Coronary artery disease promotes the development of atrial fibrillation (AF). The aim of this study was to determine short- and long-term mortality in patients with acute coronary syndromes (ACS) and AF, depending on the AF presentation. A total of 2,335 consecutive patients with ACS were included. AF was classified as known persistent or permanent AF, known paroxysmal AF, new AF at admission, and new AF during hospitalization for ACS. Four hundred forty-two patients had any AF: 54 with known persistent or permanent AF, 150 with known paroxysmal AF, 54 with new AF at admission, and 184 with new AF during hospitalization. Statistically significant differences among subgroups related to previous heart failure (p <0.0001), stroke (p = 0.04), myocardial infarction (p <0.0001), angina pectoris (p <0.0001), hypercholesterolemia (p = 0.007), coronary artery bypass grafting (p <0.0001), and percutaneous coronary intervention (p = 0.03) were observed. Thirty-day mortality differed among the subgroups (p = 0.02) and was lowest in patients with known paroxysmal AF (7.3%). Ten-year mortality ranged from 53% to 78% among the subgroups. There were 5 predictors of long-term mortality across the subgroups: age (hazard ratio [HR] 1.06, 95% confidence interval [CI] 1.04 to 1.09, p <0.0001), previous myocardial infarction (HR 1.4, 95% CI 1.0 to 1.8, p = 0.04), heart failure (HR 1.8, 95% CI 1.3 to 2.4, p = 0.0002), diabetes (HR 1.7, 95% CI 1.2 to 2.2, p = 0.0005), and smoking (HR 1.7, 95% CI 1.2 to 2.3, p = 0.001). In conclusion, patient characteristics and 30-day mortality differed significantly among the subgroups, but long-term mortality did not. Any AF associated with ACS almost doubled the long-term mortality risk. AF in patients with ACS should therefore be regarded as an important risk factor irrespective of its presentation.
Atrial fibrillation (AF) may develop in connection with acute coronary syndromes (ACS), or ACS may occur in patients with AF. New AF may result in the deterioration of cardiac function and an increased risk for complications such as congestive heart failure, ventricular arrhythmias, cardiogenic shock, and reinfarction, while its effect on long-term prognosis has been less clear. Although underlying clinical risk factors such as previous or new heart failure, hypertension, diabetes, stroke, and age are well known to influence risk and prognosis in patients with AF, the potential role of the specific presentation of AF (i.e., previously known paroxysmal AF, persistent or permanent AF, or new AF at admission or during hospitalization for ACS) might be different. In this study, we aimed to investigate the role of different presentations of AF in association with ACS. We hypothesized that the short- and long-term mortality risk would differ in consecutive patients with ACS in relation to the presence and type of AF.
Methods
This study was a secondary analysis of a prospective cohort risk stratification study in patients with ACS (Prognosis and Risk of ACS in Sweden [PRACSIS]). In total, 2,335 patients with ACS were enrolled from September 15, 1995, to March 15, 2001. The study was approved by the ethics committee of the University of Gothenburg, and all patients gave informed consent to participate.
The diagnosis of ACS was based on chest pain or other symptoms suggestive of myocardial ischemia in combination with electrocardiographic changes, biochemical markers, or previously recognized coronary artery disease. Important exclusion criteria were age ≥80 years and life expectancy <1 year because of a condition other than coronary heart disease.
AF was defined as known or new. Known AF was classified as persistent or permanent AF or as paroxysmal AF and new AF as AF first detected on admission or during hospitalization. Absence of AF was defined as no history of AF and no AF on admission or during hospitalization. Survival status and dates of death as of January 1, 2007, were obtained from the Swedish National Population Registry, and the incidence of hospital admission for AF during follow-up (International Classification of Diseases, Ninth Revision, code 427D or International Classification of Diseases, 10th Revision, code I48) was obtained via linking to the National Swedish Diagnosis Registry for hospitalized patients. Ten patients were lost during follow-up because of emigration.
