Chapter 4 Electrical Therapy
Upon completion of this chapter, you will be able to:
Defibrillation
Energy, Voltage, and Current
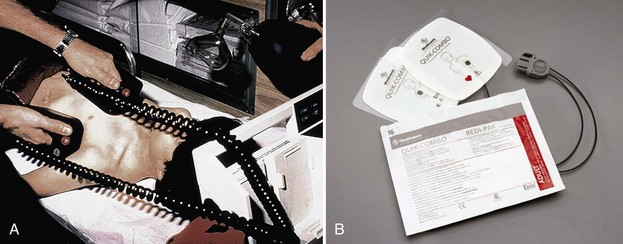
A defibrillator is a device used to deliver a shock to eliminate an abnormal heart rhythm (Figure 4-1). It consists of:
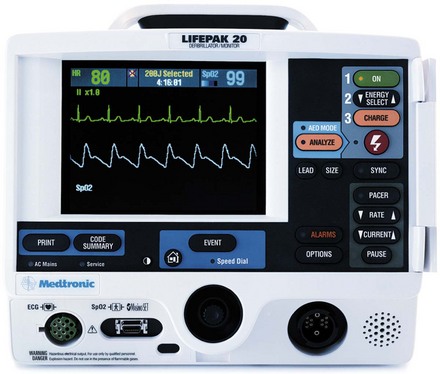
Figure 4-1 A defibrillator is used to deliver an electrical shock to terminate an abnormal heart rhythm.
Monophasic Versus Biphasic Defibrillation
[Objective 1]
There are three general types or classes of defibrillation waveforms: monophasic, biphasic, and triphasic.1 Waveforms are classified by whether the current flow delivered is in one direction, two directions, or multiple directions.
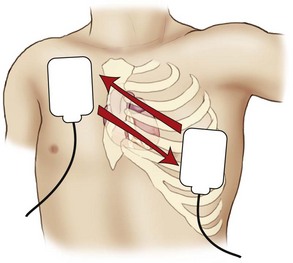
When a monophasic waveform is used, current passes through the heart in one (i.e., mono) direction (Figure 4-3). Although few monophasic waveform defibrillators are manufactured today, many are still in use. With biphasic waveforms, energy is delivered in two (i.e., bi) phases. The current moves in one direction for a specified period, stops, and then passes through the heart a second time in the opposite direction during a very short period (i.e., milliseconds) (Figure 4-4).
Most AEDs and manual defibrillators sold today make use of biphasic waveform technology. Biphasic defibrillators use either a biphasic truncated exponential (BTE) waveform or a rectilinear biphasic waveform (RBW) (Figure 4-5). The BTE waveform has been used in implantable defibrillator-cardioverters (ICDs) for many years; it was approved for use by the U.S. Food and Drug Administration in 1996 as part of the Heartstream AED, which is now a part of Philips Medical Systems (Seattle, WA). In 1999, Zoll Medical Corporation (Burlington, Mass) announced the development of RBW technology, which was subsequently approved for clinical use by the U.S. Food and Drug Administration.
Transthoracic Impedance
Body Tissue and Hair
The skin surface, fat, bone, and hair can cause significant increases in resistance. It may be difficult to ensure good electrode-to-skin contact in a patient who has a hairy chest. However, if good contact is not ensured, transthoracic impedance will be high and the effectiveness of defibrillation will be reduced.3 There is an increased risk of burns from arcing (i.e., sparks) from electrode to skin and from electrode to electrode; ECG identification and analysis may also be inhibited.
