Cardiac resynchronization therapy (CRT) has a symptomatic and survival benefit for patients with heart failure (HF), but the percentage of nonresponders remains relatively high. The aims of this study were to assess the clinical significance of baseline tricuspid regurgitation (TR) or worsening TR after implantation of a CRT device on the response to therapy. This is a multicenter retrospective analysis of prospectively collected databases that includes 689 consecutive patients who underwent implantation of CRT. The patients were divided into groups according to baseline TR grade and according to worsening TR within 15 months after device implantation. Outcome was assessed by clinical and echocardiographic response within 15 months and by estimated survival for a median interquartile range follow-up time of 3.3 years (1.6, 4.6). TR worsening after CRT implantation was documented in 104 patients (15%). These patients had worse clinical and echocardiographic response to CRT, but worsening of TR was not a significant predictor of mortality (p = 0.17). According to baseline echocardiogram, 620 patients (90%) had some degree of TR before CRT implant. Baseline TR was an independent predictor of worse survival (p <0.001), although these patients had significantly better clinical and echocardiographic response compared with patients without TR. In conclusion, worsening of TR after CRT implantation is a predictor of worse clinical and echocardiographic response but was not significantly associated with increased mortality. Baseline TR is associated with reduced survival despite better clinical and echocardiographic response after CRT implantation.
Cardiac resynchronization therapy (CRT) improves survival and quality of life in patients with advanced systolic heart failure (HF) and prolonged QRS duration. However, 30% to 35% of patients fail to respond to CRT. Reasons postulated for nonresponse have included suboptimal left ventricular (LV) lead position, poor patient selection, and suboptimal atrioventricular or ventriculoventricular timing, all suggesting inadequate resynchronization of the ventricles. However, we hypothesize that tricuspid regurgitation (TR), at times caused by the right ventricular (RV) lead placed as part of a CRT system, may be an under-recognized cause of hemodynamic nonresponse despite appropriate resynchronization of the left ventricle. Recognition of this mechanism, if present, is critical as it would have important implications for CRT implantation and device design. To test the hypothesis that TR adversely affects response and survival after CRT implantation, we performed a multicenter retrospective analysis of prospectively collected databases.
Methods
Data were prospectively collected at Mayo Clinic, Rochester, Minnesota, and Sheba Medical Center, Tel Hashomer, Israel, and subsequently pooled using prespecified joint definitions to ensure data consistency. The pooled database included 689 patients who underwent implantation of CRT or upgrade of other devices to CRT (87% of the patients were also implanted with a defibrillator) from 2002 to 2011. CRT was implanted according to pertinent American College of Cardiology/American Heart Association/Heart Rythm Society guidelines (New York Heart Association [NYHA] class II to IV symptomatic HF despite optimal medical therapy, EF ≤35%, and QRS duration of ≥120 milliseconds). All clinical and echocardiographic data before and after the implantation were prospectively collected into CRT databases in both institutions, and only patients with TR data at baseline (within 12 months before implant) and at some point during the first 15 months of follow-up (minimum of 1 week after implant) were included. The institutional review board of both centers approved the protocol.
Registered diagnostic cardiac sonographers from each center performed echocardiography, and experienced echocardiographers interpreted the results. Parameters recorded included LVEF (calculated using the modified Simpson’s formula), LV end-diastolic dimension (LVEDD) (measured with m-mode or 2-dimensional echocardiography), LV end-systolic dimension (LVESD), pulmonary artery systolic pressure (PASP) (estimated from the TR velocity and an estimate of right atrial pressures), mitral valve regurgitation (MR) and TR grade (0, none; 1, trivial/mild; 2, moderate; 3, severe; based on jet characteristics and/or proximal isovelocity surface area method), and RV function (semiquantitative grading scale: 0, normal; 0.5, borderline; 1, mild; 1.5, mild-moderate; 2, moderate; 2.5, moderate-severe; 3, severe dysfunction). Worsening TR was defined by an increase in grade of ≥1, within 15 months of the CRT implant.
Device implantation was performed as per standard clinical practice. The position of the LV lead was prioritized as lateral/posterolateral, anterolateral, anterior, and middle cardiac veins whenever possible as dictated by pacing thresholds, diaphragmatic stimulation, and ability to cannulate the veins. Standard settings included an atrioventricular delay of 100 milliseconds (sensed) and 130 milliseconds (paced), with DDD or DDDR mode, and standard lower (50 to 60 bpm) and upper (120 to 130 bpm) pacing rates. Patients were programmed either nominally as mentioned or by physician’s preference or by echocardiogram-based atrioventricular delay optimization. After implantation, patients were continuously monitored overnight. Pocket assessment, chest radiography, and repeat device interrogation were performed on the following day.
