Electrocardiographic Stress Testing
ESSENTIAL FACTS
1. With few exceptions, exercise stress testing is the test of choice for initial evaluation of suspected coronary artery disease (CAD).
2. Diagnosis of CAD using exercise stress testing is limited by verification bias and an uncertain “gold standard.”
3. Exercise capacity is the most important prognostic factor derived from exercise stress testing; Duke treadmill score (DTS), heart rate recovery (HRR), chronotropic response, and ventricular ectopy during recovery also provide important prognostic information.
4. Exercise stress testing is most useful for intermediate-risk patients.
ESSENTIAL EVIDENCE/CURRENT GUIDELINES
The exercise electrocardiographic (ECG) stress test is one of the most commonly performed diagnostic tests in modern medicine and is the test of choice for the initial evaluation of suspected CAD. Its advantages include its low cost, general safety, noninvasive nature, and its usefulness in providing information regarding functional capacity. With the wide proliferation of imaging techniques, the “plain old treadmill test” has become increasingly underappreciated, despite its ability to predict short- and long-term risks. In fact, if a patient is able to exercise, has not been previously revascularized, and has a baseline ECG that is considered interpretable, ECG stress testing is the test of choice for the evaluation of suspected CAD.
Traditionally, the primary goal of exercise stress testing is the diagnosis of obstructive CAD and myocardial ischemia in patients with symptoms of angina or risk factors for heart disease. This goal, however, is hampered by verification bias; because the majority of patients who undergo coronary angiography to confirm the diagnosis of CAD have had a positive stress test, it cannot be known for certain how sensitive or specific the stress test is—those who had a negative stress test are not evaluated similarly with angiography. Furthermore, the use of coronary angiography as the gold standard for the diagnosis of CAD is increasingly questioned, as more recent studies have suggested that, because of arterial remodeling, an angiographically normal-appearing artery can actually have a significant amount of atherosclerotic disease upon evaluation by other methods such as intravascular ultrasound. For these reasons, some cardiologists discourage the notion of exercise stress testing as a “diagnostic” tool, but instead consider it a “prognostic” tool.
Safety
Exercise treadmill testing is generally considered to be very safe, but can rarely be associated with serious complications. These may include myocardial infarction (3.5/10,000 tests), serious arrhythmias (4.8/10,000), and death (0.5/10,000). Exercise testing after myocardial infarction is also safe at as early as 3 to 5 days, though is usually limited to submaximal testing using endpoints of 70% age-predicted maximal heart rate (rather than the 85% on a standard exercise stress test) or a peak work level of 5 METs.
Indications and Contraindications to Exercise ECG Stress Testing
Most commonly, exercise stress testing is ordered for the diagnosis of obstructive or flow-limiting CAD; it is most useful in patients with an intermediate pretest probability based on age, gender, and description of chest pain. In a patient with a high pretest probability of CAD (e.g., a middle-aged male with typical anginal symptoms and multiple cardiac risk factors), a negative stress test does not sufficiently preclude a diagnosis of CAD and is more likely to be a false negative result. In contrast, in a patient with a low pretest probability of CAD (e.g., a young woman with atypical symptoms and no significant risk factors), a positive stress test is more likely to be a false positive result. The sensitivity and specificity of testing is therefore highest in patients with intermediate pretest probability. Patients must also have a baseline ECG in which ST segments and subsequent changes are interpretable.
Patients with left bundle branch block, paced rhythms, >1 mm of resting ST depression (e.g., digoxin therapy or left ventricular hypertrophy with strain pattern), and Wolff–Parkinson–White syndrome are therefore not recommended for exercise ECG testing without adjunctive imaging due to the difficulty in assessing ECG changes in these patients. In patients with underlying left bundle branch block on ECG, pharmacologic stress is preferred over exercise stress due to the risk of diagnosing false positive septal ischemia.