Paddle or Pad Size
Studies have shown that adult paddles or pads should be used for patients weighing more than 10 kg (22 lb) (i.e., generally older than 1 year).4–7 For adults, the paddle or pad size ranges from 8 to 12 cm in diameter. Use pediatric paddles or pads for infants and children weighing less than 10 kg (22 lb) or for those whose chests are too small to accommodate standard paddles or pads.8 Generally, use the largest pads that will fit the patient’s chest with at least 1 inch (3 cm) separating the pads. Avoid using pediatric electrodes for adult defibrillation because myocardial injury can occur.9
When applying defibrillation paddles or pads, remove the patient’s clothing and expose his or her chest. Be sure to look for transdermal patches or disks, which may be used to deliver nitroglycerin, nicotine, analgesics, hormones, or antihypertensives. Do not apply paddles or pads directly over the medication patch or disk because the patch may prevent good electrode contact, hindering the delivery of energy from the defibrillation electrode to the heart. A lack of good contact can cause arcing and may cause skin burns.10 If a medication patch, disk, or ointment is located at or near the site of paddle or pad placement, remove it and wipe the area clean (do not use alcohol or alcohol-based cleansers) before applying defibrillation paddles or pads.11
Paddle or Pad Position
[Objective 1]
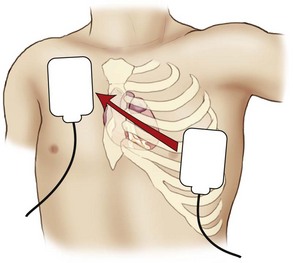
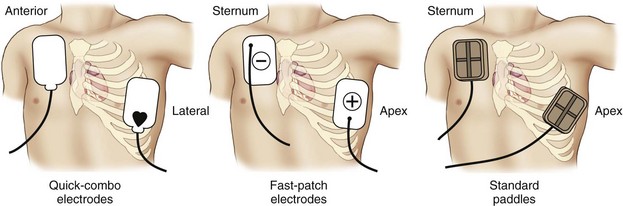
When preparing the skin for paddle or pad placement, do not use alcohol, tincture of benzoin, or antiperspirant. Hand-held paddles or combination pads should be placed on the patient’s bare chest according to the manufacturer’s instructions. Paddles or pads may be labeled according to their intended position on the chest (e.g., sternum/apex, front/back) or according to their polarity (e.g., positive, negative). Studies have shown that the anterolateral, anteroposterior, anterior-left infrascapular, and anterior-right infrascapular paddle/pad positions are equally effective to treat atrial or ventricular dysrhythmias.13
The typical paddle or pad position used during resuscitation is the sternum-apex position, also called the anterolateral or apex-anterior position. This position is often used because the anterior chest is usually easy to get to and placement of the paddles or pads in this position approximates ECG electrode positioning in lead II. Place the sternum paddle or pad lateral to the right side of the patient’s sternum, just below the clavicle. Place the center of the left (apex) paddle or pad in the midaxillary line, lateral to the patient’s left nipple (Figure 4-6). If the patient is a woman, elevate the left breast and place the apex paddle or pad lateral to or underneath the breast. Placing defibrillation paddles or pads directly on breast tissue results in higher transthoracic impedance, reducing current flow.14
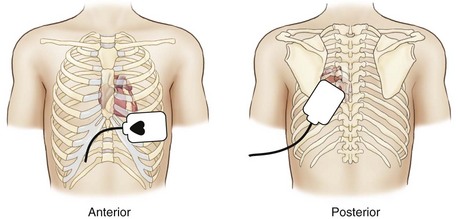
Another common position used for paddle or pad placement is the anterior-posterior position. In this position, one paddle or pad is placed over the patient’s left chest with the upper edge of the pad below the nipple. The other is placed on the back, just below the patient’s left scapula (Figure 4-7). Alternative positions may be considered based on individual patient characteristics.13
Keeping It Simple
In resuscitation situations, precious seconds can be lost when rescuers try to make sure that the “sternum” pad is placed on the sternum and the “apex” pad is placed over the apex of the heart. Delays sometimes occur when rescuers realize that paddles or pads have been placed in reversed positions and then attempt to reposition them to their “proper” location. Reversal of the position of the electrodes is not important during defibrillation, provided the heart is located between them.15
Use of Conductive Material
When applying adhesive pads to the patient’s chest, press from one edge of the pad across the entire surface to remove all air and avoid the development of air pockets (Figure 4-8). A hands-free defibrillation cable is used to attach the pads to the monitor/defibrillator.
When using pregelled pads with hand-held paddles, make sure the pads cover the entire paddle surface to avoid arcing current and potential burns. Do not use saline-soaked gauze or alcohol-soaked pads for defibrillation. Excess saline on the chest may cause arcing and burns. Alcohol-soaked pads may ignite. Do not use gels or pastes (e.g., ultrasound gel) that are not specifically made for defibrillation. The use of improper pastes, creams, gels, or pads can cause burns or sparks and may pose a risk of fire in an oxygen-enriched environment.16 If too much gel is used, the material may spread across the chest wall during resuscitation. This can lead to arcing of the current from one paddle to another and away from the heart, and this can also produce a potentially dangerous spark or burns.
Defibrillation Procedure
[Objective 1]
Be sure that the cardiopulmonary resuscitation (CPR) team member continues chest compressions as the defibrillator is readied for use (Figure 4-9). The airway team member should coordinate ventilations with the CPR team member until an advanced airway is placed and its position confirmed.