After implantation, patients were asked to return for follow-up after 6 and 12 months. All 689 patients had quantification of LVEF with repeat echocardiography and reassessment of HF symptoms according to the NYHA scale during a follow period of up to 15 months after implantation. The median (interquartile range) time from CRT implantation to post-CRT echocardiography was 9 months (5.5, 12.0). The device was interrogated to ensure normal function. Survival information was obtained from the electronic medical records and the national death database.
Continuous variables are summarized as mean ± SD and categorical variables as count (percentage). Differences in continuous variables among the 4 levels of baseline TR grade (none, trivial/mild, moderate, and severe) were tested using linear regression, and differences in categorical variables among the 4 levels of baseline TR grade were tested using the chi-square test. Similar tests were used to assess differences among those with any TR (trivial/mild, moderate, severe) versus no TR and no worsening in TR versus those with worsening TR. Linear regression was also used to assess differences in the continuous measures of change from baseline to post-CRT among the groups after adjusting for age, sex, medical therapy for HF (beta blockers, angiotensin-converting enzyme/angiotensin receptor blocker, and mineralocorticoid receptor antagonists), baseline clinical and echocardiographic parameters (NYHA class, LVEF, PASP, severe MR), QRS morphology (LBBB vs non-LBBB), and defibrillator implantation. Survival is summarized with Kaplan-Meier curves within each group, and a log-rank test was used to assess differences in survival across the groups. All subjects were required to have a post-CRT implantation echocardiogram to be included in the study and, thus, had to survive until that point. Therefore, survival time was calculated as time from post-implant echocardiogram date to death or last follow-up. Short-term survival was assessed by censoring patients who lived >2.5 years after the post-implant echocardiogram at 2.5 years. Cox proportional hazard models were used to assess differences in survival after adjusting for the same list of variables defined earlier.
Results
The study cohort included 689 patients (79% men), and the mean age at the time of CRT implant was 68 years. Most patients were in NYHA class III HF (76%) with a mean LVEF of 24.5 ± 7.5%. Sixty-nine patients (10%) had no TR before implantation and 620 patients (90%) had some degree of TR on baseline echocardiographic examination (378 [55%] trivial/mild, 167 [24%] moderate, and 75 [11%] severe). Baseline characteristics of the study population according to TR grade before CRT implantation are listed in Table 1 .
| Characteristics | N | None (N=69) | Trivial/Mild (N=378) | Moderate (N=167) | Severe (N=75) | P value |
|---|---|---|---|---|---|---|
| Age (years) | 689 | 65.6 ± 10.6 | 67.5 ± 11.7 | 68.7 ± 12.8 | 68.3 ± 10.2 | 0.29 |
| Men | 689 | 59 (86%) | 291 (77%) | 138 (83%) | 57 (76%) | 0.22 |
| Cardiac Resynchronization Therapy with a defibrillator | 689 | 60 (87%) | 327 (87%) | 145 (87%) | 67 (89%) | 0.93 |
| Prior Pacemaker/Defibrillator | 688 | <.001 | ||||
| None | 60 (87%) | 256 (68%) | 86 (51%) | 33 (44%) | ||
| Upgrade from a pacemaker | 6 (9%) | 77 (20%) | 38 (23%) | 21 (28%) | ||
| Upgrade from a defibrillator | 3 (4%) | 44 (12%) | 43 (26%) | 21 (28%) | ||
| Dilated cardiomyopathy | 686 | 32 (46%) | 164 (44%) | 62 (37%) | 31 (42%) | 0.46 |
| Beta Blockers | 680 | 58 (88%) | 342 (91%) | 147 (89%) | 65 (89%) | 0.71 |
| Angiotensin converting enzyme inhibitor/ Angiotensin receptor blocker | 681 | 59 (89%) | 325 (87%) | 139 (83%) | 56 (77%) | 0.10 |
| Mineralocorticoid receptor antagonist | 680 | 28 (43%) | 130 (35%) | 57 (34%) | 32 (44%) | 0.28 |
| QRS morphology | 681 | <.001 | ||||
| Normal | 0 | 7 (2%) | 4 (2%) | 2 (3%) | ||
| Left bundle branch block | 44(67%) | 186 (49%) | 61 (37%) | 25 (33%) | ||
| Right bundle branch block | 7 (11%) | 27 (7%) | 16 (10%) | 9 (12%) | ||
| Intraventricular conduction delay | 9 (14%) | 60 (16%) | 21 (13%) | 6 (8%) | ||
| Paced | 6 (9%) | 82 (22%) | 57 (35%) | 29 (39%) | ||
| QRS < 120ms | 0 | 15 (4%) | 4 (2%) | 4 (5%) | ||
| New York Heart Association class | 682 | <.001 | ||||
| I | 0 | 3 (1%) | 0 | 0 | ||
| II | 7 (10%) | 53 (14%) | 14 (9%) | 3 (4%) | ||
| III | 59 (87%) | 286 (76%) | 116 (71%) | 54 (72%) | ||
| IV | 2 (3%) | 33 (9%) | 34 (21%) | 18 (24%) | ||
| QRS duration (ms) | 677 | 160.5 ± 29.0 | 161.1 ± 33.1 | 168.0 ± 32.4 | 170.8 ± 36.9 | 0.03 |
| Left ventricular ejection fraction (%) | 689 | 25.2 ± 7.2 | 24.9 ± 7.2 | 23.5 ± 8.0 | 24.1 ± 7.7 | 0.17 |
| Left ventricular end diastolic dimension (mm) | 680 | 65.6 ± 11.9 | 65.6 ± 9.1 | 64.9 ± 9.4 | 63.8 ± 7.6 | 0.47 |
| Left ventricular end systolic dimension (mm) | 624 | 54.3 ± 12.8 | 55.9 ± 10.5 | 56.3 ± 10.8 | 56.0 ± 9.1 | 0.66 |
| Right ventricular dysfunction | 620 | 0.9 ± 0.9 | 0.9 ± 0.9 | 1.4 ± 0.8 | 1.7 ± 0.9 | <.001 |
| Mitral valve regurgitation grade | 676 | <.001 | ||||
| None | 33 (48%) | 34 (9%) | 17 (10%) | 10 (14%) | ||
| Trivial/mild | 25 (36%) | 184 (50%) | 42 (25%) | 10 (14%) | ||
| Moderate | 10 (14%) | 110 (30%) | 72 (43%) | 28 (38%) | ||
| Severe | 1 (1%) | 39 (11%) | 35 (21%) | 26 (35%) | ||
| Pulmonary Artery Systolic Pressure (mmHg) | 642 | 36.4 ± 9.6 | 42.5 ± 13.6 | 54.5 ± 14.6 | 54.2 ± 13.1 | <.001 |
| Study center | 689 | |||||
| Sheba | 42 (61%) | 150 (40%) | 23 (14%) | 11 (15%) | ||
| Mayo | 27 (39%) | 228 (60%) | 144 (86%) | 64 (85%) |
During follow-up time, 104 patients (15%) had TR worsening after CRT implantation. The baseline characteristics of patients with and without TR worsening are listed in Table 2 . Patients without TR worsening had better clinical and echocardiographic response to CRT compared to patients with TR worsening after implantation ( Table 3 ). The association between worsening TR and poor response to CRT remained significant after adjusting for a number of variables (age, gender, medical therapy for HF, baseline clinical and echocardiographic parameters, QRS morphology, and defibrillator implantation) with less improvement in NYHA class (p <0.001), LVEF (p = 0.04), LVESD (p = 0.01), MR, and PASP (p <0.001). TR was still not associated with significant change in LVEDD (p = 0.38) or RV function (p = 0.17) after adjustment.
| Characteristics | N | Worsening Tricuspid Regurgitation | P value | |
|---|---|---|---|---|
| No (N=585) | Yes (N=104) | |||
| Age (years) | 689 | 67.5 ± 11.8 | 68.8 ± 11.3 | 0.31 |
| Men | 689 | 468 (80%) | 77 (74%) | 0.17 |
| Prior Pacemaker/Defibrillator | 688 | 0.28 | ||
| None | 362 (62%) | 73 (70%) | ||
| Upgrade from a pacemaker | 125 (21%) | 17 (16%) | ||
| Upgrade from a defibrillator | 97 (17%) | 14 (13%) | ||
| Dilated cardiomyopathy | 686 | 240 (41%) | 49 (47%) | 0.26 |
| Beta Blockers | 680 | 529 (91%) | 83 (82%) | 0.005 |
| Angiotensin converting enzyme inhibitor/Angiotensin receptor blocker | 681 | 488 (84%) | 91 (90%) | 0.12 |
| Mineralocorticoid receptor antagonist | 680 | 211 (36%) | 36 (36%) | 0.88 |
| QRS morphology | 681 | 0.20 | ||
| Normal | 13 (2%) | 0 | ||
| Left bundle branch block | 271 (47%) | 45 (45%) | ||
| Right bundle branch block | 50 (9%) | 9 (9%) | ||
| Intraventricular conduction delay | 75 (13%) | 21 (21%) | ||
| Paced | 151 (26%) | 23 (23%) | ||
| QRS < 120ms | 21 (4%) | 2 (2%) | ||
| New York Heart Association class | 682 | 0.72 | ||
| I | 3 (1%) | 0 | ||
| II | 68 (12%) | 9 (9%) | ||
| III | 436 (75%) | 79 (77%) | ||
| IV | 73 (13%) | 14 (14%) | ||
| QRS duration (ms) | 677 | 164.3 ± 33.1 | 161.5 ± 33.4 | 0.44 |
| Left ventricular ejection fraction (%) | 689 | 24.6 ± 7.4 | 23.9 ± 7.7 | 0.41 |
| Left ventricular end diastolic dimension (mm) | 680 | 65.0 ± 9.4 | 66.2 ± 9.3 | 0.23 |
| Left ventricular end systolic dimension (mm) | 624 | 55.8 ± 10.7 | 56.3 ± 11.0 | 0.64 |
| Right ventricular dysfunction | 620 | 1.1 ± 1.0 | 1.0 ± 0.9 | 0.63 |
| Baseline mitral valve regurgitation grade | 676 | 0.009 | ||
| None | 69 (12%) | 25 (24%) | ||
| Trivial/mild | 222 (39%) | 39 (38%) | ||
| Moderate | 191 (33%) | 29 (28%) | ||
| Severe | 90 (16%) | 11 (11%) | ||
| Baseline tricuspid regurgitation grade | 689 | <.001 | ||
| None | 31 (5%) | 38 (37%) | ||
| Trivial/mild | 326 (56%) | 52 (50%) | ||
| Moderate | 153 (26%) | 14 (13%) | ||
| Severe | 75 (13%) | 0 | ||
| Pulmonary Artery Systolic Pressure (mmHg) | 642 | 46.4 ± 14.7 | 46.3 ± 16.2 | 0.92 |
| Study center | 689 | 0.35 | ||
| Sheba | 196 (34%) | 30 (29%) | ||
| Mayo | 389 (66%) | 74 (71%) | ||
| variable | N | Worsening tricuspid regurgitation | P value | |
|---|---|---|---|---|
| No (N=585) | Yes (N=104) | |||
| Change in New York Heart Association class | 563 | -0.6 ± 0.8 | -0.2 ± 0.8 | <.001 |
| Change in left ventricular ejection fraction (%) | 689 | 7.1 ± 11.5 | 4.4 ± 10.7 | 0.02 |
| Change in left ventricular end diastolic dimension (mm) | 668 | -2.4 ± 6.8 | -1.6 ± 6.9 | 0.29 |
| Change in left ventricular end systolic dimension (mm) | 563 | -4.4 ± 8.6 | -2.2 ± 8.8 | 0.03 |
| Change in right ventricular dysfunction | 578 | -0.2 ± 0.9 | 0.0 ± 0.9 | 0.20 |
| Change in mitral regurgitation grade | 669 | -0.3 ± 0.8 | 0.1 ± 0.9 | <.001 |
| Change in Pulmonary Artery Systolic Pressure (mmHg) | 622 | -5.0 ± 12.6 | 0.3 ± 13.5 | <.001 |
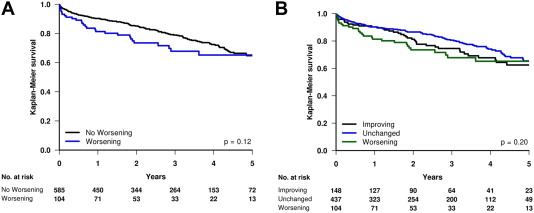
Over a median (interquartile range) follow-up time of 3.3 years (1.6, 4.6), post-implant worsening of TR was not significantly associated with mortality either compared to all patients without TR worsening (p = 0.12; Figure 1 ) or when grouped as worsening TR, improved TR, and unchanged TR (p = 0.20; Figure 1 ). However, the Kaplan-Meier curves suggested that survival may be different during the short-term follow-up period, and when we limited the follow-up time to 2.5 years, worsening TR was associated with poor short-term survival compared with no worsening (p = 0.03). After adjustment for the list of variables mentioned earlier, survival was not significantly different for those with worsening TR compared to those without worsening (hazard ratio [HR] 1.36 [0.88, 2.10]; p = 0.17), and the difference in short-term survival was no longer significant (HR 1.63 [0.98, 2.73]; p = 0.06).