Fig. 4.1
The EKG complex: individual components are identified here and will be discussed in the main text
EKG Findings in Acute Pericarditis
The pericardium is a fibrous sac that is composed of both a visceral and parietal layer that surrounds the heart and extends onto the proximal great vessels. When inflamed, be it as part of an infectious, inflammatory or oncologic process, pericarditis is present. At times, the underlying myocardium may be involved as well and this leads to a condition termed myopericarditis. This inflammatory process causes changes in the tissue of the pericardium and, when involved, the myocardium. Additionally, it may increase the amount of fluid present in the pericardial space.
Low Voltage EKG Signal

One of the hallmarks of acute pericarditis is the pericardial effusion. While it may be of varying size and hemodynamic significance, the short-circuiting effect of this effusion, as well as the electrically insulating properties of the contained fibrin are thought by many to result in low voltage recordings on the EKG. Others suggest that the low voltage seen in pericarditis is specifically a marker of cardiac tamponade [3]. Electrocardiographically, low voltage is defined as an amplitude of less than 0.5 mv (or 5 mm) on the limb leads and less than 1 mv on the precordial leads (10 mm) [4]. Anatomically, there is a larger amount of space available for fluid to collect around the anterior heart structures, as the pericardial reflections behind the atria limit the posterior potential space. This results in a low amplitude QRS complexes, while the P wave amplitude will be spared in the limb leads due to the relative paucity of fluid around the posterior atria.
While the finding of low voltage occurs in many patients with pericardial disease, it is neither a sensitive nor a specific finding and occurs in any condition in which the amplitude of the ventricular signal is decreased. The differential diagnosis of low voltage therefore includes systemic conditions including myxedematous involvement of myocardium as seen in hypothyroidism, even in absence of effusion [5], cardiac amyloidosis, scleroderma, and in chronic ischemic heart disease. Other conditions such as obesity, chronic obstructive pulmonary disease, a pneumothorax or pleural effusions may also increase the impedance across the chest wall, decreasing the EKG amplitude (Table 4.1, Fig. 4.2).

Table 4.1
Differential diagnosis of the low voltage EKG
Hypothyroidism – myxedematous involvement of myocardium |
Chronic obstructive pulmonary disease |
Infiltrative heart disease: ex. amyloidosis, scleroderma |
Chronic ischemic heart disease |
Pleural effusion |
Pneumothorax |
Obesity |

Fig. 4.2
Low voltage EKG: note the low amplitude of the signal in both the limb and precordial leads relative to normal gain signal at the beginning of the tracing
PR Deviation

Changes in the PR segment are present in approximately 80 % of patients with acute pericarditis, PR deviation is a particularly sensitive sign of pericardial effusion [6], and often persists after the ST segment changes have resolved and are not subject to the same confounding variables that affects ST segments. It is of diagnostic utility even in the presence of existing bundle branch block, acute myocardial infarction and LVH [7, 8]. Typically, in pericardial disease PR depressions are seen in both the limb and precordial leads. Particularly suggestive of pericarditis is PR elevation, occasionally in V1, but most commonly in AVR. These findings are thought to represent pressure mediated atrial injury of a mechanism similar to the ventricular injury associated ST elevations [9]. Measuring PR deviation can be challenging particularly due to the need for an appropriate electrocardiographic isoelectric reference baseline to measure against. This is evidenced by the fact that the persistent PR depression is often confused with continued ST segment elevation in these patients [6].
The differential diagnosis of PR deviation is more limited; in addition to pericarditis, it is rarely seen in patients with early ventricular repolarization (Fig. 4.3).
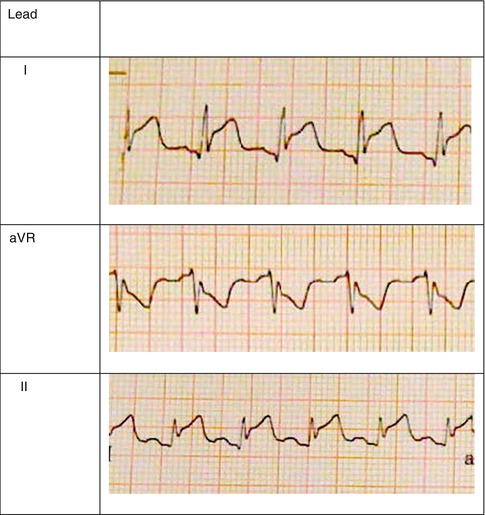
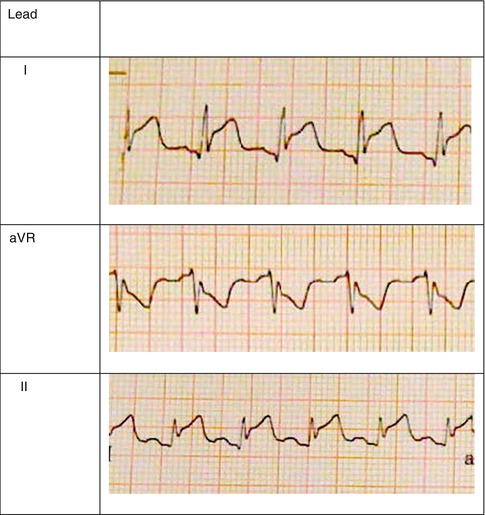
Fig. 4.3
PR deviation in acute pericarditis: note the depression of the PR segment below the baseline in leads I and II, and the PR elevation in aVR
Electrical Alternans

The accumulation of fluid around the heart releases the heart from its usual anatomic constraints and allows the heart free range to oscillate in the chest cavity. Typically, this will cause a varying QRS amplitude and vector, alternating from beat to beat, known as electrical alternans. In addition, in the presence of a pericardial effusion, respiratory variation in axis becomes more pronounced. This change is not seen from beat to beat, but rather gradually over a series of QRS complexes. It is important to note however, that while complete alternans of all components of the EKG is suggestive of cardiac tamponade, it is a specific but not highly sensitive sign [9]. Other conditions that can cause electrical alternans include [10] alternating bundle branch blocks causing differential patterns of myocardial depolarization, atrio-ventricular reentry utilizing an accessory pathway, ventricular bigeminy, where every alternate beat is ventricular in origin, alternans pre-excitation in which a supraventricular rhythm is alternately conducted via the atrioventricular node and via an accessory pathway, and the presence of a severe ventricular cardiomyopathy. Bidirectional ventricular tachycardias, as seen in patients with digitalis toxicity, catecholaminergic polymorphic ventricular tachycardia and Anderson-Tawil, or long QT seven syndrome, may also mimic electrical alternans [11, 12] (Table 4.2, Fig. 4.4).
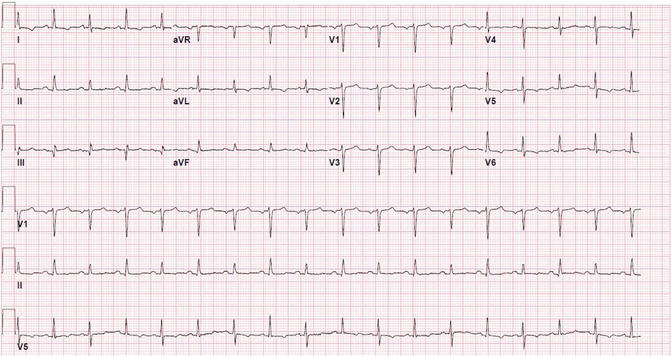
Table 4.2
Differential diagnosis of electrical alternans on EKG
Differential patterns of conduction caused by varying block |
AV reentry with accessory pathway |
Ventricular bigeminy |
Alternans pre-excitation |
Alternans bundle branch block |
Severe cardiomyopathy |
Bidirectional ventricular tachycardia |
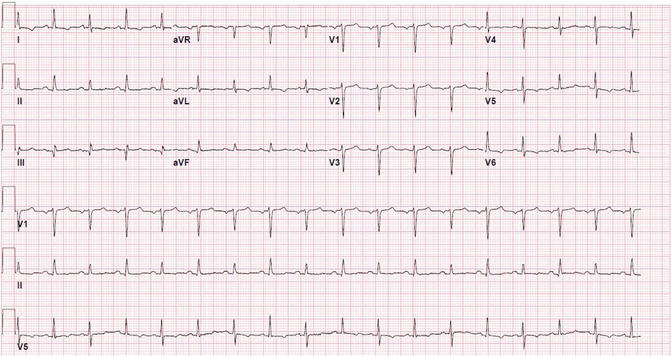
Fig. 4.4
Electrical alternans in acute pericarditis: note the alternating amplitude and axis of consecutive beats in the inferior and lateral leads
ST Segment Deviation

Deviation of the ST segment, specifically ST elevation, is present in approximately 90 % of patients with acute pericarditis. This is thought to represent myocardial injury, similar to that seen when direct pressure is applied to the myocardium when placing a pacing wire, and is termed a “current of injury”. The axis of these changes is predominantly inferior and anterior, very rarely involving the right sided leads or V1. The mechanism of this injury is multifactorial and is postulated to be due to the increased pressure exerted by the pericardial fluid on the epicardial aspect of the myocardium as well as inflammation of the myocardium. It is important to note the possibility of generating transient ST elevation in patients with pericarditis who exercise, and therefore the ST segment changes seen in these patients may vary based on heart rate. The differential diagnosis for ST elevation is quite broad as ST elevation is seen in a large number of normal and pathological processes.
Normal Variant
There is a normal variant of repolarization which is common in younger males, a demographic frequently affected by pericarditis. To differentiate this from pericardial disease, it is important to note that normal variant ST elevation is usually only present in the precordial leads and not in the limb leads. Additionally the QRS amplitude in the left lateral leads is greater in the “normal variant” than in pericarditis [13, 14].
Early Repolarization
The pattern of early ventricular repolarization has similar changes to the first stage of pericarditis [14]. Early studies suggested that in patients with early repolarization, these changes vanish or greatly diminish with the administration of isoproterenol or with exercise, while the changes get worse with the same maneuvers in patients with pericarditis. However, it is important to note that exercising patients with pericarditis has been shown to worsen outcomes [15]. Additionally, a report by Saviolo et al. demonstrates that these findings are not universally true [16].
Neurological Injury
Spinal cord injury, specifically damage to the C5 and C6 segments which provide sympathetic innervation to the heart can also cause elevation of the ST segment. Significantly however, these changes reverse with the administration of isoproterenol, demonstrating how sympathetic tone modulates ventricular repolarization [17].
Cardioversion
ST elevations may be seen in patients immediately after direct current cardioversion. These changes will resolve with time.
Acute Coronary Syndrome
Among the many conditions that mimic acute pericardial disease, it is perhaps most important to differentiate between pericardial disease and acute myocardial injury. Typically, the changes seen in acute myocardial injury are confined to the distribution of individual coronary arteries, while the changes of pericarditis are more global, reflecting the global pressure of the surrounding fluid on the chambers of the heart. Additionally, the terminal component of the QRS may merge directly into the ST segment elevation in acute ischemia, as opposed to pericardial disease, where the QRS morphology remains unchanged, but is followed by an elevated ST segment. Most importantly, perhaps is the morphology of the ST segment which in acute coronary syndrome is convex, with effacement of the T wave, while in pericardial disease the ST segment is concave and preserves the morphology of the T wave [18] (Table 4.3, Fig. 4.5).
Table 4.3
Partial list of differential diagnosis of etiologies of ST segment elevation
Normal variant |
Early repolarization
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|