Alpha-1 antitrypsin (AAT) has broad anti-inflammatory and immunomodulating properties in addition to inhibiting serine proteases. Administration of human plasma–derived AAT is protective in models of acute myocardial infarction in mice. The objective of this study was to determine the safety and tolerability of human plasma–derived AAT and its effects on the acute inflammatory response in non-AAT deficient patients with ST-segment elevation myocardial infarction (STEMI). Ten patients with acute STEMI were enrolled in an open-label, single-arm treatment study of AAT at 60 mg/kg infused intravenously within 12 hours of admission and following standard of care treatment. C-reactive protein (CRP) and plasma AAT levels were determined at admission, 72 hours, and 14 days, and patients were followed clinically for 12 weeks for the occurrence of new onset heart failure, recurrent myocardial infarction, or death. Twenty patients with STEMI enrolled in previous randomized trials with identical inclusion and/or exclusion criteria, but who received placebo, served as historical controls. Prolastin C was well tolerated and there were no in-hospital adverse events. Compared with historical controls, the area under the curve of CRP levels was significantly lower 14 days after admission in the Prolastin C group (75.9 [31.4 to 147.8] vs 205.6 [78.8 to 410.9] mg/l, p = 0.048), primarily due to a significant blunting of the increase occurring between admission and 72 hours (delta CRP +1.7 [0.2 to 9.4] vs +21.1 [3.1 to 38.0] mg/l, p = 0.007). Plasma AAT levels increased from admission (149 [116 to 189]) to 203 ([185 to 225] mg/dl) to 72 hours (p = 0.005). In conclusion, a single administration of Prolastin C in patients with STEMI is well tolerated and is associated with a blunted acute inflammatory response.
Anti-inflammatory strategies have been object of investigation in ST-segment elevation myocardial infarction (STEMI). We have recently provided data on the safety and efficacy of interleukin-1 blockade with anakinra (recombinant human interleukin-1 receptor antagonist) in 20 patients with STEMI. We now present the results of a different strategy to inhibit the inflammatory response during STEMI using plasma-derived alpha-1 antitrypsin (AAT; Prolastin C) in 10 clinically stable patients with STEMI, to appraise its safety and tolerability.
Methods
From January 15, 2014, consecutive patients presenting to our institution with suspected STEMI were screened for enrollment. Inclusion criteria were age >18 years, acute (<24 hours) onset of chest pain, new or presumably new ST-segment elevation (>1 mm) in ≥2 anatomically contiguous leads, and planned or completed urgent percutaneous coronary intervention (PCI). Exclusion criteria were lack of informed consent; cardiac arrest; unsuccessful PCI; urgent surgery; hemodynamic instability; previous Q-wave infarction; preexisting heart failure stage C or D of New York Heart Association class IV; left ventricular ejection fraction (LVEF) <20% or severe valve disease; pregnancy or breastfeeding; chronic infectious, autoinflammatory or autoimmune disease or cancer; recent (<14 days) use of anti-inflammatory drugs (other than nonsteroidal anti-inflammatory drugs); previous allergic reactions to Prolastin C or other formulations of plasma-derived AAT; and known immunoglobulin A deficiency.
This study ( www.clinicaltrials.gov NCT01936896 ; Figure 1 ) was approved by the Virginia Commonwealth University’s Institutional Review Board and all patients provided written consent. Plasma levels of C-reactive protein (CRP, high-sensitivity nephelometry, LabCorp, Burlington, North Carolina) and plasma AAT (immunoturbidimetric assay) were measured at admission, 72 hours, and 14 days. Creatine kinase-MB (direct chemiluminescent technology) were obtained and followed until peak, as a surrogate for infarct size. Clinical follow-up was performed up to week 12.
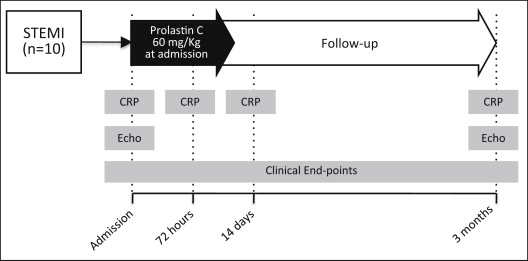
All patients received a single infusion of 60 mg/kg of Prolastin C (Grifols USA, Los Angeles, California) as a single-arm open-label treatment. The infusion was given at a rate of 0.08 ml/Kg min (lasting between 12 to 18 minutes) in the coronary intensive care unit under continuous electrocardiographic monitoring and with vital signs checked every 10 minutes. An investigational new drug use was granted by the Food and Drug Administration to the investigators (investigational new drug 15636). Doppler echocardiography was performed within 48 hours of admission and at 3-month follow-up weeks later or according to standard of care. Initial measurements and calculations were performed at time of study completion; they were repeated off-line at the end of the study by an additional reader unaware of the treatment, and averaged between the 2 measurements, with all measurements having a difference of <5%.
Twenty patients with STEMI enrolled in 2 previous randomized trials with identical inclusion and exclusion criteria at our institution and who received placebo, served as historical controls for comparison. The primary end point was the difference in the area under the curve for CRP levels comparing AAT-treated patients with the historical placebo-treated patients. Secondary end points included the difference in the increase of CRP between admission and 72 hours and the 72 hours CRP levels. Due to the unblinded nature of the study, all other end points were recorded for safety assessment, and comparisons should be considered hypothesis-generating. These exploratory end points included the infusion reactions, treatment-related adverse events, in-hospital and 3-month adverse events, and changes in LVEF.
Based on previous data showing a large increase in CRP within 72 hours of the STEMI, we calculated that a sample size of 10 patients would provide a power of >80% (alpha 0.05), allowing for a 20% loss to follow-up, to show a >50% reduction in the area under the curve for CRP levels. The values are reported as median and interquartile range for potential deviations from Gaussian distribution. Differences between groups were computed using the Mann-Whitney U test for continuous variables or Fisher’s exact test for discrete variables. Paired data within the Prolastin C group (before or after) were analyzed using the Wilcoxon test. The Spearman correlation test was used to evaluate the correlation between continuous variables. Unadjusted p values are reported, with significance set at 2-tailed 0.05 level. Computations were performed with SPSS 19.0 (IBM, Armonk, New York).
Results
From January 2014 to March 2014, we screened 17 patients admitted with STEMI and enrolled 10 patients ( Table 1 ). The characteristics of the individual placebo controls can be found in the original publications. Supplementary Table 1 summarizes the clinical characteristics of the Prolastin C group and the historical placebo controls in terms of age, ethnicity, risk factors, and clinical characteristics. There were significantly more women in the Prolastin C group (5 [50%]) than in the historical placebo cohort (2 [90%], p = 0.026). All patients underwent PCI with balloon angioplasty and coronary stenting in 9 (90%) patients. Prolastin C was administered at a median of 320 (260 to 444) minutes after PCI. None of the patients experienced any adverse infusion reactions. There were no clinically significant changes in blood pressure, heart rate, and temperature during infusions ( Table 2 ).
| Age (yrs) | Gender | Ethnicity | Hypertension | Diabetes | Time from chest pain to PCI (min) | Time from chest pain to drug (min) | CAD (culprit) | TIMI flow (initial) | TIMI flow (final) | Coronary stenting | Peak CK-MB (ng/ml) | Adverse clinical events (time) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| #1 | 33 | F | C | N | N | 138 | 310 | Ramus | 0 | 3 | + | 191 | Pulmonary Embolism (11 weeks) |
| #2 | 43 | M | C | Y | N | 90 | 558 | LM/LAD | 1 | 3 | + | 153 | |
| #3 | 46 | M | C | Y | N | 50 | 360 | PLB | 1 | 3 | + | 82 | |
| #4 | 47 | F | C | N | N | 60 | 431 | RCA | 0 | 3 | + | 36 | Sudden Death (8 weeks) |
| #5 | 49 | F | C | N | Y | 150 | 480 | RCA | 0 | 3 | + | 159 | |
| #6 | 56 | M | C | Y | N | 80 | 210 | RCA | 0 | 3 | + | 13 | |
| #7 | 58 | F | C | N | N | 553 | 810 | LAD | 1 | 3 | + | 379 | |
| #8 | 59 | M | AA | Y | N | 120 | 625 | RCA | 0 | 3 | + | 92 | |
| #9 | 67 | M | AA | N | N | 60 | 330 | RCA | 0 | 3 | + | 209 | |
| #10 | 77 | F | AA | N | N | 30 | 510 | RCA | 0 | 3 | + | 8 |
| Prior to Infusion | End of Infusion | |
|---|---|---|
| Systolic blood pressure (mmHg) | 128 [108-139] | 125 [115-135] |
| Diastolic blood pressure (mmHg) | 77 [64-89] | 70 [61-75] |
| Heart rate (_/min) | 74 [61-89] | 70 [64-78] |
| Oxygen saturimetry (%) | 98 [96-99] | 98 [96-99] |
| Temperature (oral, C°) | 36.7 [36.6-36.8] | 36.6 [36.4-36.9] |
| Pain/Discomfort (0/10 scale) | 0 [0-0] | 0 [0-0] |
Peak creatine kinase-MB, an estimate of infarct size, was remarkably similar between patients treated with AAT (123 [48 to 183] ng/ml) and historical placebo controls (123 [77 to 189] ng/ml, p = 0.85). The use of guideline-recommended treatments at discharge was not different comparing Prolastin C versus placebo controls ( Supplementary Table 2 ). Three (30%) patients had staged PCI for nonculprit lesions during the index hospitalization in the Prolastin C group and 2 (10%) in the historical control group. None of the patients experienced in-hospital complications, including no episodes of acute kidney injury.
Prolastin C treatment significantly increased plasma AAT levels at 72 hours from 149 (116 to 189) to 203 (185 to 225) mg/dl (p = 0.005). CRP levels at admission, 72 hours, and 14 days in Prolastin C-treated patients are listed in Figure 2 . The CRP levels of placebo-treated patients are also shown for comparison. Compared with historical placebo controls, Prolastin C led to a significantly smaller area under the curve for CRP levels (75.9 [31.4 to 147.8] vs 205.6 [78.8 to 410.9] mg/l, p = 0.048), primarily due to a significantly blunting of the increase between admission and 72 hours (delta CRP +1.7 [0.2 to 9.4] vs +21.1 [3.1 to 38.0] mg/l, p = 0.007; Figure 2 ). In Prolastin C-treated patients, white blood cell count was 8,700 (5,450 to 14,325) cells/mm 3 at admission, without significant changes at 24 hours (8,000 [6,275 to 13,325] cells/mm 3 , p = 0.28 vs admission) and at 72 hours (8,150 [5,275 to 10,725] cells/mm 3 ). No significant differences between Prolastin C and placebo-treated groups in white blood cell count at admission, 24 hours, or 72 hours were found (all p >0.42). There was no correlation between CRP levels and clinical variables listed in Table 1 .




