To assess the incidence of atrial fibrillation (AF) and the clinical impact of AF types on outcomes in patients with acute myocardial infarction (AMI) treated invasively, we analyzed 2,980 consecutive patients with AMI admitted to our department from 2003 through 2008. Data collected by the insurer were screened to identify patients who died during the median follow-up of 41 months. AF was recognized in 282 patients (9.46%, AF group); the remaining 2,698 patients (90.54%) were free of this arrhythmia (control group). The AF group was divided into 3 subgroups: prehospital paroxysmal AF (n = 92, 3.09%), new-onset AF (n = 109, 3.66%), and permanent AF (n = 81, 2.72%). In-hospital and long-term mortalities were significantly higher (p <0.001 for the 2 comparisons) in the AF than in the control group (14.9% vs 5.3%, 37.2% vs 17.0%, respectively). Long-term mortality was significantly higher (p <0.001 for the 2 comparisons) in the new-onset AF (35.8%) and permanent AF (54.3%) groups than in the control group but did not differ significantly between the prehospital AF and control groups (21.7% vs 17.0%, p = NS). Considering types of arrhythmia separately, only permanent AF (hazard ratio 2.59) was an independent risk factor for death in the studied population. In conclusion, AF occurs in 1 of 10 patients with AMI treated invasively, with nearly equal distributions among prehospital, new-onset, and permanent forms. Although arrhythmia is a marker of worse short- and long-term outcomes, only permanent AF is an independent predictor for death in this population.
Atrial fibrillation (AF) is the most common supraventricular tachyarrhythmia in the general population and in patients after acute myocardial infarction (AMI). The incidence of AF in patients with AMI is significantly higher compared to the general population, and it has been reported to be 5% to 23%. AF is a well-established marker of poor short- and long-term prognoses in patients with AMI and is associated with a twofold increase in mortality in this population. However, little is known about the impact of AF type on in-hospital and long-term mortalities in patients with AMI treated invasively.
Methods
All analyses were conducted using a single-center database of 2,980 consecutive patients presenting with AMI and admitted to our department from 2003 through 2008. Coronary angiography and subsequent percutaneous coronary intervention (PCI) were performed in all patients without delay. A single dose of aspirin (300 to 500 mg) and intravenous heparin 5,000 to 10,000 U were administered to all patients before coronary angiography, and a loading dose of clopidogrel was given before stent implantation. PCI was conducted with strict monitoring of activated clotting time, and, if necessary, additional boluses of heparin were administered to achieve an appropriate activated clotting time (350 to 450 seconds). Duration of dual antiplatelet therapy was in line with current recommendations of cardiac societies.
Data concerning baseline, demographic, clinical, laboratory, echocardiographic, and angiographic characteristics were obtained from a single-center registry of acute coronary syndromes. Remote follow-up was accomplished based on data obtained from the insurer—the National Health Fund, which covers >99% of the treated population.
The study population was divided into 2 groups: patients with a history of AF and those without AF (control group). Subsequently, the AF group was divided further into 3 subgroups: patients with nonpermanent prehospital-only AF (prehospital AF group), patients with nonpermanent in-hospital detected AF (new-onset AF group), and patients with permanent AF (permanent AF group).
AF was defined as electrocardiographically documented evidence of an irregular ventricular rhythm with no discernible P waves. Permanent AF was considered in patients with a history of permanent AF before index hospitalization. New-onset AF was considered in patients with AF during index hospitalization but not in their medical history. Nonpermanent prehospital-only AF was defined as a history of AF with no evidence of this arrhythmia during index hospitalization. Assessment of renal function was based on glomerular filtration rate as calculated by the abbreviated Modification of Diet in Renal Disease formula. Contrast-induced nephropathy was defined as an increase of serum creatinine by ≥44.2 μmol/L (0.5 mg/dl) or a 25% increase from baseline value within 48 hours after contrast exposure. Left ventricular ejection fraction (LVEF) <35% at discharge was considered severely decreased.