Stress testing can also be used to assess prognosis in patients with known or suspected CAD. It is recommended after myocardial infarction for activity or exercise prescription, entrance into cardiac rehabilitation, and evaluation of medical therapy: and after revascularization to evaluate symptoms and as periodic monitoring of high-risk, asymptomatic patients. In patients with valvular heart disease, stress testing is used for evaluation of exercise capacity and may be very useful in determining the appropriate timing of surgery. Use of stress testing is also indicated for adjustment of pacemaker settings, assessment of suspected exercise induced arrhythmias, and evaluation of therapy in patients with suspected exercise-induced arrhythmias. Before a patient returns to work, testing may provide a comparison of peak workload achieved to that required in employment.
There are no class I indications for testing of asymptomatic patients, and routine screening is classified as a class III indication. However, patients who are asymptomatic but have multiple risk factors, those planning to start vigorous exercise or are engaged in occupations that may affect public safety (e.g., pilots, bus drivers), and those who are at high risk of cardiovascular disease because of comorbidities such as diabetes mellitus can still be referred for exercise stress testing though these are listed as class II indications (see Table 10.1 for class I indications for exercise stress testing).
TABLE
10.1 Class I Indications for Exercise Stress Testing
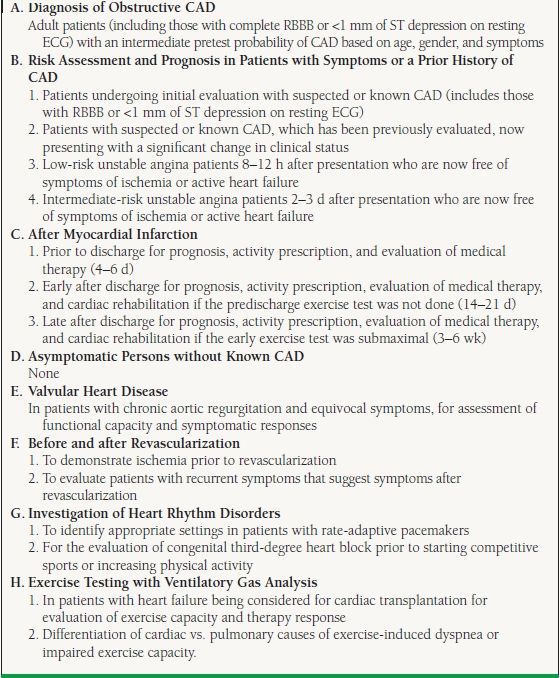
Adapted from Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation. 2002;106:1883–1892.
Contraindications to exercise stress testing (Table 10.2) include testing of extremely low-risk patients and those with recent myocardial infarction (within 2 days), unstable angina or dynamic ECG changes, active or unstable arrhythmias or congestive heart failure, aortic dissection, severe aortic stenosis, or other acute cardiac or systemic processes. Relative contraindications are at the discretion of the physician: testing may proceed if the benefit outweighs the risk.
TABLE
10.2 Contraindications to Exercise Testing
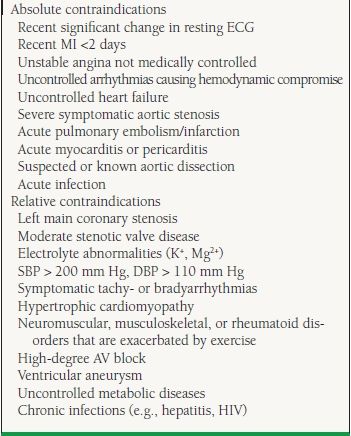
MI, myocardial infarction; SBP, systolic blood pressure; DBP, diastolic blood pressure; AV, atrioventricular.
(Adapted from Gibbons RJ, Balady GJ, Beasley JW, et al. ACC/AHA guidelines for exercise testing: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). Circulation. 1997;96:345–354.)
Methods of Testing
Ideally, the exercise stress test should last 8 to 12 minutes; this provides a reasonable compromise for assessment of functional capacity without fatigue and attainment of anaerobic threshold. It is therefore important to choose the appropriate exercise protocol to suit the patient’s projected ability to perform the test. For instance, the widely used Bruce protocol may be an appropriate test for most patients, but is likely too difficult for an elderly patient undergoing risk stratification before hospital discharge. A truncated test provides a less accurate assessment of functional capacity.
Although bicycle protocols allow for a more precise measurement of work capacity, most patients in the United States have more familiarity with treadmill methods and treadmill is therefore more commonly used. The disadvantage of treadmill is that work is only estimated and tends to be overestimated, depending on the degree of reliance (leaning) on handrails.
Placement of electrodes for ECG measurement differs in exercise testing compared to standard 12-lead ECG and may result in rightward axis shift and false positive or negative inferior Q waves. Lead V5 is often the best for assessment of ST changes. ECGs are obtained at rest, during each stage of exercise, at peak exercise, and every 1 to 2 minutes for at least 5 minutes of recovery. Other data obtained during testing include cardiac rhythm, heart rate, blood pressure, symptoms, and the patient’s rating of perceived exertion. The test is completed when the patient attains 85% of the age-predicted maximum heart rate or cannot proceed because of symptoms. The age-predicted maximum heart rate is calculated as 220 minus the age in years.
Absolute indications for termination of stress testing (Table 10.3) include symptoms, drop in systolic blood pressure, sustained ventricular arrhythmias, and the development of ST elevation in leads without q waves. Relative indications for termination of testing are also listed.
TABLE
10.3 Indications for Termination of ECG Stress Testing
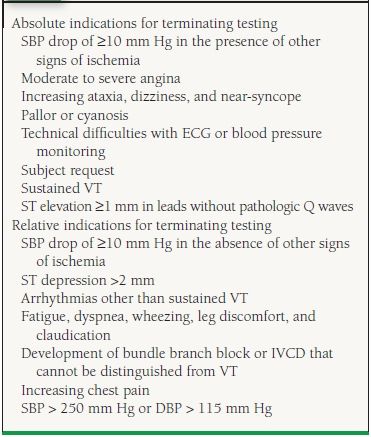
SBP, systolic blood pressure; VT, ventricular tachycardia; IVCD, intraventricular conduction defect; DBP, diastolic blood pressure.
(Adapted from Gibbons RJ, Balady GJ, Beasley JW, et al. ACC/AHA guidelines for exercise testing: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). Circulation. 1997;96:345–354.)
Diagnostic Interpretation
Interpretation of the ECG stress test primarily involves evaluation of the ST segment. The classic positive finding is ≥1 mm of horizontal or down-sloping ST-segment depression 80 ms after the J point, though many labs also consider up-sloping ST-segment depression ≥1.5 mm a positive finding. Ischemic changes tend to occur in leads I and V4-V6; the more widespread the ECG changes, usually the more severe the disease. ST-segment depression does not localize ischemia; however, ST-segment elevation in leads without Q waves does localize the distribution of ischemia and is an absolute indication for termination of the test. Markers of severe CAD during testing include a drop in systolic blood pressure below resting value, exercise-limiting angina, poor exercise capacity <5 METs, down-sloping ST depression in recovery, and ST depression at low work load.
Prognostic Interpretation
Of as much importance as evaluation of ST segments during stress testing is the contribution of other markers of risk to overall prognosis. Exercise capacity is the most important prognostic variable; it is widely accepted that patients able to perform >10 METs are in general at low risk for cardiovascular events (Table 10.4). The heart rate recovery (HRR), the difference in heart rate from peak exercise to 1 minute recovery, is known to be a very strong prognostic indicator. HRR of 12 beats or less predicts an increased relative risk of sudden cardiac death and all cause mortality independent of CAD severity. Normally, withdrawal of the sympathetic nervous system and reactivation of the parasympathetic nervous system lead to a drop in heart rate after exercise, that is, HRR > 12 beats. A reduction in vagal activity, which may be the mechanism of a low HRR, has been previously shown to have an adverse effect on mortality and may be the reason a poor HRR predicts mortality.
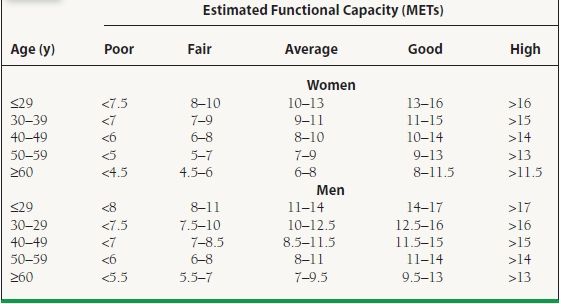
TABLE
10.4 Age and Gender Estimated Functional Capacity