Cardioselective β blockers are considered to have little impact on lung function at rest in patients with chronic obstructive pulmonary disease (COPD). However, their effects on dynamic hyperinflation, an important mechanism contributing to symptoms and exercise tolerance in patients with COPD, have not been evaluated. Twenty-seven patients with moderate to severe COPD (forced expiratory volume in 1 second 52 ± 13% predicted) completed pulmonary function tests, echocardiography, maximal exercise tests, and cycle endurance tests at baseline. Inspiratory capacity was measured at 2-minute intervals during the cycle endurance test to quantify dynamic hyperinflation. Pulmonary function and cycle endurance testing were repeated after 14 days of bisoprolol 10 mg/day and 14 days of placebo in a randomized, double-blind, placebo-controlled, crossover trial. The extent of dynamic hyperinflation at peak isotime exercise with bisoprolol and placebo was compared. Peak isotime was defined as the latest time point that was reached during the 2 cycle endurance tests. Changes in inspiratory capacity from rest to peak isotime were different with bisoprolol compared to placebo (−0.50 ± 0.35 vs −0.41 ± 0.33 L, p = 0.01). Exercise duration tended to be lower with bisoprolol compared to placebo (305 ± 125 vs 353 ± 172 seconds, p = 0.11). The magnitude of change in exercise duration between the bisoprolol and placebo conditions was correlated with the magnitude of change in inspiratory capacity (r = 0.57, p <0.01). In conclusion, bisoprolol was associated with modest worsening dynamic hyperinflation, whereas exercise duration remained unchanged in patients with moderate to severe COPD. The magnitude of these effects was small and should not contraindicate the use of bisoprolol in patients with COPD.
The prevalence of chronic obstructive pulmonary disease (COPD) is high in patients with ventricular dysfunction or heart failure. The number of patients with COPD with a concomitant cardiac disease who could benefit from the use of β blockers is significant. However, cardiologists and respirologists are often reluctant to use β blockers in patients with COPD because of safety concerns, despite a recent Cochrane review concluding that cardioselective β blockers do not influence lung function at rest in patients with COPD. This practice, which may negatively affect long-term outcomes in patients with COPD with concomitant heart disease, is likely related to the fact that symptoms in patients with COPD are more related to exercise-induced increases in operating lung volumes (i.e., dynamic hyperinflation) than to lung function at rest. Similarly, the reduction in dynamic hyperinflation during exercise is responsible for the improvement in dyspnea associated with bronchodilation. Importantly, the impact of cardioselective β blockers on dynamic hyperinflation and exercise capacity in patients with COPD remains unknown.
The aim of this study was to assess the effect of a cardioselective β blocker, bisoprolol, on dynamic hyperinflation in patients with moderate to severe COPD using a randomized, double-blind, placebo-controlled, crossover trial. We hypothesized that bisoprolol would worsen dynamic airway function and decrease exercise capacity in COPD despite exerting little or no effect on forced expiratory volume in 1 second (FEV 1 ) at rest. We also hypothesized that changes in endurance time would be related to changes in dynamic hyperinflation induced by bisoprolol.
Methods
Consecutive patients with COPD were recruited from the COPD clinic of Institut Universitaire de Cardiologie et de Pneumologie de Québec. Inclusion criteria were (1) age >50 years, (2) cigarette exposure >10 pack-years, (3) stable condition with no respiratory exacerbation over a 4-month period preceding the study, and (4) moderate to severe COPD (FEV 1 30% to 80% of predicted with FEV 1 /forced vital capacity <70%). Exclusion criteria were (1) long-term oxygen therapy or arterial oxygen saturation at rest <85%, (2) known coronary artery disease or other medical condition requiring treatment with β blockers, (3) a left ventricular ejection fraction <40%, (4) current treatment with oral corticosteroids, (5) a medical condition other than COPD influencing exercise capacity, (6) baseline heart rate <60 beats/min, and (7) blood pressure <110/60 mm Hg. Patients’ regular respiratory medications, including long acting β 2 agonists (n = 7), methylxanthine (n = 1), muscarinic receptor antagonists (n = 17), and inhaled corticosteroids alone (n = 1) or in combination with long-acting β 2 agonists (n = 16), were maintained throughout the study. This protocol was approved by the scientific and ethic committees of our institution (Comité d’Éthique IUCPQ, CÉR 20300), and each patient signed an informed consent form before enrollment.
Lung volumes, carbon monoxide diffusion capacity, and spirometry were measured (Vmax Spectra; SensorMedics, Yorba Linda, California) according to guidelines. Individual results were compared to the predicted values. FEV 1 was measured before and 20 minutes after the inhalation of salbutamol 400 μg using a metered-dose inhaler.
