4 Echocardiographic Parameters Important for Decision Making
Anatomic Imaging
LV Cavity Size and Systolic Function
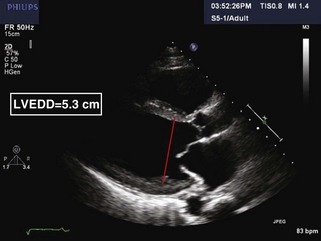
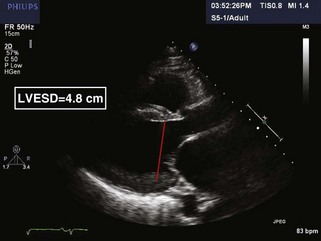
Step 1: Determination of LV Cavity Size by 2D Echocardiography in Parasternal Long-Axis View
• By convention, M-mode specifies that each point of the measurement be placed on the near edge (closest to the transducer) of the bright echo corresponding to the appropriate interface (“leading edge–to–leading edge” technique). For LV cavity measurements, these interfaces are located between the interventricular septum and the ventricular cavity and between the LV cavity and the posterior wall. While this technique has decades of data supporting its use, it gives information only along the lines that originate from the transducer. Unless the desired chamber size is exactly parallel to one of these lines, the measurements will overestimate the chamber sizes as compared with those obtained from 2D echocardiography. These differences are particularly notable in patients with “vertical” hearts (hearts with a more vertical axis in the parasternal long-axis view).
• 2D echocardiographic LV dimensions are measured at the interface between the bright myocardium and the echo-lucent cavity space. 2D imaging provides the flexibility of measuring along any line within the image plane. Improved image resolution and easier determination of precise timing during viewing have increased the use of 2D echocardiography for the determination of the same chamber measurements that can be obtained from M-mode. Measurements made from 2D echocardiography provide an accurate representation of the chamber size.
• In the parasternal long-axis view in either M-mode or 2D, LV dimension is obtained at end-diastole (LVEDD) and end-systole (LVESD) (Figures 4-1 and 4-2 and Table 4-1)
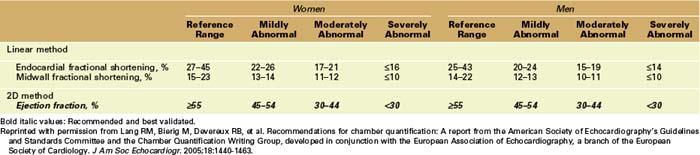
TABLE 4-1 RECOMMENDATIONS FROM THE AMERICAN SOCIETY OF ECHOCARDIOGRAPHY FOR THE QUANTIFICATION OF LEFT VENTRICULAR SIZE AND VOLUME

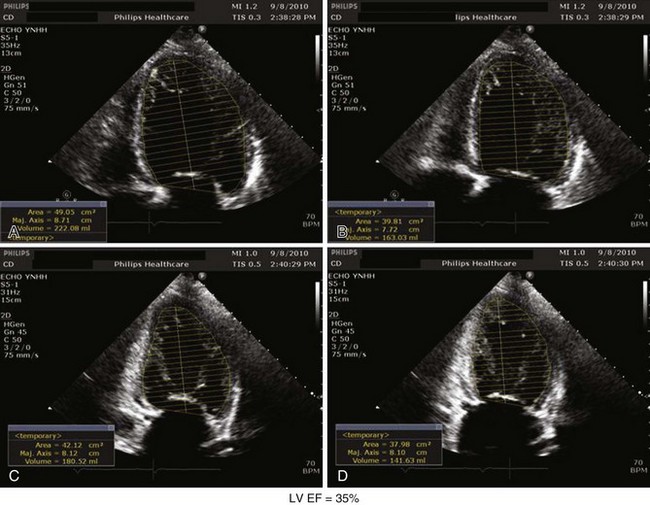
Step 2: Estimation of LV Volumes and EF by 2D by Simpson’s Method
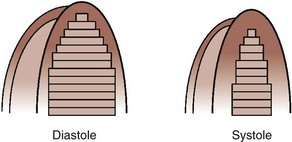
• By making the geometric assumption that the LV is a stack of thin disks (Figure 4-3), LV volumes can be estimated. Outlines of endocardial walls in 4-chamber (4C) and 2-chamber views are combined with a linear measurement of the long axis to create a stack of individual volumes of multiple “disks” within the LV cavity.
• In the apical 4C view, obtain an image optimizing visualization of the endocardial borders of the LV, paying particular attention to include the true apex. Next trace an outline of the endocardial walls of the LV still frame images at end-diastole and end-systole (Figure 4-4).
• Estimates of the LV volumes are made by combining measurements in both views at end-diastole and at end-systole. Most modern echocardiography machines contain software that automatically combines these measurements. Stroke volume (SV; difference between the LV end-diastolic volume and the LV end-systolic volume) and EF (SV divided by the LV end-diastolic volume) are then estimated (Table 4-2).
TABLE 4-2 RECOMMENDATIONS FROM THE AMERICAN SOCIETY OF ECHOCARDIOGRAPHY FOR THE QUANTIFICATION OF LEFT VENTRICULAR FUNCTION
Key Point
• Foreshortening of the apex may significantly underestimate LV volumes in both diastole and systole. Because EF is a relative estimation, the magnitude of the error on estimated LVEF is diminished. Thus, estimates of LVEF correlate with other modalities, such as cardiac magnetic resonance imaging (MRI), better than do estimates of SV, which is an estimation of an absolute value.
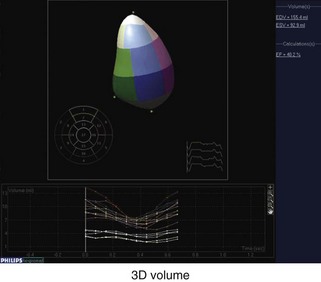
Step 3: Determination of Estimated LV Volumes and EF by 3D
• Images are obtained in the apical view. Current technology requires combining data from four cardiac cycles during a breath hold in order to obtain a full volume set.
• Although 3D echocardiography has been shown to estimate LV volume more accurately compared with MRI than does 2D echocardiography, care must still be taken to obtain images of the true apex for accurate volumes.
• In addition to estimated volume at end-diastole and end-systole only, volumes can be estimated at various points (typically 16 time points) throughout the cardiac cycle, enabling display of volume over time. The left ventricular cavity can be divided into 16 or 17 volumes corresponding the 16 or 17-wall-segment model and displayed over time (Figure 4-5).
Right Ventricle
Step 1: Determination of Right Ventricular Size by 2D
• Although a general sense of RV size can be obtained from the parasternal long- and short-axis views, because of the complex shape of the RV, neither definitive nor quantitative assessment of RV size is recommended in the parasternal view.
• The apical 4-chamber (4C) view provides a more complete and reliable perspective. Initially, a qualitative assessment is performed by noting RV apical location and overall size in comparison with the LV. The RV apex is normally closer to the base of the heart than the LV. With RV enlargement, the apex of the RV may be closer to or participate in forming part of the apex of the heart. Normally, the RV is approximately two-thirds the area of the LV in the 4C view. Qualitatively the degree of RV enlargement can be classified as: mild when the RV size is smaller than the LV but larger than three-fourths the size of the LV, moderate when the RV and LV are approximately equal in size, and severe when the RV is larger than the LV.
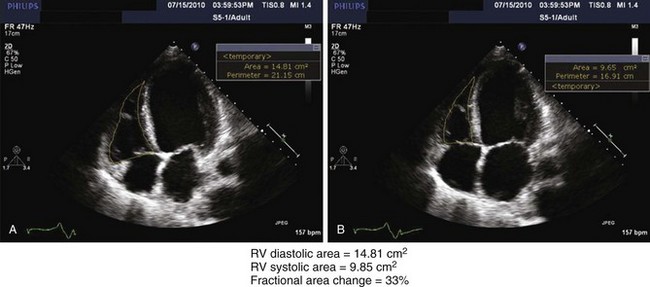
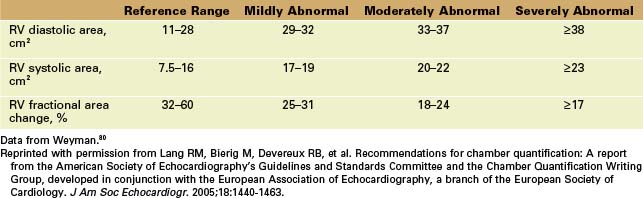
• A quantitative assessment can be obtained in the 4C view by measuring the minor axis at the tricuspid annulus, the minor axis at the midventricular level, and/or a longitudinal axis from the mid-tricuspid plane to the apex at end-diastole. In addition, the endocardial borders of the right ventricular cavity can be traced at end-diastole in the apical 4C view to obtain an RV diastolic area (Figure 4-6A and Table 4-3). Similar to LV measurements, it is important to avoid foreshortening, which may underestimate values.
TABLE 4-3 RECOMMENDATIONS FROM THE AMERICAN SOCIETY OF ECHOCARDIOGRAPHY FOR THE QUANTIFICATION OF RIGHT VENTRICULAR SIZE AND SYSTOLIC FUNCTION
Step 2: Determination of RV Systolic Function
• Assessment of RV size and systolic function can be obtained from the parasternal and subcostal views. However, assessment of RV systolic function is optimally obtained in the 4C view.
• Qualitative judgment remains critically important in assessment of RV systolic function. Typical categorization includes hyperdynamic, normal, mildly decreased, moderately decreased, and severely decreased.
• Because of the complex geometry of the RV, estimates of volume by 2D are relatively unreliable. Thus, quantitative estimation of right ventricular ejection fraction (RVEF) is less common than LVEF. One means of quantitative assessment of RV systolic function is the change in fractional area in the 4C view, which can be obtained using Simpson’s method as with the LV (see Figure 4-6B).
• A second quantitative assessment of RV systolic function can be obtained by measuring the excursion of the tricuspid annulus during the cardiac cycle. A sample volume is obtained from the lateral tricuspid annulus by tissue Doppler imaging (TDI) in the apical 4C view. Normal tricuspid annular plane systolic excursion (TAPSE) is greater than 2.0 cm. Of note, TAPSE has been shown to be decreased in patients with normal RV systolic function but decreased LV systolic function.
Key Points
• 3D echocardiography provides a more complete and reliable assessment of RV size. Quantitative assessment of RV size and RVEF by 3D has been shown to correlate better than that by 2D with other modalities, such as MRI.
• Assessment of RV diastolic function has not been validated to the degree that it has in determination of LV diastolic dysfunction. However, assessment of tricuspid inflow and diastolic parameters of TDI may become increasingly useful, particularly with improvements in 3D speckle tracking, which allows measurement of motion in all directions, not just in the direction of the probe.
LA Volume (LAV)
Step 1: Obtaining 2D Images
• LAV is best obtained in the apical 4C and 2-chamber views using the area-length method. In the final frame before mitral valve (MV) opening, approximating end-systole, endocardial borders of the left atrium are traced. Of note, the pulmonary veins and left atrial appendage should be carefully excluded, and a straight line should be drawn from one mitral annulus to the other (excluding the area immediately under the MV leaflets).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree