The aim of this study was to compare the prognoses of patients with ST-segment elevation myocardial infarction (STEMI) and those with non-ST-segment elevation myocardial infarction (NSTEMI) without obstructive coronary artery disease (CAD) and the risk associated with gender for future cardiovascular events. The study population was selected from 95,849 patients who underwent coronary angiography for myocardial infarction from 2005 to 2010 and registered in the Swedish Coronary Angiography and Angioplasty Registry (SCAAR). Outcome analyses, including all-cause death, myocardial infarction, congestive heart failure, stroke, and revascularization, were performed in 2,268 patients with STEMI and 10,904 with NSTEMI without obstructive CAD (<50% stenosis). Hazard ratios and 95% confidence intervals comparing women with men were calculated for events, adjusting for cardiovascular risk factors and age. Nonobstructive CAD was found in 7% of patients with STEMI (6% men, 10% women) and in 17% of those with NSTEMI (11% men, 28% women). During a median follow-up of 2.6 years, 8% of patients with STEMI and 5% of those with NSTEMI died. Gender-associated differences in risk were observed in patients with NSTEMI, with adjusted hazard ratios lower in women than men for mortality (hazard ratio 0.90, 95% confidence interval 0.50 to 0.73) and congestive heart failure (hazard ratio 0.61, 95% confidence interval 0.52 to 0.72). In the 2 groups, women underwent less revascularization. In conclusion, nonobstructive CAD was more common in patients with NSTEMI than those with STEMI, as well as in women compared with men. Long-term mortality in patients with nonobstructive CAD was higher after STEMI than NSTEMI. The gender differences in outcomes suggest gender differences in the underlying pathogenesis of myocardial infarction without obstructive CAD.
In both ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (NSTEMI), coronary artery plaque rupture followed by intraluminal thrombosis is the principal pathophysiologic mechanism. However, in up to 30% of patients with acute coronary syndromes (ACS), neither thrombosis nor significant plaque burden is visible on coronary angiography. Many different causes have been proposed to explain myocardial infarction (MI) in the setting of nonobstructive coronary artery disease (CAD). Prognosis in nonobstructive CAD by MI type is an understudied area. Gender is an important aspect with regard to nonobstructive CAD, as most of these patients are women. The aim of this study was therefore to compare the prognosis of patients with STEMI with that of patients with NSTEMI without obstructive CAD. Furthermore, we investigated whether the risk for future cardiovascular events in these patients differs by gender.
Methods
The study population was composed of patients who underwent coronary angiography for the first time and were registered in the Swedish Coronary Angiography and Angioplasty Registry (SCAAR) from 2005 to 2010. SCAAR is a national registry containing medical data on consecutive patients from all hospitals in Sweden that perform coronary angiography. Patients with MI who did not undergo coronary angiography were not included. Three patient cohorts were studied, all of which fulfilled the inclusion criteria of nonobstructive CAD (defined as <50% luminal narrowing in any epicardial coronary artery) and no previous diagnosis of CAD (i.e., MI, percutaneous coronary intervention, or coronary bypass surgery), congestive heart failure (CHF), or valvular disease. Patients with MI included all patients presenting with signs and symptoms suggestive of ACS. Patients were further classified by electrocardiographic findings at presentation as having either ST-segment elevation, including left bundle branch block (n = 2,268), or non-ST-segment elevation (n = 10,904). Patients with stable chest pain included those referred for elective coronary angiography to rule out CAD (n = 11,127).
Information on risk factors was obtained through SCAAR. Hypertension and hyperlipidemia were defined as current use of medical therapy. The definition of diabetes included diet and medical treatment. Co-morbidities and outcome measures, including in-hospital events, were attained by merging the SCAAR database with the national patient registry, which includes information on hospitalization and discharge diagnoses classified according to the International Classification of Diseases, 10th Revision. Outcomes included all-cause death, MI, revascularization (percutaneous coronary intervention, coronary artery bypass grafting), CHF, and stroke from 2005 to 2010. Death included in-hospital mortality, whereas other events were after hospital discharge. The use of International Classification of Diseases coding did not allow the differentiation of systolic versus diastolic CHF. The time frame for the survival analysis was defined as the time from the date of inclusion (i.e., coronary angiography) to a first event followed by all-cause mortality.