Echocardiography (Sonos 5500; Phillips Medical Systems, Andover, Massachusetts) was performed in each patient by the same cardiologist (M.S.). Recordings were analyzed using an off-line quantification system. Measurements were made on 3 representative beats, and results were averaged. Maximal tricuspid regurgitant jet velocity, right ventricular index of myocardial performance, tricuspid annular plane systolic excursion, the left ventricular ejection fraction, cardiac output, valvular abnormalities, and left ventricular filling pressures were measured. Systolic pulmonary artery pressure was estimated using the maximal tricuspid regurgitant jet velocity according to the Bernoulli equation, and results were compared to reference values.
Patients then performed an incremental cardiopulmonary cycle exercise test according to the latest guidelines. Patients were seated on an electromagnetically braked cycle ergometer (Corival; Lode BV, Groningen, The Netherlands) and connected to the respiratory circuit through a mouthpiece (Vmax Spectra). After 2 minutes of rest followed by 2 minutes of unloaded pedaling, a ramp protocol was used, with increments of 5 to 20 W/min according to the patient’s fitness level until volitional exhaustion. Pulmonary gas exchange and ventilatory variables were obtained breath by breath throughout the protocol. Heart rate and oxygen hemoglobin saturation were continuously monitored using an electrocardiograph (Cardiosoft; Corina, Milwaukee, Wisconsin) and a pulse oximeter (Nellcor N-395; Covidien, Boulder, Colorado), respectively, whereas blood pressure was automatically monitored every 2 minutes (STBP-780; Colin Medical Instruments Corporation, San Antonio, Texas).
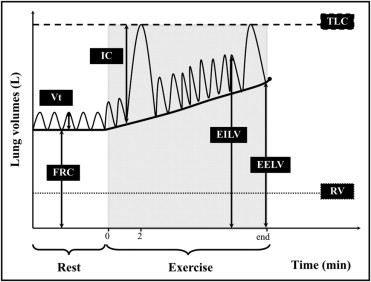
After 2 hours of rest, patients were positioned on the same ergometer to perform a cycle endurance test. This test served as a familiarization test. Patients were continuously monitored, as for the incremental test. At rest, patients completed ≥3 inspiratory capacity (IC) maneuvers. Values within 10% or 150 ml of the largest acceptable IC were considered reproducible. Then, after 2 minutes of unloaded pedaling, the workload was set at 75% of peak workload achieved during the incremental maximal cardiopulmonary exercise test. Patients were initially asked to maintain cycling until exhaustion, but no encouragements were provided during this test. Measurements of dynamic IC were made every 2 minutes and at end-exercise as previously described. Assuming a constant total lung capacity at rest and during exercise, changes in IC were used to derive changes in operational lung volumes during the cycle endurance test ( Figure 1 ) . Also, blood pressure was monitored, and symptoms of breathlessness as well as leg fatigue were assessed using the Borg scale at 2-minute intervals and at end-exercise. Endurance time was defined as the total exercise duration until exhaustion excluding the unloaded pedaling time.
Patients were randomized to receive daily bisoprolol or matching placebo of identical appearance for 14 days. Bisoprolol was initiated at a dose of 2.5 mg/day for 2 days and up-titrated to 5 mg/day for 2 days. A nurse who was not otherwise involved in the study then ensured that heart rate and blood pressure remained >60 beats/min and >110/60 mm Hg, respectively. Vital signs were not divulgated to patients unless abnormal. The dose was then up-titrated to 10 mg/day for the subsequent 10 days. Patients then performed pulmonary function tests at rest and symptom-limited cycle endurance tests including IC maneuvers as described previously. Each subject was then crossed over to the alternative treatment for an additional 14-day period before pulmonary function tests at rest and symptom-limited cycle endurance tests were repeated. The up-titration procedure was similarly done for the active medication and placebo. To ensure maximal bronchodilation during exercise, inhaled salbutamol 400 μg was given before exercise tests. All assessments were made at the same time of the day, and patients and exercise technicians were blinded to patients’ medications as well as heart rates and oxygen pulses throughout the cycle endurance tests.
