease appears to occur when there is arrested development.30
56. ANSWER: C. The patient is presenting with neurocardiogenic syncope. All the therapeutic options can be used for treatment of neurocardiogenic syncope. However, fluid liberalization and behavior modification should be the first steps in treatment of symptoms. A majority of the patients will improve with this alone and need no further intervention. A tilt table test is useful only when the diagnosis cannot be made by history alone. Although there is a pause of 3.5 s, without true episodes of syncope a pacemaker is not indicated. An ICD is not indicated in neurocardiogenic syncope. There is no value to an invasive electrophysiology study as this phenomenon is mediated by bradycardia induced by the vagus nerve rather than an arrhythmia.
57. ANSWER: E. Hypokalemia increases digoxin cardiac sensitivity and should be corrected. Patients with hypomagnesemia, hypokalemia, or both may become cardiotoxic even with therapeutic digitalis levels. β-adrenergic blockers can decrease automaticity and slow conduction velocity induced by a catecholamine surge from digitalis intoxication and can shorten the refractory period of atrial and ventricular muscle. In the presence of SA or AV node depression, however, they may depress activity further; therefore, a short-acting β-blocker such as esmolol is recommended in rapid atrial conduction. Temporary pacing (not permanent pacing) is an alternative for patients with nodal blocks before any other medical interventions are attempted. Digibind is a relatively pure Fab product that is very safe and extremely effective. Onset of action ranges from 20 to 90 minutes, and digoxin is removed irreversibly from the myocardium and other specific binding sites. A complete response generally occurs within 4 hours.
58. ANSWER: E. This rhythm strip shows TdP, which is a ventricular tachycardia with a varying QRS amplitude. MgSO4 is a very effective and safe treatment for TdP. Its use is therefore recommended for therapy of TdP. Magnesium can be given at 1 to 2 g IV initially in 30 to 60 s, which then can be repeated in 5 to 15 min. Magnesium is effective even in patients with normal magnesium levels.31
59. ANSWER: B. A treadmill may be more likely to cause injury than a cycle because the subject can fall from the treadmill. Also, it is more difficult to hear the Korotkoff sounds when the subject is running or jogging on a treadmill than when he or she is cycling. If the subject is connected to numerous monitoring devices, cycling may be preferable because it involves less movement of the trunk and extremities. However, this reduced motion of the trunk and extremities also limits the VO2 max on the cycle.32
60. ANSWER: D. The fourth letter of the NBG pacing code represents rate response pacing. The pacemaker uses some type of sensor to detect activity and increases the lower rate limit of pacing in conjunction with the level of activity. When the activity ceases, the pacing returns to the set basal rate. Rate response enables a patient’s pacemaker to vary heart rate when the sinus node cannot provide the appropriate rate to meet the body’s demands. Rate responsive pacing is indicated for patients who have chronotropic incompetence (heart rate cannot reach appropriate levels during exercise or to meet other metabolic demands).
61. ANSWER: C. When the pacemaker is programmed AAIR, it is capable of pacing and sensing only in the atrium. This mode of pacing is indicated only when there is a problem with the sinus node. To correct any degree of heart block, a lead in the ventricle is necessary.
62. ANSWER: C. The patient will receive a defibrillation shock if the ventricular rate goes at or above the programmed shock rate of 180 bpm. In the ventricular fibrillation zone, the patient will receive a shock if the ventricular rate, even if the rhythm is sinus. In addition, the patient will not receive a shock if a ventricular tachycardia occurs at a rate slower than the set shocking rate. An ICD programmed in the VVI mode cannot look at the atrial rate and hence is unable to differentiate between sinus tachycardia and ventricular tachycardia. Sinus tachycardia falling in the VT zone can lead to inappropriate shocks and is the most common reason for inappropriate shocks in patients with an AICD.
63. ANSWER: B. Electrocautery can create inappropriate noise and sensing within the pacemaker thus causing it to oversense and prevent necessary pacing. Placement of a magnet over a pacemaker causes an asynchronous pacing (no sensing, just pacing at the pacemakers magnet rate). This avoids inappropriate pacemaker inhibition due to oversensing from electrocautery during surgery.
64. ANSWER: B. When a magnet is placed over an ICD, it disables shock therapy but pacing is not affected. This is different from when a magnet is placed over a pacemaker which enables an asynchronous pacing. By disabling shock therapy, it avoids inappropriate shocks due to oversensing from electrocautery during surgery. However, it also avoids appropriate shocks due to ventricular tachycardias. The effects are temporary and there only as long as the magnet is placed over the ICD.
65. ANSWER: E. The etiology of a cardiac arrest is not always clear despite extensive testing. In the absence of a known reversible or treatable cause of sudden cardiac arrest, an ICD is the most logical treatment of choice as this patient is at risk for having cardiac arrest again.
66. ANSWER: B. This ECG shows the classic pattern for Brugada syndrome with a right bundle branch block pattern and ST segment elevation in leads V1 and V2. This is a channelopathy affecting ion transport during cardiac conduction. The clinical manifestation of Brugada syndrome is highly variable. Symptomatic patients experience ventricular tachyarrhythmias that may lead to recurrent syncope and/or sudden cardiac death. In symptomatic patients with Brugada syndrome, the ICD is the only life-saving option. β-blockers are not effective at presenting sudden cardiac death.
67. ANSWER: E. CHB detected in utero is strongly associated with maternal antibodies to SSA (Ro) and SSB (La). Their pathogenic role in the development of CHB has been established in several studies. The mothers of affected infants frequently have autoimmune disease (systemic lupus erythematosus, Sjögren’s syndrome) or are entirely asymptomatic. It is very difficult to identify pregnant asymptomatic mothers carrying anti-SSA/SSB antibodies. Although the association of anti-SSA/SSB with CHB is widely accepted, the precise mechanism by which these antibodies cause cardiac conduction abnormalities remains to be defined. Fetal and neonatal diseases are presumed to be due to the transplacental passage of these immunoglobulin G (IgG) autoantibodies from the mother into the fetal circulation. Since these antibodies may have a pathogenic role in CHB, screening of infants with isolated CHB or neonatal lupus and their mothers for the presence of anti-SSA and anti-SSB is strongly recommended.
68. ANSWER: B. The ECG shows a wide complex rhythm at a rate of ~150 bpm. Although P waves are not clearly visible, the rhythm is most consistent with a sinus tachycardia. This patient is severely dehydrated, acidotic, and hyperkalemic. Hyperkalemia produces tall peaked T waves. However, this finding is nonspecific and insensitive because normal children may have peaked T waves, and those with hyperkalemia may not have peaked T waves. As the potassium level increases, the T waves become more peaked and an intraventricular conduction delay results in a widened QRS along with PR prolongation. The resultant ECG may resemble a sine wave or wide ventricular tachycardia. At concentrations of 9 mEq/L atrial standstill, AV bloc and ventricular fibrillation can occur. In addition, there is no differentiation between the QRS and the T wave. This is seen in patients with hypoxia, acidosis, or hyperkalemia. Increased calcium causes a shortened QT interval. The other electrolytes have minimal effect on the ECG.33
69. ANSWER: D. In Wolff–Parkinson–White, there is an accessory connection between the atria and the ventricles bypassing the AV node. These accessory pathways conduct quickly to the ventricles. It normally takes 35 to 70 ms to get through the AV node. A short HV interval (<25 to 35 ms) indicates an alternative method of conduction other than the AV node, that is, an accessory pathway.34
70. ANSWER: E. This ECG shows TdP. In this type of ventricular tachycardia, the QRS complexes change morphology as if it were rotating around a point. This is the classic arrhythmia seen with LQTS. Of the medications on the list, erythromycin is a medicine that prolongs the QT interval and should therefore be avoided in this patient.35
71. ANSWER: A. The ECG shows atrial flutter. The treatment of choice for converting this rhythm is cardioversion. Adenosine will only block the AV node, but the atrial flutter will continue. Ventricular pacing will have no effect on this atrial arrhythmia. Lidocaine has minimal effect on atrial arrhythmias. As the newborn heart is very sensitive to calcium, calcium channel blockers such as verapamil should be avoided as they may result in long pauses and have been associated with sudden death with longer term use.36