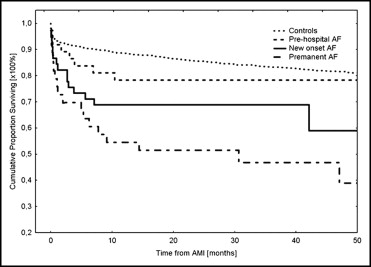
Continuous parameters were expressed as mean ± SD and categorical variables as number and percentage. Comparative analysis between groups was performed with Student’s t test for continuous variables and chi-square or Fisher’s exact test, as appropriate, for dichotomous parameters. Independent predictors of death were identified with the multivariate Cox regression model and expressed as hazard ratio (HR) with 95% confidence interval. All parameters that differed significantly between the AF group and the control group were considered covariates in multivariate analysis. In addition, 3 types of AF were incorporated as covariates into the Cox regression model. Cumulative proportions of patients free of death in every group were plotted as Kaplan–Meier survival curves and compared with log-rank tests between different categories. A p value <0.05 was considered statistically significant. Statistica 6.0 (StatSoft, Inc., Tulsa, Oklahoma) was used for statistical analysis.
Results
Of the 2,980 patients, AF was diagnosed in 282 (9.46%). Prehospital-only AF, new-onset AF, and permanent AF were diagnosed in 92 patients (3.09%), 109 patients (3.66%), and 81 patients (2.72%), respectively. Patients with AF had significantly (p <0.001 for all comparisons) more cardiovascular risk factors than those free of arrhythmia, i.e., they were significantly older and more frequently had diabetes mellitus, impaired renal function, and severely decreased LVEF. Patients with prehospital AF had a significantly lower incidence of impaired LVEF compared to patients with new-onset AF and those with permanent AF. The new-onset AF and permanent AF groups were similar in age, incidence of diabetes mellitus, impaired renal function, and decreased LVEF. Baseline characteristics of all groups are presented in Table 1 .
| Parameter | Prehospital AF | New-Onset AF | Permanent AF | AF Free |
|---|---|---|---|---|
| (n = 92) | (n = 109) | (n = 81) | (n = 2,698) | |
| Men | 44 (47.4%) † | 61 (56.0%) ⁎ | 56 (69.1%) | 1,905 (70.6%) |
| Age (years) | 66.9 ⁎ | 67.9 ⁎ | 67.6 ⁎ | 61.3 |
| Diabetes mellitus | 41 (44.6%) ⁎ | 69 (63.3%) † | 41 (50.6%) † | 831 (30.8%) |
| Hypertension | 63 (68.5%) ⁎ | 69 (63.3%) | 54 (66.7%) ⁎ | 1,452 (53.8%) |
| Hyperlipidemia | 42 (45.7%) | 30 (27.5%) † | 31 (38.3%) | 1,303 (48.3%) |
| Smokers | 40 (43.5%) ⁎ | 47 (43.1%) ⁎ | 35 (43.2%) ⁎ | 1,538 (57.0%) |
| Previous stroke | 5 (5.4%) | 12 (11.0%) ⁎ | 7 (8.6%) ⁎ | 116 (4.3%) |
| Previous acute myocardial infarction | 27 (29.3%) ⁎ | 32 (29.4%) ⁎ | 13 (16.0%) | 529 (19.6%) |
| Previous percutaneous coronary intervention | 5 (5.4%) | 14 (12.8%) | 8 (9.9%) | 281 (10.4%) |
| Previous coronary artery bypass grafting | 10 (10.9%) † | 10 (9.2%) ⁎ | 5 (6.2%) | 89 (3.3%) |
| Anterior ST-segment elevation infarction | 31 (33.7%) | 46 (42.2%) ⁎ | 32 (39.5%) | 885 (32.8%) |
| Non–ST-segment elevation infarction | 35 (38.0%) ⁎ | 19 (17.4%) | 18 (22.2%) | 645 (23.9%) |
| Shock on admission | 5 (5.4%) | 12 (11%) ⁎ | 7 (8.6%) | 156 (5.8%) |
| Incomplete revascularization | 43 (46.7%) | 55 (50.5%) | 47 (58.0%) | 1,317 (48.8%) |
| Multivessel disease | 71 (77.2%) ⁎ | 80 (73.4%) ⁎ | 52 (64.2%) | 1,719 (63.7%) |
| Duration of hospitalization (days) | 7.3 | 8.2 | 7.6 | 7.7 |
| Contrast-induced nephropathy | 27 (29.3%) | 51 (46.8%) † | 32 (39.5%) † | 618 (22.9%) |
| Hematocrit on admission (%) | 38.7 | 39.6 | 40.5 | 41.3 |
| Glomerular filtration rate <60 ml/min/1.73 m 2 | 34 (37.0%) † | 44 (40.4%) † | 29 (35.8%) † | 461 (17.1%) |
| Left ventricular ejection fraction (%) | 40.7 ⁎ | 36.9 ⁎ | 38.3 ⁎ | 43.9 |
| Left ventricular ejection fraction <35% | 17 (18.5%) | 39 (35.8%) † | 28 (34.6%) † | 326 (12.1%) |
| Thrombolysis | 1 (1.1%) | 2 (1.8%) | 2 (2.5%) | 59 (2.2%) |
| Glycoprotein IIb/IIIa receptor inhibitors | 12 (13.0%) | 16 (14.7%) | 14 (17.3%) | 388 (14.4%) |
| Vitamin K antagonists at discharge | 41 (44.6%) † | 29 (26.6%) † | 47 (58.0%) † | 5 (0.2%) |
| Acetylsalicylic acid at discharge | 90 (97.8%) | 107 (98.2%) | 80 (98.8%) | 2,652 (98.3%) |
| Thienopyridine at discharge | 87 (94.6%) | 104 (95.4%) | 78 (96.3%) | 2,596 (96.2%) |
| β Blockers at discharge | 86 (93.5%) | 103 (94.5%) | 77 (95.1%) | 2,506 (92.9%) |
| Angiotensin-converting enzyme inhibitors at discharge | 81 (88.0%) | 95 (87.2%) | 71 (87.7%) | 2,393 (88.7%) |
| Statins at discharge | 80 (87.0%) | 92 (84.4%) | 70 (86.4%) | 2,304 (85.4%) |
In-hospital, 30-day, 1-year, and remote mortalities during the median follow-up of 41.5 months were significantly higher (p <0.001 for all comparisons) in patients with AF than in controls. However, when comparing the arrhythmic subgroups to arrhythmia-free controls, only the permanent AF and new-onset AF groups had significantly higher short- and long-term mortalities than patients without AF ( Figure 1 ) . Comparing the outcomes between particular AF types, patients with permanent AF had significantly higher in-hospital, 30-day, 1-year, and long-term mortalities than the prehospital AF group and higher 1-year and long-term mortalities than the new-onset AF group ( Table 2 ).
| Variable | Prehospital AF | New-Onset AF | Permanent AF | AF Free |
|---|---|---|---|---|
| (n = 92) | (n = 109) | (n = 81) | (n = 2,698) | |
| In-hospital mortality | 7 (7.6%) | 14 (12.8%) ⁎ | 17 (21.0%) ⁎ † | 143 (5.3%) |
| 30-day mortality | 8 (8.7%) | 17 (15.6%) ⁎ | 20 (24.7%) ⁎ † | 162 (6.0%) |
| 1-year mortality | 13 (14.1%) | 34 (31.2%) ⁎ † | 37 (45.7%) ⁎ † ‡ | 254 (9.4%) |
| Total mortality | 20 (21.7%) | 39 (35.8%) ⁎ † | 44 (54.3%) ⁎ † ‡ | 459 (17.0%) |
⁎ p <0.001 versus group without atrial fibrillation.
† p <0.05 versus group with prehospital atrial fibrillation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