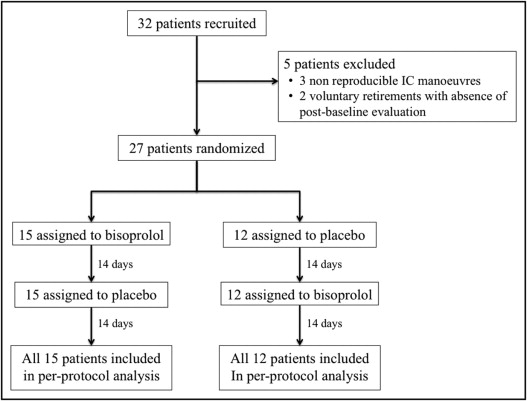
The primary outcome of interest was the difference in dynamic hyperinflation, defined as the difference in IC between rest and the latest time point that was reached during the 2 cycle endurance tests (peak isotime) (ΔIC rest-peak isotime ). Patients with nonreproducible IC maneuvers at baseline or without postbaseline assessments were excluded from the analysis. The secondary outcomes of interest were differences in cycle endurance test duration and pulmonary function at rest between the bisoprolol and placebo treatment arms. Difference in dynamic hyperinflation, endurance time, and lung function at rest were assessed using a crossover statistical analysis, corrected for baseline rest values (covariate). Normality and variance assumptions were verified using the Shapiro-Wilk and Brown-Forsythe tests, respectively. Results are expressed as mean ± SD unless specified otherwise. Pearson’s correlation was performed to examine the relation between changes in ΔIC rest-peak isotime and changes in cycle endurance test duration between the placebo and bisoprolol phases. A statistical level of significance of 0.05 was used. All analyses were run blinded using SAS version 9.2 (SAS Institute Inc., Cary, North Carolina). Bronchodilators have been associated with changes in peak isotime IC averaging 0.20 L in patients with COPD. Assuming a mean difference in IC of 0.20 ± 0.24 L between the treatment and placebo arms and a dropout rate of 25%, 32 subjects were necessary to detect a significant treatment effect with type 1 error of 5% and type 2 error of 20%.
Results
A total of 32 patients were recruited from June 2008 to September 2010 ( Table 1 ). Five patients were excluded from the analysis ( Figure 2 ) . Mild (n = 16) or moderate (n = 6) left ventricular diastolic dysfunction as well as mild pulmonary hypertension (n = 3) were observed on Doppler echocardiography study. Bisoprolol and matching placebo were progressively up-titrated to 10 mg/day in all 27 patients without significant bradycardia or hypotension.
| Characteristic | Value | % Predicted Values |
|---|---|---|
| Age (years) | 65 ± 8 | |
| Women/men | 10/17 | |
| GOLD stage II/III | 17/10 | |
| Body mass index (kg/m 2 ) | 27 ± 5 | |
| FEV 1 (L) | 1.40 ± 0.45 | 52 ± 13 |
| Forced vital capacity (L) | 3.41 ± 0.95 | 101 ± 15 |
| FEV 1 /forced vital capacity (%) | 42 ± 11 | |
| Total lung capacity (L) | 6.65 ± 1.52 | 111 ± 13 |
| Functional residual capacity (L) | 4.29 ± 1.27 | 133 ± 31 |
| Diffusing capacity of the lungs for carbon monoxide (mL · mm Hg −1 · min –1 ) | 14 ± 5 | 58 ± 16 |
| Peak work rate (W) | 91 ± 34 | 68 ± 20 |
| Peak oxygen consumption (ml · kg −1 · min −1 ) | 18.5 ± 4.7 | 79 ± 26 |
| Ejection fraction (%) | 59 ± 7 | |
| Tei index | 0.54 ± 0.17 | |
| Systolic pulmonary arterial pressure (mm Hg) | 37 ± 5 | |
| Tricuspid annular plane systolic excursion (mm) | 23 ± 5 | |
| Tricuspid annular plane systolic excursion (cm/s) | 13.6 ± 2.3 |
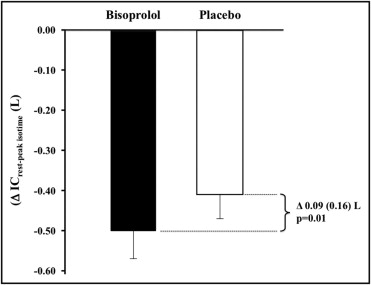
IC significantly decreased during exercise from 2.51 ± 0.59 to 2.01 ± 0.62 L (p <0.01) (ΔIC rest-peak isotime 0.50 L) in the bisoprolol arm and from 2.48 ± 0.56 to 2.07 ± 0.65 L (p <0.01) (ΔIC rest-peak isotime 0.41 L) in the placebo arm for a difference of 0.09 ± 0.16 L (p = 0.01) between the 2 conditions ( Figure 3 ) . Rest lung volumes, expiratory flows, and other parameters related to dynamic hyperinflation were not significantly changed with bisoprolol compared to the placebo condition ( Table 2 ). Bisoprolol was associated with lower oxygen consumption, heart rate, and blood pressure and higher oxygen pulse at peak isotime compared to placebo, whereas no differences were noted in respiratory exchange ratio, minute ventilation, and Borg scale ( Table 2 ). No sequence, time, or carryover effects were observed with any of the peak isotime parameters. Cycle endurance test duration was not significantly lower on bisoprolol ( Figure 4 ). The 95% confidence interval around the difference in cycle endurance test duration between the 2 treatments was within the suggested minimal clinically important difference for this specific variable (105 seconds) ( Figure 4 ). The magnitude of change in cycle endurance test duration between the bisoprolol and placebo conditions was correlated with the magnitude of change in IC at peak isotime (r = 0.57, p <0.01).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