72. ANSWER: D. The newborn myocardium has unique properties that allow it to conduct impulses very rapidly. Atrial flutter at very fast rates (up to over 400 bpm) can be maintained in the presence of no structural heart disease. Although it is important to perform an echocardiogram on all patients who present in atrial flutter, the majority of these patients have no underlying structural heart disease and a low incidence of recurrence of atrial flutter.36
73. ANSWER: A. This ECG shows atrial fibrillation with an irregularly irregular rhythm. This rhythm results in no organized atrial contractions and stasis in the atria. This stasis predisposes patients to thrombi and potential strokes. This risk may persist for some period of time, even after sinus rhythm is restored.37
74. ANSWER: C. This tracing shows Mobitz I second-degree AV block (Wenckebach) with progressive prolongation of the PR interval followed by a dropped beat. This finding is not uncommon in teenagers and older adults while sleeping, but is rare while awake. If it occurs in an otherwise asymptomatic person while sleeping, it likely has no clinical significance.38
75. ANSWER: A. This tracing shows loss of pre-excitation in a single beat. The loss in a single beat on an exercise treadmill test indicates an accessory pathway that will not rapidly conduct to the ventricle in atrial fibrillation and is therefore at a low risk for sudden death. The antegrade conduction seen on a resting ECG has no definitive relationship with the retrograde conduction that causes supraventricular tachycardia, and therefore, the risk of SVT cannot be estimated. There is no evidence of ventricular tachycardia.39
76. ANSWER: B. The tracing shows failure of atrial sensing as well as atrial pacing with no evidence of capture. This is indicative of atrial lead dysfunction.40
77. ANSWER: E. This ECG shows severe bradycardia with no other significant abnormalities. The body’s response to nutritional deprivation is to decrease the heart rate. There is no evidence of Wolff–Parkinson–White. Renal failure typically causes electrolyte disturbances that change the QRS or QT intervals. An atrial septal defect usually does not result in severe bradycardia. Thyroid storm involves hyperthyroidism and an elevated heart rate. This ECG could be consistent with hypothyroidism.38
78. ANSWER: D. The intracardiac tracing shows a pattern of activation through the bundle of His, to the atrium followed by the ventricle. This pattern of activation is the classic pattern seen with typical AV node reentry tachycardia.34
79. ANSWER: E. This ECG shows left axis deviation with the S wave being larger than the R wave in lead aVF. Left axis deviation is the classic finding in patients with complete AV canal, primum atrial septal defect, or tricuspid atresia.38
80. ANSWER: A. This ECG shows massive right and left atrial enlargement consistent with restrictive cardiomyopathy. It is very unusual to see this degree of bi-atrial enlargement in any condition other than restrictive cardiomyopathy. Patients with restrictive cardiomyopathy are at risk for pulmonary hypertension. None of the other conditions are associated with this condition.41
81. ANSWER: B. This ECG, which is performed at half standard (any measured voltage should be doubled to determine the true height) shows massive ventricular hypertrophy. There is also a shortened PR interval. These findings are consistent with a glycogen storage disorder, particularly glycogen storage disease type 2 (Pompe’s disease). These patients present with heptatomegaly.42, 43
82. ANSWER: C. This ECG shows a right bundle branch block and ST segment elevation in leads V1 and V2, consistent with Brugada syndrome. It is not related to coronary pathology. In a patient with syncope or documented arrhythmias and a classic Brugada ICD, an ICD is warranted as these patients are at risk for sudden death. β-blockers such as atenolol do not decrease this risk. Amiodarone may exacerbate ventricular arrhythmias.44, 45
83. ANSWER: E. The genetic defect associated with Brugada syndrome results from a mutation in the SCN-5A channel that is a sodium channel. HERG and KCNQ! mutations cause LQTS. 22Q11 deletion is associated with DiGeorge syndrome. Trisomy 21 has no relationship to Brugada syndrome.46
84. ANSWER: E. In patients with Brugada syndrome, Vaughn Williams class I drugs such as procainamide that block the sodium channel may bring out a Brugada-type pattern on ECG. Epinephrine may be useful in identifying patients with LQTS, but not Brugada syndrome.47
85. ANSWER: A. This tracing shows progressive prolongation of the atrium to His (AH interval) and consequentially PR intervals followed by a nonconducted beat. This finding can be created by pacing the atria faster and faster during an atrial pacing protocol. There is no evidence on this tracing of supraventricular tachycardia, atrial fibrillation, an increase in the AH interval, or pre-excitation.34
86. ANSWER: D. This tracing shows appropriate dual chamber pacemaker function. The first letter in the pacemaker code (NBG code) is the chamber paced. The second letter is the chamber sensed. The third is the response to a sensed event (i—inhibit, t—trigger or track or d—both inhibit and track). This tracing shows a native p wave that is followed by an intrinsic atrial event. The device senses the atrium and then triggers a ventricular pace in the ventricle. Therefore, it is a dual chamber device set DDD.40
87. ANSWER: A. This tracing shows an irregular wide complex tachycardia. This is atrial fibrillation in the presence of either a pre-existing bundle branch block or pre-excitation (Wolff–Parkinson–White). The most likely scenario in a previously asymptomatic patient is atrial fibrillation with WPW. Patients with Ebstein’s anomaly have an increased incidence of WPW and are at risk for atrial fibrillation because of their dilated atria. WPW is classically associated with Ebstein’s, congenitally corrected transposition of the great arteries and hypertrophic cardiomyopathy, not the other conditions listed.48
88. ANSWER: B. In the presence of atrial fibrillation and WPW, any drug that can block the AV node, such as adenosine, digoxin, or a calcium channel blocker is relatively contraindicated. This may cause preferential conduction down the accessory pathway resulting in rapid conduction to the ventricle and subsequently ventricular fibrillation.49
89. ANSWER: A. This ECG shows complete AV block. There is no relationship between the P waves and the QRS complexes, the atrial rate is faster than the ventricular rate and there are P waves that should conduct, but do not. There is not a significant enough increase in ventricular arrhythmias to warrant implantation of an ICD in the absence of other risk factors. β-blockers will have little effect and may slow the underlying junctional rate. Left stellate ganglionectomy may have some utility in LQTS, but not complete AV block. Cardiac transplantation is not indicated. A pacemaker is indicated in the presence of symptoms, a wide complex escape rhythm, complex ventricular ectopy, or a heart rate <50 in the absence of congenital heart disease and 70 in the presence of congenital heart disease.50
90. ANSWER: D. Hypertrophic cardiomyopathy is not classically associated with AV block. All the other conditions may result in alterations of AV nodal condution.33
91. ANSWER: B. This ECG shows a long RP tachycardia (the P wave occurs greater than half the distance between two successive QRS complexes). The P waves are deeply negative in leads II, III, and aVF. This is consistent with either the PJRT or atypical AV node reentry tachycardia. Both of these are dependent on the AV node and will break with adenosine. However, both also tend to be incessant and may re-initiate quickly after termination with adenosine. Atrial flutter will continue with only P waves in a saw-tooth pattern after adenosine. Sinus tachycardia will slow transiently, then speed back up. A sinus tachycardia or atrial tachycardia in the presence of pre-excitation may widen transiently as the AV node blocks and there is preferential conduction down the AV node.
92. ANSWER: C. The differential diagnosis for a long RP tachycardia shown includes an atrial tachycardia with a focus in the low posterior right atrium, the PJRT or atypical AV node reentry tachycardia. A Mahaim fiber is an accessory pathway fiber that conducts antegrade only. Mahaim fiber tachycardias present with a wide complex tachycardia. Atrial flutter can also present as a long RP tachycardia.51
93. ANSWER: C. This tracing shows a supraventricular tachycardia. The atrial activation is earliest in the mid CS, which runs along the AV groove between the left atrium and left ventricle. There are no normal structures that connect the atria and the ventricles present in this location. Therefore, this tracing shows supraventricular tachycardia due to a left sided accessory pathway.34
94. ANSWER: D. This ECG shows prolonged QT syndrome with QRS alternans. This is an alternating pattern of appearance of the T waves. This is a poor prognostic sign, and these patients are at risk for both 2:1 AV block (which this patient has on other tracings) as well as sudden death. Methadone prolongs the QT interval and should be avoided. Most cases of LQTS are familial; hence, other family members should be screened. The underlying mutation is typically due to a sodium or potassium channel mutation. Calcium channel mutations may cause CPVT.51
References
1. Batra AS, Loo JC. Fetal arrhythmias. In: Briggs G, Nageotte M, eds. Diseases, Complications, and Drug Therapy in Obstetrics – A Guide for Clinicians. 2009.
2. Polak PE, Zulstra F, Roelandt JR. Indications for pacemaker implantation in the Kearns-Sayre syndrome. Eur Heart J. 1989;10:281–282.
3. Autore C, Quarta G, Spirito P. Risk stratification and prevention of sudden death in hypertrophic cardiomyopathy. Curr Treat Options Cardiovasc Med. 2007;9:431–435.
4. Costello JM, Alexander ME, Greco KM, et al. Lyme carditis in children: presentation, predictive factors, and clinical course. Pediatrics. 2009;123:e835–e841.
5. Horigome H, Nagashima M, Sumitomo N.Clinical characteristics and genetic background of congenital long-QT syndrome diagnosed in fetal, neonatal, and infantile life: a nationwide questionnaire survey in Japan. Circ Arrhythm Electrophysiol. 2010;3:10–17.
6. Boineau JP, Moore EN, Patterson DF. Relationship between the ECG, ventricular activation, and the ventricular conduction system in ostium primum ASD. Circulation. 1973;48:556–564.
Reiss RE. Fetal distress and monitoring. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adults. 7th ed. Lippincott Williams & Wilkins; 2007.
[Q]8. Murphy JG, Gersh BJ, Mair DD, et al. Long-term outcome in patients undergoing surgical repair of tetralogy of Fallot. N Engl J Med. 1993;329(9):593–599.
9. Khairy P, Harris L, Landzberg MJ, et al. Implantable cardioverter-defibrillators in tetralogy of Fallot.Circulation. 2008;117:363–370.
10. Ayoub EM. Acute rheumatic fever. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adults. 5th ed. Lippincott Williams & Wilkins; 1400–1414.
11. Kleinman CS, Copel JA, Weinstein EM, et al. In utero diagnosis and treatment of fetal supraventricular tachycardia. Semin Perinatol. 1985;9:113–129.
12. Kleinman CS. Prenatal diagnosis and management of intrauterine arrhythmias. Fetal Ther. 1986;1:92–95.
13. Kugler JD, Danford DA, Gumbiner CH. Ventricular fibrillation during transesophageal atrial pacing in an infant with Wolff-Parkinson-White syndrome. Pediatr Cardiol. 1991;12(1):36–38.
14.Benson DW. The normal electrocardiogram. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adults. Lippincott Williams & Wilkins; 152–165.
15. Fish F, Benson W. Disorders of cardiac rhythm and conduction. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adults. Lippincott Williams & Wilkins; 1573.
16. Petrov D, Petrov M. Widening of the QRS complex due to severe hyperkalemia as an acute complication of diabetic ketoacidosis. J Emerg Med. 2008;34:459–461.
17. Fish F, Benson W. Disorders of cardiac rhythm and conduction. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adults. Lippincott Williams & Wilkins; 1585.
18. Hoffman J. Congenital anomalies of the coronary vessels and the aortic root. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adults. 5th ed. Lippincott Williams & Wilkins; 771.
19. Reiss RE. Maternal Diseases and therapies affecting the fetal cardiovascular system. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adults. 5th ed. Lippincott Williams & Wilkins; 549.
20. Fish F, Benson W. Disorders of cardiac rhythm and conduction. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adults. Lippincott Williams & Wilkins; 1593.
21. Gregoratos et al., ACC/AHA/NASPE 2002 Guideline update for implantation of cardiac pacemakers and antiarrhythmia devices. http://www.acc.org/clinical/guidelines/pacemaker/index.htm 2002
22. Jayaprasad N, Francis J. Atrial fibrillation and hyperthyroidism. Indian Pacing Electrophysiol J. 2005;5:305–311.
23. Attenhofer Jost CH, Connolly HM, Danielson GK, et al. Sinus venosus atrial septal defect long-term postoperative outcome for 115 patients. Circulation. 2005;112:1953–1958.
24. Batra AS, Wells WJ, Hinoki KW, et al. Late recovery of atrioventricular conduction after pacemaker implantation for complete heart block associated with surgery for congenital heart disease. J Thorac Cardiovasc Surg. 2003;125(6):1291–1293.
25. Gross GJ, Chiu CC, Hamilton RM, et al. Natural history of postoperative heart block in congenital heart disease: implications for pacing intervention. Heart Rhythm. 2006;3:601–604.
26.Prince KJ, Fish FA. Disorders of cardiac rhythm and conduction. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adults. Lippincott Williams & Wilkins.
27. Laitinen PJ, Brown KM, Piippo K, et al. Mutations of the cardiac ryanodine receptor (RyR2) gene in familial polymorphic ventricular tachycardia. Circulation. 2001;103:485–490.
28.Artman M. Pharmacologic therapy. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adults. 5th ed. Lippincott Williams & Wilkins; 390.
29.Saul JP. Electrophysiologic therapeutic catheterization. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adults. Lippincott Williams & Wilkins.
30. Tzivoni D, Banai S, Schuger C, et al. Treatment of torsade de pointes with magnesium sulfate. Circulation. 1988;77:392–397.
31. Pianosi PT, Driscoll DJ. Exercise testing. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adults. 7th ed. Lippincott Williams & Wilkins.
32. Van Hare GF, Dubin AM. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adults. 7th ed. Lippincott Williams & Wilkins.
33. Fogoros R. Electrophysiologic Testing. 4th ed. Malden, MA: Blackwell Publishers; 2006.
34. www.qtdrugs.org
35. Surawicz B, Knilans TK, Chou T-C. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric. Philadelphia, PA: Saunders; 2001.
36. Olsson SB, Halperin JL. Prevention of stroke in patients with atrial fibrillation. Semin Vasc Med. 2005;5(3):285–292.
37.Deal BJ, Johnsrude CL, Buck SH, eds. Pediatric ECG Interpretation: An Illustrative Guide. Austin, TX: Futura Publishing; 2004.
38. Bricker JT, Porter CJ, Garson A Jr, et al. Exercise testing in children with Wolff-Parkinson-White syndrome. Am J Cardiol. 1985;55:1001–1004.
39.Ellenbogen KA, Wood, MA. Cardiac Pacing and ICDs. 5th ed. Hoboken, NJ: Wiley-Blackwell, 2008.
40. Denfield SW, Rosenthal G, Gajarski RJ, et al. Restrictive cardiomyopathies in childhood. Etiologies and natural history. Tex Heart Inst J. 1997;24(1):38–44.
41. Kishnani PS, Hwu W-L, Mandel H, et al. A retrospective, multinational, multicenter study on the natural history of infantile-onset Pompe disease. J Pediatr. 2006;148:671—676.
42.Hirschhorn R, Arnold JJR. Glycogen storage disease type II: acid alpha-glucosidase (acid maltase) deficiency. In: Scriver C, Beaudet A, Sly W, et al., eds. The Metabolic and Molecular Bases of Inherited Disease. 8th ed. New York, NY: McGraw-Hill; 2001:3389–3420.
43. Haverkamp W, Rolf S, Eckardt L, et al. Long QT syndrome and Brugada syndrome: drugs, ablation or ICD? Herz. 2005;30(2):111–118.
44. Postema PG, Wolpert C, Amin AS, et al. Drugs and Brugada syndrome patients: review of the literature, recommendations, and an up-to-date website (www.brugadadrugs.org. Heart Rhythm. 2009;6(9):1335–1341.
45. Ackerman MJ, Priori SG, Willems S, et al. HRS/EHRA expert consensus statement on the state of genetic testing for the channelopathies and cardiomyopathies this document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA). Heart Rhythm. 2011;8(8):1308–1339.
46. Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation. 2005;111(5):659–670.
47. Pietersen AH, Andersen ED, Sandoe E. Atrial fibrillation in the Wolff-Parkinson-White syndrome. Am J Cardiol. 1992;70:38A–43A.
48. Paul T, Guccione P, Garson A Jr. Relation of syncope in young patients with Wolff-Parkinson-White syndrome to rapid ventricular response during atrial fibrillation. Am J Cardiol. 1990;65:318—321.
49. Epstein AE, DiMarco JP, Ellenbogen KA, et al.; American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices); American Association for Thoracic Surgery; Society of Thoracic Surgeons. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;51(21):e1–62.
50.Walsh EP, Saul JP, Triedman J, eds. Cardiac Arrhythmias in Children and Young Adults with Congenital Heart Disease. Baltimore, MD: Williams & Wilkins; 2001.
51. Lehnart SE, Ackerman MJ, Benson DW Jr, et al. Inherited arrhythmias: a National Heart, Lung, and Blood Institute and Office of Rare Diseases workshop consensus report about the diagnosis, phenotyping, molecular mechanisms, and therapeutic approaches for primary cardiomyopathies of gene mutations affecting ion channel function. Circulation. 2007;116(20):2325–2345.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