Because all data in the respective national registries are anonymized, written informed consent from each patient was not needed. The study complied with the Declaration of Helsinki and was approved by the local research ethics board.
Background characteristics are reported as counts, percentages, or medians. Proportions were tested with chi-square tests and medians with Mann-Whitney U tests. For each patient cohort, Kaplan-Meier survival curves were calculated for each event, and comparison between groups was performed using log-rank statistics. The relation between gender and outcome was examined using Cox proportional hazards analysis and was performed on the cohort of patients for whom no data for the covariates studied were missing (1,856 patients with STEMI, 8,732 with NSTEMI, and 8,928 with chest pain). Covariates adjusted for in the model were clinically relevant and statistically significant and included age, hypertension, hyperlipidemia, diabetes, smoking, and cancer. The Cox proportional hazards model was used to calculate hazard ratios (HRs) and 95% confidence intervals. Interaction analyses were performed for each event for group and gender. All statistical analyses and graphics were done using R version 3.0.2 (R Foundation for Statistical Computing, Vienna, Austria). The Cox regression was done with the survival package of the R version. All reported p values are 2 sided. A p value <0.05 was considered to indicate statistical significance in all analyses.
Variables used in the modeling with more than about 5% missing or unknown values were smoking (21% to 27%) and, for women with STEMI, hyperlipidemia (6%). Because “unknown” values are generally considered different from systematically missing values and because we were not interested in the effects of these covariates, these values were simply kept as an additional level of the categorical covariates. Sensitivity analysis was performed by adjusting the model to equate unknown and missing values and by imputing the missing values. Such variations did not alter the estimated effect of gender (i.e., HR) in any significant way.
Results
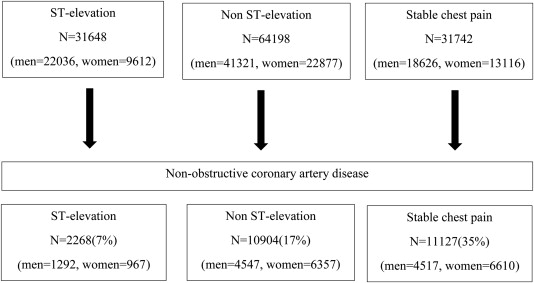
The total number of women and men who underwent coronary angiography from 2005 to 2010 for STEMI, NSTEMI, and chest pain and the proportion of patients with nonobstructive CAD are illustrated in Figure 1 . Nonobstructive CAD was more common in patients with NSTEMI compared with those with STEMI and in women compared with men.
Patients’ baseline characteristics are listed in Table 1 . The STEMI population was younger than the NSTEMI population. With the exception of smoking, cardiovascular risk factors (i.e., hyperlipidemia, hypertension, and diabetes) were less prevalent in the STEMI population. Hypertension and chronic obstructive pulmonary disease were more prevalent in women in the 2 MI populations, and women were also older than the men in these populations. More men than women were former smokers. A previous diagnosis of cancer was equally frequent in the STEMI and NSTEMI populations.
