Chapter 3
Electrocardiogram
1. What are the most commonly used criteria to diagnose left ventricular hypertrophy (LVH)?
2. What are the most commonly used criteria to diagnose right ventricular hypertrophy (RVH)?
3. What criteria are used to diagnose left atrial enlargement (LAE)?
 P wave total width of > 0.12 sec (3 small boxes) in the inferior leads, usually with a double-peaked P wave
P wave total width of > 0.12 sec (3 small boxes) in the inferior leads, usually with a double-peaked P wave
 Terminal portion of the P wave in lead V1 ≥ 0.04 sec (1 small box) wide and ≥ 1 mm (1 small box) deep
Terminal portion of the P wave in lead V1 ≥ 0.04 sec (1 small box) wide and ≥ 1 mm (1 small box) deep
4. What electrocardiogram (ECG) finding suggests right atrial enlargement (RAE)?
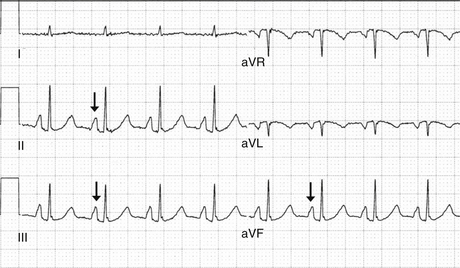
 P-wave height in the inferior leads (II, III, and aVF) ≥ 2.5 to 3 mm (2.5 to 3 small boxes) (Fig. 3-1)
P-wave height in the inferior leads (II, III, and aVF) ≥ 2.5 to 3 mm (2.5 to 3 small boxes) (Fig. 3-1)
5. What is the normal rate of a junctional rhythm?
6. How can one distinguish a junctional escape rhythm from a ventricular escape rhythm in a patient with complete heart block?
7. Describe the three types of heart block.
 First-degree heart block: The PR interval is a fixed duration of more than 0.20 seconds.
First-degree heart block: The PR interval is a fixed duration of more than 0.20 seconds.
 Second-degree heart block: In Mobitz type I (Wenckebach) block, the PR interval increases until a P wave is nonconducted (Fig. 3-2). The cycle then resets and starts again. Mobitz type I second-degree heart block is sometimes due to increased vagal tone and is usually a relatively benign finding. In Mobitz type II block, the PR interval is fixed and occasional P waves are nonconducted. Mobitz type II second-degree heart block usually indicates structural disease in the atrioventricular (AV) node or His-Purkinje system and is an indication for pacemaker implantation.
Second-degree heart block: In Mobitz type I (Wenckebach) block, the PR interval increases until a P wave is nonconducted (Fig. 3-2). The cycle then resets and starts again. Mobitz type I second-degree heart block is sometimes due to increased vagal tone and is usually a relatively benign finding. In Mobitz type II block, the PR interval is fixed and occasional P waves are nonconducted. Mobitz type II second-degree heart block usually indicates structural disease in the atrioventricular (AV) node or His-Purkinje system and is an indication for pacemaker implantation.
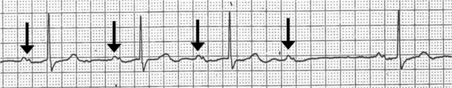
Figure 3-2 Wenckebach block (Mobitz type I second-degree AV block). The PR interval progressively increases until there is a nonconducted P wave.
 Third-degree heart block: All P waves are nonconducted, and there is either a junctional or ventricular escape rhythm. To call a rhythm third-degree or complete heart block, the atrial rate (as evidenced by the P waves) should be faster than the ventricular escape rate (the QRS complexes). Third-degree heart block is almost always an indication for a permanent pacemaker.
Third-degree heart block: All P waves are nonconducted, and there is either a junctional or ventricular escape rhythm. To call a rhythm third-degree or complete heart block, the atrial rate (as evidenced by the P waves) should be faster than the ventricular escape rate (the QRS complexes). Third-degree heart block is almost always an indication for a permanent pacemaker.
8. What are the causes of ST segment elevation?
 Acute myocardial infarction (MI) due to thrombotic occlusion of a coronary artery
Acute myocardial infarction (MI) due to thrombotic occlusion of a coronary artery
 Prinzmetal angina (variant angina), in which there is vasospasm of a coronary artery
Prinzmetal angina (variant angina), in which there is vasospasm of a coronary artery
 Cocaine-induced MI, in which there is vasospasm of a coronary artery, with or without additional thrombotic occlusion
Cocaine-induced MI, in which there is vasospasm of a coronary artery, with or without additional thrombotic occlusion
 Pericarditis, in which there is usually diffuse ST segment elevation
Pericarditis, in which there is usually diffuse ST segment elevation
 Left bundle branch block (LBBB)
Left bundle branch block (LBBB)
 Left ventricular hypertrophy with repolarization abnormalities
Left ventricular hypertrophy with repolarization abnormalities
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree