Electrical Therapy
 Just the facts
Just the factsIn this chapter, you’ll learn:
♦ the procedure for defibrillation
♦ the procedure for cardioversion
♦ techniques for inserting pacemakers
♦ techniques for evaluating pacemaker function.
Defibrillation
Defibrillation is used to deliver a large amount of electric current to a patient over a brief period of time. It’s the standard treatment for ventricular fibrillation (VF) and pulseless ventricular tachycardia (VT).
A defibrillation shock aims to temporarily depolarize the heart when the rhythm is chaotic. It does so by completely depolarizing the myocardium, producing a momentary asystole. This provides an opportunity for the heart’s natural pacemaker centers to restore a normal rhythm.
CPR before and after is better
According to the 2010 American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care, the foundation of successful advanced cardiac life support (ACLS) is high-quality cardiopulmonary resuscitation (CPR) and, for VF or pulseless VT, attempted defibrillation within moments of arrest. For monitored hospital patients, the time from VF to defibrillation should be less than 3 minutes and CPR should be performed while the defibrillator is readied. This is because effective chest compressions help deliver blood to the coronary arteries and brain.
Key points
Defibrillation
Delivery of electric shocks to depolarize irregular heartbeat and allow coordinated conteractile activity to resume
Treatment for ven-tricular fibrillation and unstable tachycardia
Early defibrillation most effective
It’s also important to perform CPR immediately after defibrillation because the patient may experience a period of asystole or pulseless electrical activity, which CPR may help convert to a perfusing rhythm. However, basic CPR can’t convert VF to a normal rhythm. The only way to end VF and restore normal rhythm is electrical defibrillation.
A real need for speed
Defibrillation is significantly more effective when VF is recognized and treated quickly. When defibrillation is performed within the first 5 minutes of cardiac arrest, the survival rate is 50%. This survival rate decreases by 7% to 10% for each minute that the patient is in VF.
When performing defibrillation, you can use either an automated external defibrillator (AED) or a conventional defibrillator.
|
Automated external defibrillators
The AED is a portable defibrillator with a microcomputer that senses and analyzes a patient’s heart rhythm and then gives you step-by-step directions on how to proceed if defibrillation is indicated.
Form and function
All AED models have the same basic functions but offer different operating options. For example, all AEDs communicate directions by displaying messages on a screen, giving voice commands, or both. Some AEDs simultaneously display a patient’s heart rhythm. All devices record your interactions with the patient during defibrillation and some may have an integral printer for immediate event documentation.
Two types of AEDs currently exist:
the fully automated AED, which delivers a shock if VF is present
the semiautomatic AED, which requires you to press an ANALYZE control to start the rhythm analysis; it then audibly or visually prompts you to press a SHOCK control to deliver a shock if warranted. (See Understanding AEDs.)
With either device, the electrical shock is delivered through two adhesive electrode pads applied to the patient (upperright sternal border, lower-left ribs over the cardiac apex). The adhesive pads have two functions: to transmit the patient’s rhythm and to deliver the shock.
|
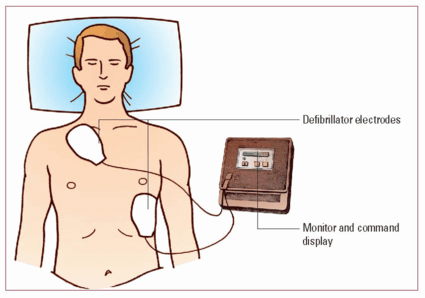
Understanding AEDs
Automated external defibrillators (AEDs) vary with the manufacturer but the basic components for each device are similar. This illustration shows a typical AED and proper electrode placement.
|
How it’s done
For a person who has collapsed and is unconscious, initiate CPR immediately and use an AED as soon as it’s available. Perform five cycles (2 minutes) of CPR before checking the electrocardiogram (ECG) rhythm and attempting defibrillation.
To perform defibrillation with an AED:
Open the packets containing the two electrode pads.
Expose the patient’s chest.
Remove the plastic backing film from the electrode pads. Follow the manufacturer’s instructions for pad placement and connection to the cable. (The correct pad placement is usually illustrated on the pads.)
Press the ON button and wait while the machine performs a self-test. (Most AEDs signal their readiness by a computerized voice that says, “Stand clear” or by emitting a series of loud beeps. When that occurs, the machine is ready to analyze the patient’s heart rhythm.)
Ask all personnel to stand clear, then press the ANALYZE button when the machine prompts; don’t touch or move the patient while the AED is in analysis mode. Analysis takes 5 to 15 seconds, depending on the machine. (See How AEDs sense rhythm.)
If a shock isn’t needed, the AED will display or say “No shock indicated” and then prompt you to immediately resume CPR starting with chest compressions. If the patient needs a shock, the AED will announce a “stand clear” message and emit a beep that changes to a steady tone as it charges.
When the AED is fully charged and ready to deliver a shock, it will prompt you to press the SHOCK button.
Make sure no one is touching the patient or bed and call out “Stand clear.” Then press the SHOCK button on the AED.
After you deliver the first shock, immediately resume CPR, performing five cycles (about 2 minutes).
Key points
Automated external defibrillators
Contain cardiac rhythm analysis systems
May be fully or semiautomated
For patients with no pulse and no respirations
Less training needed to operate
Faster speed of operation and delivery
Hands-free-technique
Energy level = 200 to 360 joules
How AEDs sense rhythm
The accuracy of the automated external defibrillator (AED) in rhythm analysis is considered very high. A microprocessor analyzes features of the patient’s electrocardiogram signal for frequency, amplitude, and integration of frequency and amplitude. A safety filter checks for false signals, such as those deriving from radio transmissions, poor electrode contact, 60-cycle interference, or loose electrodes.
Multiple analyses
In addition, the AED takes multiple looks—each lasting a few seconds—at the rhythm being analyzed. Several analyses must confirm the presence of a shockable rhythm, and other checks must be consistent with a nonperfusing cardiac status. The fully automated AED will then charge and deliver a shock; the semiautomatic AED will signal the operator that a shock is advised.
|
Data entry
The AED should then analyze the rhythm and prompt you to deliver another shock if needed. When the patient is stable, remove the computer memory module or tape from the AED and transcribe it, or prompt the AED to print a rhythm strip with code data.
What to consider
The patient can’t be touched while the AED analyzes the rhythm, charges its capacitors, and delivers the shock.
You must stop chest compressions and ventilations while the device is operating.
You’ll need to modify your actions for patients with implanted pacemakers, implantable cardioverter-defibrillators, transdermal medication patches, and for those being resuscitated around water. (See Safety tips for defibrillation.)
Safety tips for defibrillation
You must take precautions when defibrillating a patient with an implantable cardioverter-defibrillator (ICD) or pacemaker or for a patient who’s wearing a transdermal medication patch. You must also be careful when defibrillating a patient who’s in contact with water.
Defibrillating a patient with an ICD or pacemaker
Avoid placing the defibrillator paddles or pads directly over the implanted device. Place them at least 1” (2.5 cm) away from the device.
Defibrillating a patient with a transdermal medication patch
Avoid placing electrodes directly on top of a transdermal medication patch, such as nitroglycerin, nicotine, analgesics, or hormone replacements. The patch can block delivery of energy and cause a small burn to the skin. Remove the medication patch and quickly wipe the area clean before defibrillation.
Defibrillating a patient near water
Water is a conductor of electricity and may provide a pathway for energy from the defibrillator to the rescuers treating the patient. Remove the patient from free-standing water and quickly dry his chest before defibrillation.
Conventional defibrillators
The conventional defibrillator is commonly used in most health care facilities. Unlike an AED, it requires you to analyze the rhythm, select the energy level to be administered, apply the paddles or “hands off” pads to the patient’s chest, and discharge the current by pressing both paddle buttons simultaneously or by pressing the SHOCK button on the defibrillator.
|
Two types of conventional defibrillators exist: monophasic and biphasic. (See Monophasic and biphasic defibrillators, page 106.)
How it’s done
For a quick look at the patient’s cardiac rhythm, place the paddles on the patient’s chest while you have someone place the defibrillator’s monitoring leads and defibrillator pads on the patient. Assess the patient and the rhythm on the defibrillator monitor. If the patient is in VF or pulseless VT, defibrillation is appropriate.
Monophasic and biphasic defibrillators
Two types of defibrillators are available: monophasic and biphasic.
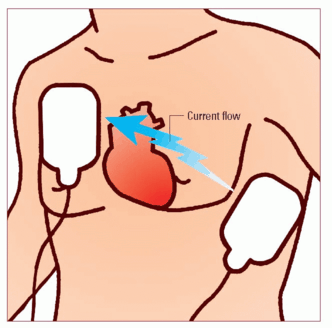
Monophasic defibrillators
Monophasic defibrillators deliver a single current of electricity that travels in one direction between the two pads or paddles on the patient’s chest. To be effective, a large amount of electrical current is required for monophasic defibrillation.
|
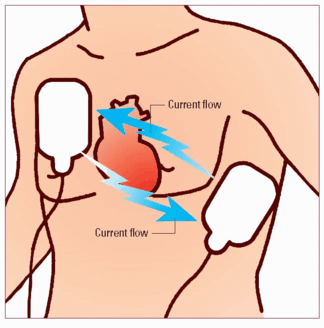
Biphasic defibrillators
For biphasic defibrillators, pad or paddle placement is the same; however, the discharged electrical current travels in a positive direction for a specified duration and then reverses and flows in a negative direction for the remaining time of the electrical discharge, thereby delivering two currents of electricity. Using two currents lowers the defibrillation threshold of the heart muscle, increasing the likelihood for successful defibrillation of ventricular fibrillation with smaller amounts of energy. Biphasic defibrillators also adjust for differences in impedance or resistance, which reduces the number of shocks needed. Most newer defibrillators are biphasic.
|
Conventional wisdom
To perform defibrillation with a conventional defibrillator:
Expose the patient’s chest.
Apply conductive material—gel to the paddles or conduction pads to the chest wall. You can also use remote defibrillation “hands-off” pads, which connect directly to the defibrillator.
– For anterolateral pad placement: Place one pad to the right of the upper sternum, just below the right clavicle, and the other over the fifth or sixth intercostal space at the left anterior axillary line.
– For anteroposterior pad placement: Place the anterior pad directly over the heart at the precordium to the left of the lower sternal border; place the posterior pad under the patient’s body beneath the heart and immediately below the scapula.
Turn on the defibrillator.
Set the monophasic defibrillator energy level to 360 joules, or set the biphasic energy level, following manufacturer and facility recommendations, to 120 to 200 joules for an adult patient. If you don’t know which type of defibrillator you’re using, set the energy level to 200 joules.
Place the paddles over the conductive pads and press firmly against the patient’s chest using 25 lb of pressure. If you’re using gel, place the paddles in the appropriate positions; if you’re using the “hands off” pads, don’t touch the paddles.
Charge the defibrillator by pressing the CHARGE buttons, located either on the machine or on the paddles themselves. If you’re using remote defibrillator pads, press the CHARGE button on the machine.
When the machine is fully charged, instruct everyone to stand clear of the patient and the bed. Also, instruct someone to turn off any oxygen flow.
Discharge the current by simultaneously pressing the CHARGE buttons on both paddles. If you’re using remote defibrillator pads, press the DISCHARGE or SHOCK button on the machine.
|
After the first shock is delivered, immediately resume CPR, beginning with chest compressions, performing five cycles (about 2 minutes). Reassess the patient’s cardiac rhythm on the monitor and, if necessary, prepare to defibrillate a second time if appropriate.
Restoration station
If defibrillation restores cardiac rhythm and return of spontaneous circulation:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree