The aim of this study was to describe the clinical importance and methods of transcatheter closure of systemic venous baffle leaks after atrial redirection procedures for transposed great vessels. Until the late 1970s, atrial redirection surgery was the principal surgical palliative approach to manage transposed great vessels. Baffle leaks are among the many long-term complications of this type of surgery, and their prevalence increases over time. The clinical consequences of baffle leaks in this population are poorly understood, and the indications for closure are incompletely defined. During outpatient follow-up of 126 patients after atrial redirection surgery, 15 baffle leaks were detected in 11 patients. All underwent transcatheter closure using either an occluding device or a covered stent if there was concomitant baffle obstruction. The average age at the time of the procedure was 26 years (range 6 to 42). Ten of 11 patients were cyanosed at rest or on a simple walk test (median oxygen saturation level 80%, range 65% to 96%). Six of 11 patients were polycythemic before leak closure (median hemoglobin concentration 19 g/dl, range 13.8 to 23). After closure, there was a significant improvement in saturation (median 97%, p <0.0001) and a significant reduction in hemoglobin concentration at 6 months after the procedure (median 14.8 g/dl, p <0.05). There were no procedural adverse events. One patient experienced late device embolization necessitating surgical removal. In conclusion, transcatheter closure of baffle leaks is a technically feasible although frequently complex and lengthy procedure. Closure is associated with an improvement in oxygen saturations and a reduction in polycythaemia.
Before the arterial switch operation, atrial redirection surgery was the standard approach for long-term palliation of patients with transposition of the great arteries. As a result, there exists a large cohort of patients under clinical follow-up with complex intra-atrial baffles to redirect systemic and pulmonary venous return (physiologically although not anatomically corrected circulations). Long-term complications relating to surgically placed intra-atrial baffles are common and include baffle obstruction and baffle leak, in addition to atrial bradyarrhythmia and tachyarrhythmia. A transcatheter approach to occlusion of baffle leaks has many potential advantages, including the avoidance of repeat sternotomy and cardiopulmonary bypass in patients with vulnerable morphologic right ventricles in the systemic position. The clinical benefits and effectiveness of routine transcatheter closure of many of these defects have not been demonstrated. We describe the diagnosis, management, and results of transcatheter baffle leak closure in a cohort of adult patients who underwent childhood atrial redirection procedures at our institution over the past 15 years.
Methods
Of 3,743 adult patients (aged >16 years) with congenital heart disease under regular follow-up at the Yorkshire Heart Centre (Leeds, United Kingdom), there are 246 patients with transposed great arteries as their principal diagnosis (6.6%). One hundred twenty-six of these patients underwent atrial redirection surgery in early life (48 Mustard, 78 Senning). This group of patients undergo yearly outpatient clinical evaluation, including transcutaneous oximetry in addition to other routine investigations (12-lead electrocardiography and transthoracic echocardiogram). Those patients found to be desaturated at rest (≤93%) undergo further detailed imaging of their intra-atrial baffles, including transthoracic echocardiography with a bubble study and transesophageal echocardiography or cardiac magnetic resonance imaging to fully delineate the size, margins, and location of baffle leaks before consideration of transcatheter defect closure. In desaturated patients, hemoglobin concentrations are routinely measured to look for polycythemia.
This study was a retrospective case series of all patients who underwent transcatheter baffle leak closure in the past 15 years, including demographics, surgical notes, intervention procedural data, and angiographic data. Additional information was obtained from archived echocardiographic examinations, cardiac magnetic resonance imaging studies, and cardiac catheterization procedures. After baffle leak occlusion, assessments of saturation at rest and during exercise were performed by pulse oximetry with a further assessment of hemoglobin concentration 6 months after the procedure. Clinical procedural success was defined as elimination of baffle leak as determined by normalization of saturation (>93%) at rest and at peak exercise and resolution of polycythemia (hemoglobin concentration ≤16 g/dl) during subsequent follow-up.
Descriptive variables and statistical tests were performed in SPSS for Windows version 14 (SPSS, Inc., Chicago, Illinois). Two-tailed Student’s t test of paired samples was used to compare oxygen saturation and hemoglobin concentration before and 6 months after baffle leak closure. Significance was taken at p <0.05.
Procedures were performed under general anesthesia having obtained written consent. Transesophageal echocardiography and biplane fluoroscopy were used to guide closure in all patients. Vascular access was obtained from the right internal jugular vein, the right brachial vein, or the right femoral vein depending on the position of the baffle leak. Heparin (100 U/kg) was given after access was obtained. After the collection of hemodynamic data, angiography of the systemic venous baffle was performed using a pigtail catheter. Additional interrogation of baffle leaks using balloon sizing was performed when necessary (Meditech balloon over a 0.035-inch Amplatzer super-stiff exchange wire; Boston Scientific Corporation, Natick, Massachusetts). Two closure techniques were used depending on location of the lesion and whether there was concomitant baffle obstruction. In the absence of baffle stenosis, leaks were closed with an Amplatzer septal occluder (ASO; AGA Medical, Plymouth, Minnesota) sized with transesophageal echocardiography and delivered through a torque-view sheath. One leak early in the experience was closed using a Rashkind device (Bard, Tewkesbury, Massachusetts). Baffle leaks associated with baffle limb stenosis were approached from either the right internal jugular or the femoral vein. Covered CP Stents (length 34 to 45 mm; NuMED, Inc., Toronto, Ontario, Canada) mounted on Cristal balloons (Balt, Montmorency, France) appropriately sized to the vessel proximal to the stenosis were positioned. High-pressure postdilation using a Mullins balloon (NuMED, Inc.) or deployment of a second stent was performed when necessary.
Results
Transcatheter closure of 15 baffle leaks (7 in the inferior limb, 8 in the superior limb) was performed in 11 patients (6 of whom had undergone previous Mustard and 5 previous Senning procedures). Nine leaks were closed with ASOs, 1 with a Rashkind umbrella device, and 5 using Covered CP Stents.
Procedural data are listed in Table 1 . The average age at the time of the procedure was 26 years (range 6 to 42). Median procedure time was 100 minutes (range 34 to 210), fluoroscopy time 14.2 minutes (range 6.8 to 67.2), and radiation dose 5,560 Gy/cm 2 (range 2,930 to 26,840). Of the 9 Amplatzer devices placed, the mean size was 14 mm (range 6 to 22; see Table 1 ). Successful closure on angiography and transesophageal echocardiography was achieved in 14 of 15 leaks.
| Patient | Age (years) | Surgery | Limb | Device 1 | Device 2 | Sheath Size (Fr) | Dose (Gy/cm 2 ) | Procedure Time (minutes) | Fluoroscopy Time (minutes) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 25 | Mustard | Inferior | 20-mm ASO | 12 | 5,450 | 65 | 14.2 | |
| 2 | 26 | Mustard | Superior | 22-mm ASO | 12 | 2,930 | NA | 7.4 | |
| 3 | 23 | Senning | Inferior | 12-mm ASO | 12 | 11,070 | 120 | 23.6 | |
| 4 | 31 | Mustard | Superior | 12-mm ASO | 14-mm ASO | 8 | 5,220 | 34 | 6.8 |
| 5 | 33 | Mustard | Inferior | 10-mm ASO | 34-mm CCP | 12 | 26,840 | 210 | 67.2 |
| 6 | 21 | Senning | Inferior | 45-mm CCP | 12 | 5,400 | 71 | 7.7 | |
| 7 | 29 | Mustard | Inferior | 39-mm CCP | 12 | 6,300 | NA | 14.3 | |
| 8 | 6 | Senning | Inferior | 17-mm Rashkind | 11 | NA | NA | 14.5 | |
| 9 | 42 | Senning | Superior | 39-mm CCP | 45-mm CCP | 14 | 20,280 | 152 | 16.2 |
| 10 | 25 | Senning | Inferior | 14-mm ASO | 8 | 5,560 | 45 | 16.8 | |
| 11 | NA | Mustard | Superior | 6-mm ASO | 14-mm ASO | 12 | NA | NA | NA |
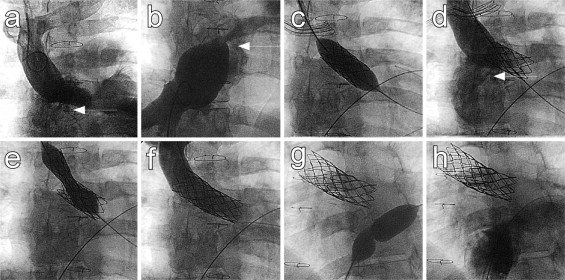
Of the 4 patients with stenosis of the systemic venous baffle limbs (patients 5 to 7 and 9; Figure 1 ) patients 6 and 7 had stenosis and multiple baffle leaks of the superior and inferior limbs respectively, so the logical choice was to place a covered stent. Patient 9 also had multiple leaks of the superior limb that required 2 covered stents for successful occlusion ( Figure 1 ). In this patient, additional angioplasty of an obstructed inferior limb was also performed ( Figure 1 ). Patient 5 had a significantly stenosed superior limb and complete occlusion of the inferior limb. The inferior limb was decompressing to the pulmonary venous atrium through a large right-to-left shunt through a baffle leak. In this case, temporary balloon occlusion of the baffle leak revealed a large azygous vein. The superior limb stenosis was relieved using an uncovered CP Stent and the baffle leak closed using a 10-mm ASO device ( Figure 2 ).
Seven patients were significantly desaturated at rest before baffle leak closure, with a further 3 desaturated on a simple 6-minute outpatient walk test consistent with a periodic right-to-left shunt during minimal exertion ( Table 2 ; left and right atrial pressure measurements at cardiac catheterization and outpatient saturation measurements, median oxygen saturation level 80%, range 65% to 96%). In only 1 patient was the baffle leak entirely left to right (patient 4). There were corresponding elevations in hemoglobin concentrations in 7 patients, suggesting prolonged periods of desaturation (median hemoglobin concentration 19 g/dl, range 13.8 to 23). Consistent with clinically important polycythemia, 3 patients had episodes of gout before the procedure, which resolved after baffle leak closure. By 6 months, there was a significant improvement in saturation (median 97%, p <0.0001) and a significant reduction in hemoglobin concentration (median 14.8 g/dl, p <0.05). At 6-month follow-up after baffle leak occlusion, only 1 patient remained mildly desaturated on outpatient walk test, and this was associated with recurrence of baffle leak in the context of device embolization (patient 1, 92%). In a second patient, a follow-up walk test was not performed (clinical procedural success in 9 of 11 [81%]). Formal preprocedural exercise test data were available for 6 patients using a standard Bruce protocol on a treadmill ( Supplementary Table 1 ). Preprocedural and postprocedural data were collected on 2 patients. In both, the ability to exercise increased markedly from 6.35 and 4.46 to 12 and 9.06 minutes, respectively. In a further case (patient 5), exercise capacity improved from New York Heart Association class IV (wheelchair bound) to class II. This patient was profoundly cyanosed at rest (65%), with normal postprocedural saturation.