| Variable | ST-elevation | Non-ST-elevation | Chest pain | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Men (N=1292) | Women (N=976) | p ∗ | Men (N=4547) | Women (N=6357) | p ∗ | Men (N=4517) | Women (N=6610) | p ∗ | |
| Age, years (SD) | 56.6(13.9) | 66(12.2) | <0.001 | 59.9(11.9) | 66(10.9) | <0.001 | 60.3(10.6) | 62(9.9) | <0.001 |
| Smoker | |||||||||
| -Current | 231(18%) | 152(16%) | 0.19 | 721(16%) | 781(12%) | <0.001 | 421(9%) | 525(8%) | 0.005 |
| -Former | 274(21%) | 145(15%) | <0.001 | 1216(27%) | 1300(20%) | <0.001 | 1405(31%) | 1504(23%) | <0.001 |
| Diabetes Mellitus | 113(9%) | 84(9%) | 0.97 | 562(12%) | 638(10%) | <0.001 | 645(14%) | 758(12%) | <0.001 |
| Hyperlipidemia | 144(11%) | 116(12%) | 0.63 | 1527(34%) | 2324(37%) | 0.001 | 2299(51%) | 3331(50%) | 0.58 |
| Hypertension | 298(23%) | 367(38%) | <0.001 | 1812(40%) | 2926(46%) | <0.001 | 2248(50%) | 3559(54%) | <0.001 |
| Stroke | 24(2%) | 60(6%) | <0.001 | 166(4%) | 264(4%) | 0.2 | 142(3%) | 174(3%) | 0.12 |
| Chronic obstructive pulmonary disease | 61(5%) | 104(11%) | <0.001 | 321(7%) | 713(11%) | <0.001 | 218(5%) | 411(6%) | 0.002 |
| Kidney failure | 7(<1%) | 7(<1%) | 0.80 | 47(1%) | 43(<1%) | 0.054 | 33(<1%) | 31(<1%) | 0.096 |
| Cancer | 37(3%) | 29(3%) | 0.98 | 125(3%) | 188(3%) | 0.56 | 109(2%) | 108(2%) | 0.004 |
| Peripheral artery disease | 15(1%) | 9(<1%) | 0.73 | 67(2%) | 77(1%) | 0.27 | 67(2%) | 83(1%) | 0.35 |
| Follow-up, years | 2.5 | 2.4 | 0.86 | 2.6 | 2.7 | 0.24 | 2.7 | 2.8 | 0.016 |
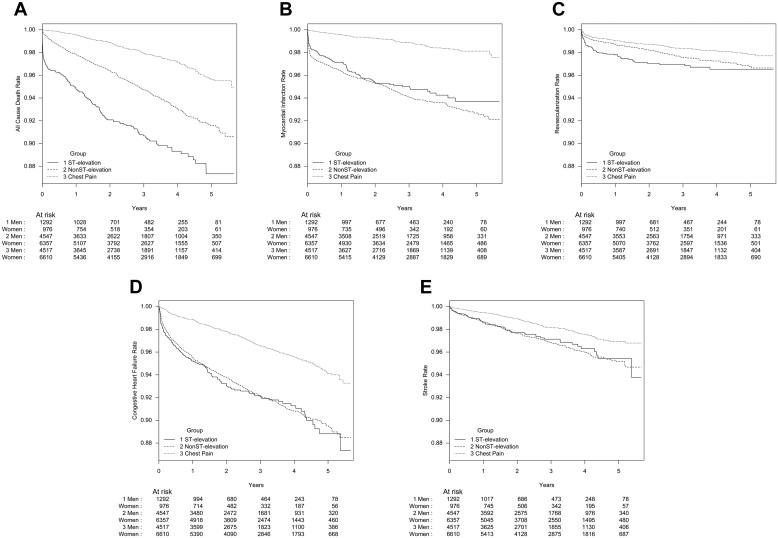
The median follow-up time was 2.6 years. Survival curves for the different events are shown in Figure 2 . Death occurred in 8% of patients with STEMI, 5% of those with NSTEMI, and 2% of those with chest pain. The event rates per 100 patient-years were 3.4 for STEMI, 1.9 for NSTEMI, and 0.7 for chest pain. Crude all-cause mortality rates were significantly higher in patients with STEMI than in those with NSTEMI (p <0.00001; Figure 2 ). For all-cause mortality, a significant interaction was found between groups and gender (p <0.0001), with higher rates observed for women than for men with STEMI. After adjustment, the HR for all-cause mortality did not differ for women compared with men with STEMI, whereas the HR in the NSTEMI and chest pain populations was lower in women ( Figure 3 ).