Data are presented as percentages, medians, or mean ± SD. The Cox proportional-hazards model in a forward stepwise mode was used to identify predictors of all-cause long-term mortality in the AF group. The following 15 variables were tested for inclusion in the model: age, gender, index diagnosis, peak creatine kinase-MB, smoking habits, and history of either myocardial infarction (MI), angina, heart failure, diabetes, hypertension, stroke, hypercholesterolemia, coronary artery bypass grafting, percutaneous coronary intervention, or valve surgery. A p value <0.05 was required for inclusion and retention in the model at each step in the selection procedure. All tests were 2 sided, and p values <0.05 were considered statistically significant for overall comparisons of the 4 AF groups. In addition, p values <0.01 were required for a difference to be considered significantly different in the pairwise 2-group comparisons regarding mortality during follow-up (using log-rank tests). Kaplan-Meier estimates were used to construct cumulative mortality.
Results
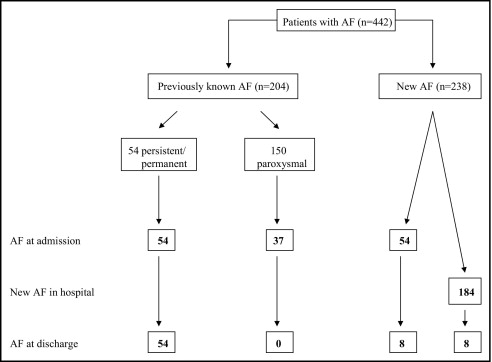
Altogether, 19% of the patients (n = 442) had known or new AF at or during hospitalization for ACS. Their mean age was 71 ± 8 years (range 67 to 76), and 32% were women. The patients without AF (n = 1,893) were younger, had a similar proportion of women, and had fewer co-morbidities than patients with AF ( Table 1 ). In 54 patients, AF had long been present and was classified as persistent or permanent ( Figure 1 ) . Of 150 patients with known paroxysmal AF, 37 had AF on admission that self-terminated so that they were in sinus rhythm at discharge. Another 54 patients had first documented AF on admission, and 8 of them remained in AF at discharge. Of patients without known AF and in sinus rhythm at admission, 184 had their first documented AF episodes during hospitalization, and 8 of them had AF at discharge.
| Variable | Patients Without AF (n = 1,893) | Previously Known AF | New AF | p Value ⁎ | ||
|---|---|---|---|---|---|---|
| Persistent or Paroxysmal | Permanent | On Admission | In Hospital | |||
| (n = 54) | (n = 150) | (n = 54) | (n = 184) | |||
| Age (years) (mean ± SD) | 64 ± 10 | 73 ± 5 | 71 ± 7 | 69 ± 8 | 70 ± 8 | 0.21 |
| Women | 30% | 22% | 34% | 28% | 35% | 0.29 |
| Previous heart failure | 8% | 39% | 35% | 15% | 9% | <0.0001 |
| Hypertension | 40% | 49% | 52% | 50% | 45% | 0.62 |
| Diabetes mellitus | 18% | 30% | 27% | 15% | 23% | 0.27 |
| Previous stroke | 7% | 20% | 16% | 8% | 9% | 0.04 |
| Previous MI | 24% | 30% | 42% | 35% | 19% | <0.0001 |
| Previous angina | 52% | 54% | 71% | 58% | 42% | <0.0001 |
| Previous hypercholesterolemia | 31% | 17% | 35% | 31% | 20% | 0.007 |
| Previous coronary artery bypass grafting | 9% | 7% | 19% | 19% | 4% | <0.0001 |
| Previous percutaneous coronary intervention | 9% | 4% | 11% | 11% | 4% | 0.03 |
| Previous valve surgery | <1% | 2% | 4% | 2% | 1% | 0.32 |
| Smoking | 31% | 24% | 18% | 28% | 29% | 0.12 |
| Admission and hospitalization | ||||||
| ST-segment elevation MI | 37% | 30% | 23% | 30% | 54% | <0.0001 |
| Non–ST-segment elevation MI | 32% | 43% | 46% | 56% | 33% | 0.008 |
| Unstable angina | 31% | 28% | 31% | 15% | 14% | 0.0004 |
| Maximum creatine kinase-MB (μg/L) (median) | 33 | 44 | 24 | 53 | 106 | <0.0001 |
| Killip class >1 at admission | 7% | 22% | 13% | 13% | 11% | 0.26 |
| Left ventricular ejection fraction (%) (median) | 55 | 45 | 52 | 45 | 47 | 0.01 |
| Thrombolysis | 14% | 17% | 9% | 9% | 22% | 0.005 |
| Primary percutaneous coronary intervention | 13% | 7% | 5% | 7% | 16% | 0.004 |
| Other percutaneous coronary intervention/coronary artery bypass grafting | 31% | 24% | 29% | 17% | 25% | 0.38 |
| Days in hospital (median) | 6 | 7 | 6 | 7 | 9 | <0.0001 |
| Ventricular arrhythmia | 24% | 37% | 23% | 39% | 45% | 0.0005 |
| Reinfarction | 1% | 0% | 3% | 0% | 6% | 0.07 |
| Cardiogenic shock | 3% | 8% | 2% | 6% | 5% | 0.12 |
| Stroke | 1% | 0% | 1% | 2% | 4% | 0.24 |
| Warfarin (at entry) | 2% | 41% | 18% | 8% | 4% | <0.0001 |
| Aspirin (at entry) | 36% | 33% | 55% | 55% | 31% | <0.0001 |
| Aspirin (hospital phase) | 93% | 64% | 76% | 77% | 83% | 0.04 |
| Warfarin (hospital phase) | 6% | 43% | 27% | 15% | 11% | <0.0001 |
⁎ For each of these variables, the p value indicates the significance of differences among the subgroups with AF.
Statistically significant differences among the AF subgroups were present regarding history of heart failure, stroke, MI, angina pectoris, hypercholesterolemia, coronary artery bypass grafting, and percutaneous coronary intervention ( Table 1 ). The highest proportion of heart failure was observed in patients with persistent or permanent AF (39%), while MI, angina pectoris, and hypercholesterolemia were more frequent in patients with known paroxysmal AF (42%, 71%, and 35%, respectively). The prevalence of previous stroke was highest in patients with persistent or permanent AF (20%) and lowest in those with new AF at admission (8%).
There were highly statistically significant differences among the AF subgroups in the proportions of ST-segment elevation MI (p <0.0001), non–ST-segment elevation MI (p = 0.008), and unstable angina (p = 0.0004) ( Table 1 ). Unstable angina was less common in patients with new AF than in patients with known AF or without AF. Patients with new AF during hospitalization differed from all other groups in that non–ST-segment elevation MI was least common and at the level of patients without AF, while ST-segment elevation MI was more common than in any of the other subgroups. Patients with new AF during hospitalization had the highest release of creatine kinase-MB, and the difference between subgroups was significant. Additional differences between the subgroups were found regarding ventricular arrhythmia during hospitalization (p <0.0001) and in the mean number of days in the hospital (p = 0.0005), with the longest duration observed in patients with new AF in the hospital.
A statistically significant difference among the AF subgroups was noted with respect to warfarin use at admission (p <0.0001; Table 1 ), which was most common in patients with known persistent or permanent AF, although only 41% of them were taking warfarin.
There was a significant difference among the subgroups regarding hospitalization with AF during the long-term follow-up (p = 0.01 for any difference), with the highest (55%) observed in those with new AF at admission ( Table 2 ). Almost 1/3 of patients with their detected AF during hospitalization were hospitalized with AF during follow-up. The hospitalization rate for AF in patients with known persistent or permanent AF was 16%.
| Variable | Patients Without AF (n = 1,893) | Previously Known AF | New AF | p Value ⁎ | ||
|---|---|---|---|---|---|---|
| Persistent or Permanent | Paroxysmal | At Admission | In Hospital | |||
| (n = 54) | (n = 150) | (n = 54) | (n = 184) | |||
| Hospitalization because of AF | 7.9% | 16.4% | 36.2% | 54.7% | 29.5% | 0.01 |
| All-cause mortality (actuarial) | ||||||
| Early (<30-day) mortality | 5.2% | 22.2% | 7.3% | 14.8% | 16.3% | 0.02 |
| Total 10-year mortality | 36.3% | 78% | 69% | 68.0% | 53.2% | 0.24 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