Turn the power to the monitor/defibrillator on and verify the presence of a shockable rhythm on the monitor. Select an appropriate energy level. Use 360 J for all shocks if a monophasic defibrillator is used.13,17 Use the energy levels recommended by the manufacturer for the initial and subsequent shocks if a biphasic defibrillator is used (i.e., 120 to 200 J). If you do not know what the recommended energy levels are, consider defibrillation at the maximal dose.13,17
While the defibrillator is readied, instruct the IV/medication team member to prepare the initial drugs that will be used and start an IV after the first shock is delivered. If hand-held paddles are used, instruct the defibrillation team member to place the paddles in their proper positions on the patient’s chest. Be sure that firm downward pressure (about 25 lb) is applied to each paddle. Do not lean on the paddles because they may slip! Charge the defibrillator. If hand-held paddles are used, press the “Charge” button on the machine or the button located on the apex paddle. If combination pads are used, press the “Charge” button on the machine (Figure 4-10).
If a shockable rhythm is still present, call “Clear!” Look around you (360 degrees) to be sure everyone—including you—is clear of the patient, the bed, and any equipment connected to the patient (Figure 4-11). Be sure oxygen is not flowing over the patient’s chest. Press the “SHOCK” control to discharge energy to the patient. Release the shock control after the shock has been delivered. Instruct the team to resume chest compressions immediately without pausing for a rhythm or pulse check. Instruct the airway team member to turn on the oxygen and coordinate ventilations with the chest compressor. Instruct the IV/medications team member to establish vascular access and give the patient a vasopressor during CPR. Remember that interruptions in chest compressions must be kept to a minimum throughout the resuscitation effort. Continue CPR for about 2 minutes. After five cycles of CPR (about 2 minutes), recheck the rhythm. If a shockable rhythm is present, charge the defibrillator to a higher dose and then call “Clear!” Check to be certain that everyone is clear and then defibrillate. Resume CPR immediately. While continuing CPR, instruct the IV/medications team member to give an antiarrhythmic (amiodarone or lidocaine if amiodarone is not available). Consider placement of an advanced airway. Use the memory aids PATCH-4-MD or the 5 H’s and 5 T’s to help identify possible reversible causes of the arrest or factors that may be complicating the resuscitation effort. After 2 minutes of CPR, repeat the sequence, beginning with a rhythm check.
If defibrillation restores an organized rhythm, check for a pulse. If a pulse is present, check the patient’s blood pressure and other vital signs and begin post–cardiac arrest care. If you are not sure if a pulse is present, resume CPR.17 If defibrillation successfully terminates pulseless VT/VF but the rhythm recurs, begin defibrillation at the last energy level used that resulted in successful defibrillation. If a rhythm check reveals a nonshockable rhythm, resume CPR, consider possible causes of the arrest, and give medications and other emergency care as indicated. Continue CPR for 2 minutes before performing another rhythm check.
You Should Know
What If …?
What energy should be used if you deliver a shock that eliminates pulseless VT/VF and then the rhythm recurs? If defibrillation terminates pulseless VT/VF that then recurs, defibrillate at the last successful energy setting.17
What if the patient has a permanent pacemaker or an ICD? An ICD is typically placed subcutaneously in the left upper quadrant of the patient’s abdomen or the left pectoral area (Figure 4-12). It can deliver a range of therapies (also called tiered-therapy) including defibrillation, antitachycardia (i.e., “overdrive”) pacing, synchronized cardioversion, and bradycardia pacing, depending on the dysrhythmia detected and how the device is programmed (Figure 4-13). A physician determines the appropriate therapies for each patient. Depending on the manufacturer, the ICD may deliver a maximum of six shocks for VF. About 2 J are delivered at the body surface when the ICD discharges internally. Rescuers in contact with the patient may feel a tingling sensation when the ICD delivers a shock. Although the energy is enough to be felt by the rescuer, it is not enough to cause physiologic harm. If the ICD is delivering shocks, wait 30 to 60 seconds for the ICD to complete the treatment cycle before attaching an AED. When defibrillating or cardioverting a patient with a permanent (implanted) pacemaker or an ICD, be careful to not place the defibrillator paddles or combination pads directly over the device. The anterior-posterior and anterolateral paddle or pad positions are considered acceptable in these patients.13 Although placement of paddles or pads should not delay defibrillation, defibrillator paddles or combination pads should ideally be placed at least 3 inches (8 cm) from the pulse generator (there will be a bulge under the patient’s skin).13 Because some of the defibrillation current flows down the pacemaker leads, a patient who has a permanent pacemaker or ICD should have the device checked to ensure proper function after defibrillation.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree