Fig. 5.1
Pericardial anatomy. Panel a: Pericardial fat pad on transthoracic echocardiogram in the parasternal long-axis view. Note the heterogeneous appearance of the two layers of pericardial fat (arrows); one layer is intrapericardial (epicardial; #1), and the other is extrapericardial (mediastinal; #2). Panel b: Transesophageal echocardiogram demonstrates effusion in the transverse sinus (arrow) of the pericardium adjacent to the ascending aorta. This finding should not be mistaken for a type A aortic dissection. Panel c: Transesophageal echocardiogram demonstrates effusion in the transverse sinus (arrows) of the pericardium adjacent to the left atrial appendage which is filled with dense spontaneous echo contrast (‘smoke’) in this patient with atrial fibrillation. Abbreviations: AV aortic valve, LA left atrium, LAA left atrial appendage, LV left ventricle, RV right ventricle
Intra vs Extrapericardial Structures: For a full understanding of pericardial physiology and pathology, it is important to recognize which cardiac structures are within and which are outside the pericardial sac. The proximal portions of the great vessels (the ascending aorta and the main pulmonary artery) are within the pericardial sac. Thus injuries or dissections of proximal portions of these vessels may lead to pericardial effusion. In contrast, superior portion of the left atrium and the ostia of the pulmonary veins are not within the pericardial sac. This anatomic fact contributes to exaggerated respiratory variations in tamponade and constrictive pericarditis as further discussed in appropriate sections of this chapter.
Pericardial Extensions: The main pericardial space communicates with several extensions referred to as sinuses and recesses. Transverse sinus (Fig. 5.1, Panels b, c) is located around the origins of the great vessels and the left atrial appendage while the oblique sinus surrounds the ostia of the pulmonary veins. Pericardial effusion may occasionally be restricted to one or more of these sinuses and recesses. These localized pericardial effusions should not be mistaken for other pathologies such as the type A aortic dissection in the case of fluid accumulation in the transverse sinus.
Congenital Absence of the Pericardium
Partial or complete absence of the pericardium is a rare congenital disorder that could not reliably be diagnosed in vivo prior to advent of modern cardiac imaging. Congenital absence of the pericardium was first undoubtedly described in 1793 on autopsy by the Scottish physician and pathologist Matthew Baillie (1761–1823) [5] although an earlier and likely erroneous description might have been made by the Italian anatomist Realdo Colombo (1516–1559) [6]. The reported occurrence of congenital absence of the pericardium is 1 per 14,000 autopsies [7].
Key Anatomic Features
Since partial absence of the pericardium surrounding the left heart is the most common form, excessive displacement of the cardiac apex to the left (levoposition and levorotation of the heart) is the key anatomic feature.
Echocardiography Indications
Congenital absence of the pericardium may be an incidental finding or the patient may present with nonspecific symptoms such as chest pain, palpitations or shortness of breath.
Echocardiography Findings
Echocardiographically, congenital absence of the pericardium cannot be visualized per se but is rather deduced from indirect signs. Because the cardiac apex is displaced laterally in the partially absent left-sided pericardium, standard echocardiographic imaging windows provide unusual images of the heart. In the parasternal views, the right ventricle, although typically normal in size, appears enlarged. Additionally, there is increased cardiac motion due to absence of pericardial constraint and paradoxical interventricular septal motion (Fig. 5.2, Panel a). On the apical 4-chamber view the cardiac apex is displaced to the left and the heart has an unusual tear-drop shape.
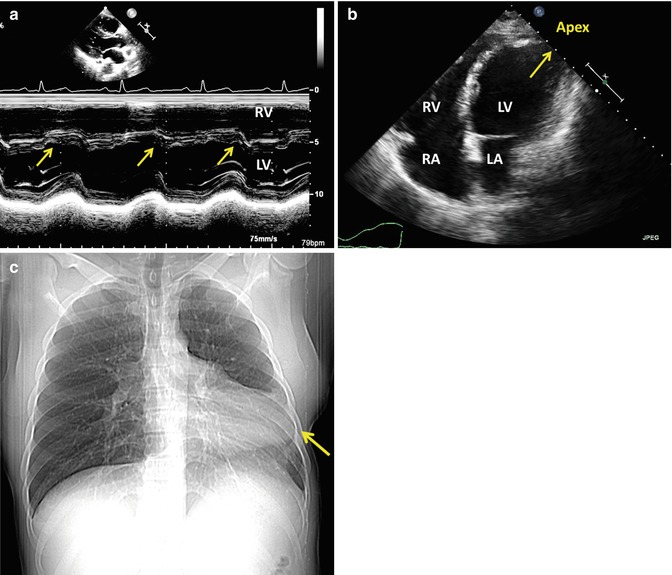
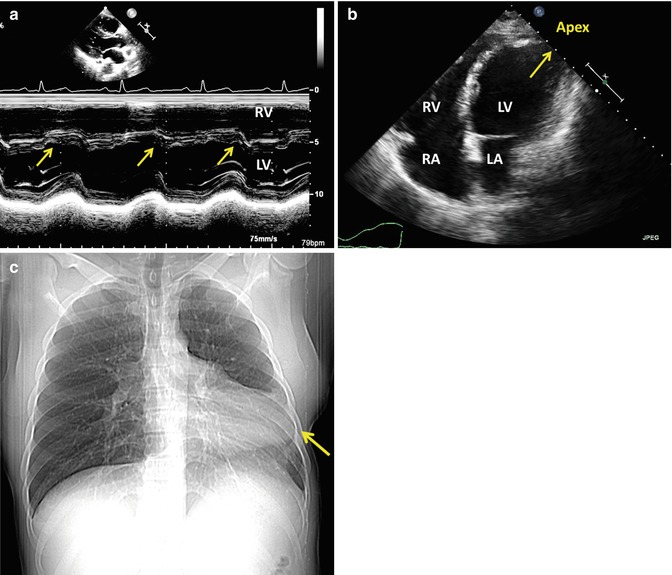
Fig. 5.2
Absence of the pericardium. Panel a: M mode recording shows paradoxical interventricular septal motion (arrow) in a patient with congenital absence of the pericardium. Panel b: Transthoracic echocardiogram in the apical 4-chamber view demonstrates characteristic lateral displacement of the cardiac apex (arrow) in a patient with absent pericardium after surgical stripping (pericardiectomy). Panel c: Chest X ray demonstrates an unusual cardiac silhouette with lateral and cranial displacement of the cardiac apex (arrow) in a patient with congenital absence of the pericardium (Courtesy of Dr. Robert Donnino, Department of Radiology and Division of Cardiology, New York University Langone Medical Center). Abbreviations: LA left atrium, LV left ventricle, RA right atrium, RV right ventricle
Patients in whom the pericardium was surgically removed (Fig. 5.2, Panel b) may have echocardiographic findings similar to those in patients with congenitally absent pericardium (e.g. patients post pericardiectomy for constrictive pericarditis).
Alternative Imaging
Congenital absence of the pericardium may be suspected from an unusual shape to the cardiac silhouette on chest X ray (Fig. 5.2, Panel c). Definitive diagnosis of congenitally absent pericardium is usually established by CT or CRM.
Pericardial Cysts and Diverticula
Congenital pericardial cysts and diverticula may be considered as accessory pericardial spaces. Pericardial cysts are thin-walled unilocular structures filled with clear, watery fluid; they do not communicate with the pericardial sac. In contrast, pericardial diverticula are abnormal extensions that communicate with the main pericardial space.
In general, pericardial cysts are rare, typically benign and congenital in nature with a prevalence of 1 per 100,000 cases [8]. Congenital pericardial cysts arise from the primitive coelum, the progenitor of pericardial, pleural and peritoneal cavities. Their exact embryogenesis is uncertain. Acquired cysts, such as pericardial hydatid cysts, may be seen in parts of the world where parasitic infections with Echinococcus species are common. Like congenital cysts, hydatid cysts are filled with a watery fluid, thus the name (from Greek úδατίς; stem úδατιδ– meaning ‘a drop of water’).
Key Anatomic Features
Congenital pericardial cysts are typically located in one of the cardiophrenic angles, more often in the right than the left cardiophrenic angle. Their size varies from small fluid collection in the cardiophrenic angle to large masses filling the mediastinum.
Echocardiography Indications
Pericardial cysts and diverticula may be an incidental finding or the patient may present with nonspecific symptoms such as chest pain, palpitations or shortness of breath.
Echocardiography Findings
On ultrasound imaging, pericardial cysts were first characterized by M mode echocardiography in 1975 [9], and then by 2D echocardiography in 1983 [10]. The key echocardiographic findings of a pericardial cyst include an echo lucent, thin-walled structure located adjacent to the heart and above the diaphragm (most often in and around the right atrioventricular groove), filled with clear, stationary fluid and without obvious communications to any of the surrounding structures (Fig. 5.3, Panel a).
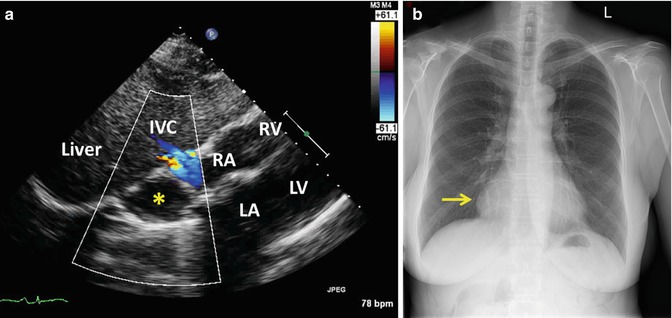
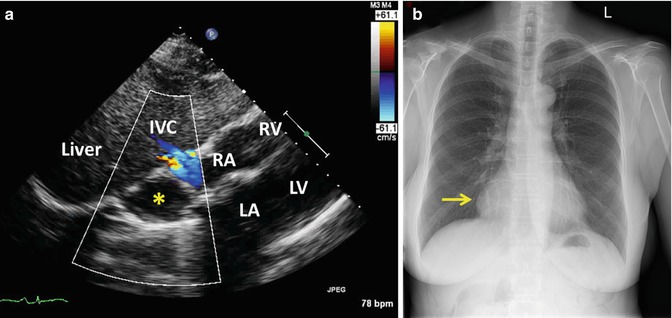
Fig. 5.3
Pericardial cyst. Panel a: Transthoracic echocardiogram in the subcostal view demonstrates a small pericardial cyst (asterisk) adjacent to the right atrium (RA). Abbreviations: IVC inferior vena cava, LA left atrium, LV left ventricle, RA right atrium, RV right ventricle. Panel b: Chest X ray demonstrates a pericardial cyst in the right cardiophrenic angle (arrow). Panel b: Chest X ray demonstrates a pericardial cyst in the right cardiophrenic angle (arrow) (Courtesy of Dr. Robert Donnino, Department of Radiology and Division of Cardiology, New York University Langone Medical Center)
Differential Diagnosis
Other echo lucent structures adjacent to the heart such as pericardial and pleural effusion or ascites may be mistaken for a pericardial cyst. Pericardial effusions tend to be circumferential and often show signs of organization. Unlike pericardial cysts, left and right pleural effusions follow the anatomic boundaries of respective pleural spaces.
Vascular anomalies (especially in and around atrioventricular grooves) such as coronary artery aneurysms, coronary artery fistulas and enlarged coronary sinus may be differentiated from pericardial cysts with the intravenous administration of echocardiographic contrast agents. Unlike vascular anomalies, pericardial cysts do not communicate with the vascular pool and thus they do not opacify after echocardiographic contrast administration. To differentiate pericardial cysts from coronary artery aneurysms and coronary artery fistulas, microbubble contrast agents (such as perflutrane) should be used while agitated saline can be used for the diagnosis of enlarged coronary sinus due to persistence of the left superior vena cava.
Alternative Imaging
The diagnosis of a pericardial cyst is often suspected on a chest X ray as a mass like density, typically located in the right cardiophrenic angle (Fig. 5.3, Panel b). The definitive diagnosis of pericardial cysts and diverticular is usually established by CT or CMR.
Pericardial Effusion
Pericardial effusion is an accumulation of fluid in the pericardial sac between the visceral and parietal layer of the pericardium. There are numerous causes of pericardial effusions including infectious, metabolic, rheumatologic, traumatic, neoplastic and idiopathic etiologies. In the developed countries, the predominant causes of pericardial effusion are idiopathic and traumatic (especially iatrogenic following surgical or percutaneous procedures).
The hemodynamic spectrum of a pericardial effusion spans from asymptomatic to tamponade, cardiovascular collapse and death.
Key Anatomic and Hemodynamic Features
The pericardial sac envelopes the entire heart except the cranial portion of the left atrium around the ostia of the pulmonary veins. The proximal portions of the ascending aorta and the main pulmonary artery are also within the pericardial sac. In contrast, the descending thoracic aorta lies outside the pericardial sac; this anatomic feature helps differentiate a pericardial effusion from a left pleural effusion (see below).
The primary determinant of hemodynamic significance of a pericardial effusion is not the volume of intrapericardial fluid per se but rather the intrapericardial pressure exerted by that volume. This is further discussed in the Tamponade section below.
Echocardiography Indications
Pericardial effusion may be an incidental finding on an echocardiogram ordered for a different reason, or the patient may present with chest pain, shortness of breath or hypotension and shock.
Echocardiography Findings
Here the general echocardiographic features of pericardial effusions will be discussed (Fig. 5.4). Tamponade findings are described separately in a section below.
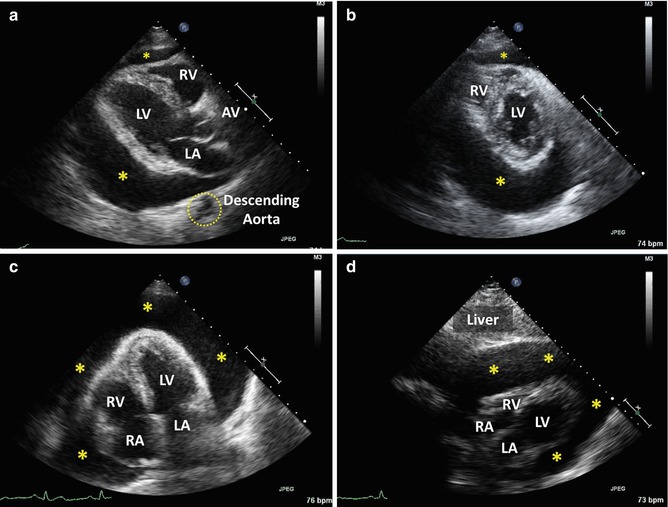
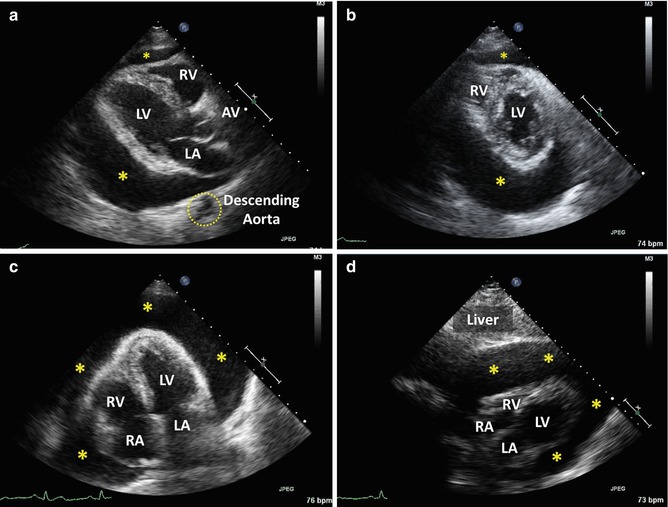
Fig. 5.4
Pericardial effusion. Transthoracic echocardiogram demonstrates a large pericardial effusion (asterisks) in a 47-year-old woman with breast cancer. Panel a: Parasternal long axis view demonstrates typical interposition of the pericardial effusion (asterisks) between the heart and the descending thoracic aorta. This finding differentiates a pericardial effusion from a left pleural effusion in which there is no such interposition between the heart and the descending thoracic aorta. Panel b: Parasternal short axis at the level of the papillary muscles demonstrates that the pericardial effusion (asterisks) is larger posterior to the left ventricle that anterior to the right ventricle. This is due to gravity in this supine patient. Panel c: In the apical 4-chamber view, note that the pericardial effusion (asterisks) surrounds the cardiac apex. This feature helps distinguish a pericardial effusion from a pleural effusion. Panel d: Subcostal view demonstrates a large pericardial effusion (asterisks). Abbreviations: AV aortic valve, LA left atrium, LV left ventricle, RA right atrium, RV right ventricle
Pericardial effusions are typically circumferential (around the entire heart) but not necessarily symmetrical; a larger amount of fluid tends to occur in more dependent areas compared to less dependent ones. In a supine patient, circumferential pericardial effusions tend to be larger posterior to the left heart than anterior to the right heart. Loculated pericardial effusions may occur in any portion of the pericardial sac.
The consistency of pericardial fluid varies from clear, water like collections to partly organized (with strands spanning the two layers of the pericardium) to fully organized, tumor like densities (as in the case of hemorrhagic effusion).
On an echocardiography report, the size, location (circumferential vs. loculated) and fluid characteristics (clear vs. organized) should be described. The size of a circumferential pericardial effusion may be expressed and the end-diastolic effusion thickness (the distance between epicardial and parietal layers of the pericardium). Small pericardial effusions have end-diastolic thickness of <1 cm; moderate between 1 and 2 cm; and large >2 cm as described in the latest ASE guidelines [2].
The volume of pericardial fluid can roughly be estimated using the so-called cube rule which assumes that the heart is a prolate ellipsoid and that a volume of a cardiac chamber is the cube of its short-axis diameter [11]. In practical terms, one obtains 2D echocardiographic images of the heart in the parasternal long or short axis and then measures the end-diastolic thickness of the pericardial fluid (PF), end-diastolic diameters of the left (LV) and right ventricles (RV), and end-diastolic thickness of the right ventricular free wall (RVF), interventricular septum (IVS) and inferolateral wall (IL).
The end-diastolic diameter of the heart is RVF + RV + IVS + LV + IL; this diameter cubed gives the volume of the heart. The end-diastolic diameter of the pericardial sac is the sum of anterior and posterior pericardial effusion thickness plus the end-diastolic diameter of the heart; the cube of the end-diastolic pericardial sac diameter represents the volume of the pericardial sec. The volume of pericardial effusion is then the difference between the pericardial sac volume and the volume of the heart.
Example:
The patient has a pericardial effusion that measures 1.0 cm both anterior to the right heart and posterior to the left heart at end diastole; RVF = 0.3 cm; RV = 1.7 cm; IVS = 0.7 cm; LV = 3.9 cm; IL = 0.6 cm.
Heart:
Pericardial sac:
Pericardial effusion:
It must be emphasized that this calculation method gives only a rough estimate of pericardial effusion volume and might overestimate effusion volume especially if cardiac diameters are large.
When pericardial effusions are very large, one may observe a swinging motion of the heart with the cardiac apex moving toward and then away from the anterior chest wall. In such instances, one may notice the electrical alternans (a change in QRS voltage) on simultaneous EKG tracings which should accompany any echocardiographic recording. Additionally, overall EKG voltage may be diminished [12].
Differential Diagnosis
Typically, the differential diagnosis of pericardial effusion includes pericardial fat, pericardial cyst, pleural effusion and ascites.
Pericardial fat is typically non-circumferential and most prominent along the right heart border; it is heterogeneous in appearance, and moves in concert with the heart (Fig. 5.1, Panel a). In contrast, pericardial effusion is typically echo lucent, immobile and circumferential with the largest amount of fluid in dependent areas closest to the ground.
Pericardial cysts are thin-walled structures containing clear, stationary fluid; they tend to occur in the right atrioventricular groove and have no direct communication with any surrounding structure (Fig. 5.3, Panel a).
Left pleural effusion is located posterior to the left ventricle on parasternal views or lateral to the left ventricle on apical views (Fig. 5.5, Panel a). To differentiate a left pleural effusion from a pericardial effusion, one should pay a special attention to the relationship between the descending thoracic aorta and the left heart border on e.g., parasternal views. The larger the pericardial effusion, the more separation between the descending thoracic aorta and the left heart border there is. In contrast, left pleural effusion does not create an echo lucent area of separation between the descending thoracic aorta and the heart. Because there is no communication between the left and right pleural spaces at the cardiac apex, periapical fluid collection seen on apical views are more likely to be pericardial than pleural in origin.
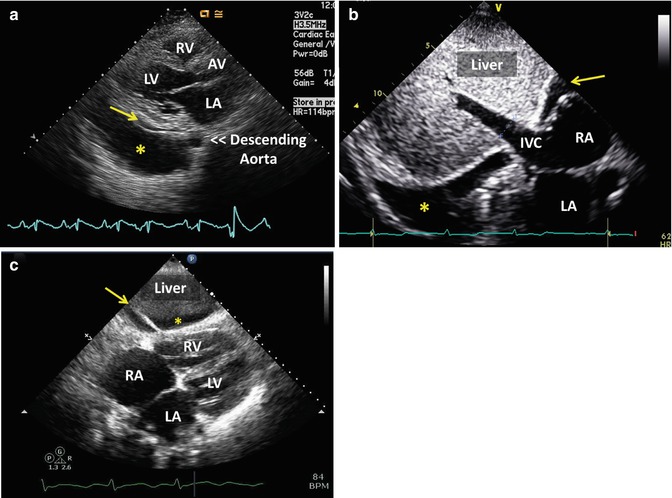
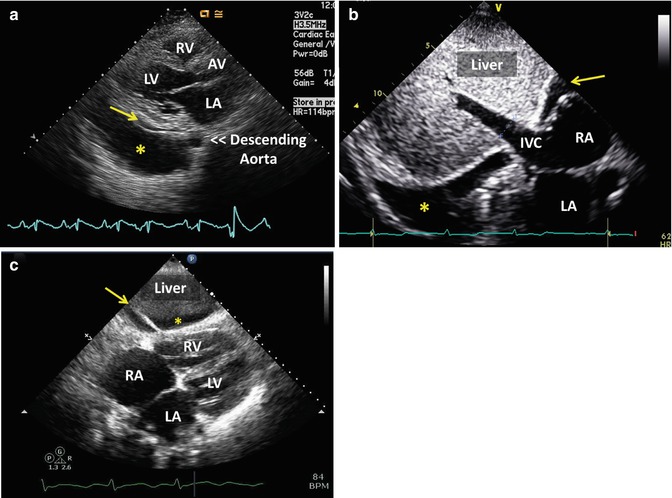
Fig. 5.5
Differential diagnosis of a pericardial effusion. Panel a: Left pleural effusion – Transthoracic echocardiogram in the parasternal long axis view demonstrates a left pleural effusion (asterisk) and a very small pericardial effusion (arrow). Note that unlike the pericardial effusion, the left pleural effusion does not create an echo lucent area of separation between the descending thoracic aorta and the heart. Panel b: Right pleural effusion – Transthoracic echocardiogram in the subcostal view demonstrates a left pleural effusion (asterisk) and a pericardial effusion (arrow). Note that the right pleural effusion follows the contours of the diaphragm which lies just cranial to the liver boundary. Panel c: Ascites – Transthoracic echocardiogram in the subcostal view demonstrates ascites (asterisk) between the liver and the heart. The presence of the falciform ligament (arrow) helps differentiate ascites from a pericardial effusion. Abbreviations: AV aortic valve, IVC inferior vena cava, LA left atrium, LV left ventricle, RA right atrium, RV right ventricle
Right pleural effusion is best differentiated from the pericardial effusion in the subcostal view; a right pleural effusion follows the contours of the diaphragm (Fig. 5.5, Panel b).
Ascites is a subdiaphragmatic fluid collection containing the falciform (sickle-shaped) ligament which anchors the liver to the diaphragm (Fig. 5.5, Panel c).
Alternative Imaging
Echocardiography is typically sufficient to establish the diagnosis and hemodynamic significance of a pericardial effusion.
Imaging with CT and CMR may provide additional anatomic details; particularly related to extracardiac structures and their relationship to pericardial effusion (e.g. type A aortic dissection, mediastinal hematoma post cardiac surgery, thoracic tumor extension into the pericardial space etc.).
EKG has low sensitivity for detection of pericardial effusion; low voltage and electrical alternans are seen only infrequently [12].
Tamponade
Tamponade, originally a French word meaning ‘plugging’, refers to a clinical syndrome of impaired cardiac filling due to elevation of intrapericardial pressure in the setting of a pericardial effusion. As a clinical entity, cardiac tamponade resulting from a pericardial effusion was first described in the 1930s [13].
Cardiac tamponade is a form of diastolic heart failure. It is important to emphasize that tamponade is not a discrete point in time but rather a process of progressive impairment in cardiac filling extending from an asymptomatic phase to exercise intolerance to hypotension, shock and death. An increase in intracardiac pressures and tachycardia are compensatory mechanisms that delay the progression of tamponade physiology.
Key Anatomic and Hemodynamic Features
The primary determinant of hemodynamic significance of a pericardial effusion is not the size of a pericardial effusion but rather the magnitude of intrapericardial pressure. Cardinal features of tamponade are cardiac chamber collapse (due to extrinsic compression of cardiac walls by pericardial effusion), ventricular interdependence (manifested as exaggerated respiratory variations in cardiac filling), and frequently intracardiac pressure elevation including right atrial pressure elevation leading to a plethoric inferior vena cava.
A normal intrapericardial pressure is close to 0 mmHg or even negative (subatmospheric). In tamponade, intrapericardial pressure exceeds intracardiac pressures for at least part of the cardiac cycle.
The intrapericardial pressure (P) is a product of intrapericardial volume (V) and pericardial stiffness (ΔP/ΔV):






Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree