10 Echocardiographic Imaging of Single-Ventricle Lesions
Key Points
• Echocardiography (echo) is essential in delineating the anatomy, physiology, and postoperative management of single-ventricle (SV) lesions.
• Most common are the lesions that comprise the hypoplastic left heart syndrome (HLHS):
• HLHS is a spectrum of cardiac defects that result in underdevelopment of the left ventricle (LV) and left ventricular-to-aortic outflow axis.
• The aortic valve (AV) and mitral valve (MV) are either hypoplastic or atretic with no flow across the valve by color Doppler.
• The small non-apex-forming LV is best seen from the subcostal apical or parasternal short axis view.
• Lesions with obstructed PBF:
• DILV with D-malposition of the GVs and subpulmonary stenosis or pulmonary stenosis (PS) (Holmes heart).
This chapter discusses in detail the imaging of these three lesions:
Hypoplastic Left Heart Syndrome
Definition and Prevalence
• Underdevelopment of the LV with associated hypoplasia or atresia of both/either of the AV and MV resulting in the inability of the left heart to support systemic circulation.
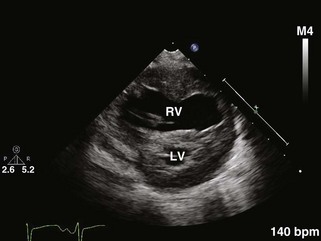
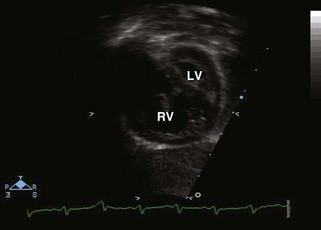
Parasternal Long Axis View (Fig. 10-1)
• Size discrepancy between the two ventricular chambers: the hypoplastic LV posteriorly and the dilated RV anteriorly.
• Endocardial fibroelastosis echobright areas on the endocardial surface of the LV and the MV papillary muscles.
• Hypoplasia of left atrium (LA). A dilated LA raises the suspicion of an intact AS or a restrictive atrial-level communication.
• Patency and mobility of the MV and AV leaflets.
• The MV is usually hypoplastic with thick doming leaflets and abnormal submitral apparatus or a completely atretic MV replaced by a platelike structure. A supravalvar mitral ring might also be present.
• Similarly, AV hypoplasia or atresia may be present and might be associated with subaortic obstruction.
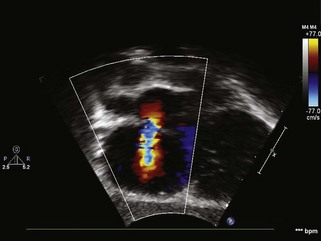
• Right ventricular (RV) and TV function by angling transducer toward the right hip. Color Doppler interrogation will reveal the presence of tricuspid regurgitation (TR). Significant TR is a poor prognostic indicator in HLHS.
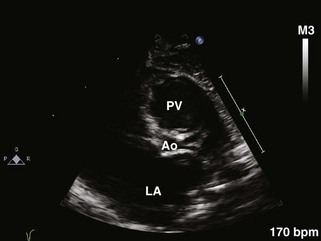
• Assess right ventricular outflow tract (RVOT) and dilated main pulmonary artery (MPA) by angling the transducer toward the left shoulder.
Parasternal Short Axis View
• Ascertain the presence and position or absence of two papillary muscles. The MV is often a “parachute” (a single papillary muscle).
• Normal relationship of the GVs with the hypoplastic aorta posteriorly and to the right of the MPA.
• Evaluate the size and direction of flow across the patent ductus arteriosus (PDA). This is usually obtained from a high left parasternal view moving the transducer superiorly toward the left shoulder and rotating it counterclockwise to about the 1 o’clock position. The branch pulmonary arteries (PAs) are seen from this view (also known as the “three pant leg view” or the trifurcation view).
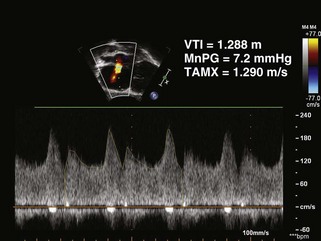
• Doppler interrogation of the PDA is best done from this view. It shows right-to-left flow across the ductus in systole. The direction of flow in diastole is usually dependent on the resistance in the pulmonary vascular bed. The systolic gradient should be assessed for signs of early ductal restriction.
• Presence of ventriculocoronary fistulous connections in the LV myocardium (commonly seen in HLHS with mitral and aortic atresia). This is best performed with color Doppler interrogation of the LV myocardium scanning from base to apex while lowering the color scale because fistulous flow is of low velocity.
• Presence of a VSD using 2D imaging as well as color Doppler interrogation with low color scale to identify small VSDs with low flow velocity in the presence of high pulmonary pressures.
Apical Four-Chamber View
• Size discrepancy between the two ventricles: a non-apex forming LV and a hypoplastic LV. The RV is dilated and hypertrophied. Move the transducer into the axilla (i.e., into a far posteroinferior and lateral position) to optimize the visualization of the hypoplastic LV.
• Degree of MV hypoplasia (thick doming stenotic leaflets) or atresia (platelike structure). In the presence of concomitant aortic stenosis or atresia, MV leaflet excursion may be limited secondary to markedly elevated LV end-diastolic pressure.
• MV inflow and regurgitation. If flow by color Doppler is present, pulsed wave (PW) Doppler and continuous wave (CW) Doppler interrogation of the gradient across the MV will assess the degree of stenosis. The transmitral gradient will be underestimated in the presence of a large atrial communication. Degree of AV hypoplasia or atresia in addition to subaortic stenosis.
• Aortic antegrade flow (if flow present) or regurgitation by color Doppler and spectral Doppler interrogation.
Subcostal Four-Chamber or Coronal View
• Dilated RA and RV with slitlike or diminutive LV prompting the evaluation of left-sided structures (MV, AV, and aortic arch).
• Size discrepancy between the GVs with a dilated MPA and hypoplastic ascending aorta. If ascending aorta is severely hypoplastic, this region may be difficult to visualize.
• Optimal view to evaluate the AS and the number, size, location, and degree of restriction across the atrial communication. Bulging of the AS into the RA or a dilated LA suggests restriction of flow at the atrial level (Figs. 10-4 and 10-5).
• Flow by color Doppler is usually left to right but can be bidirectional in the presence of severe TR or anomalous pulmonary venous connections.
• The spectral Doppler cursor is often parallel to the direction of flow across the AS, allowing accurate measurement of the mean pressure gradient across the AS. Tracing of the gradient over three cardiac cycles is usually done to account for respiratory variation.
• Septum primum attaching directly to the posterosuperior left atrial wall far to the left of the septum secundum.
Subcostal Short Axis or Sagittal View
• Visualizing the PDA as a continuation of the dilated MPA by angling the transducer toward the patient’s left for 2D and Doppler imaging.
• The entire arch can be visualized from this view if the transducer is angled further to the left of the patient’s abdomen. This proves to be useful if suprasternal notch (SSN) imaging is not possible.
• Pulsatility of the abdominal aorta by color Doppler and spectral Doppler. A decrease in pulsatility indicates a coarctation. Flow reversal is seen in the presence of a PDA.
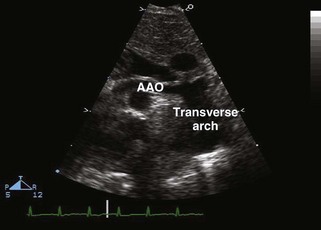
Suprasternal Long Axis View
• Presence of a coarctation, and, in the case of severe coarctation, a juxtaductal posterior shelf is seen with an increased distance between the left carotid artery and the left subclavian artery. Doppler interrogation might not be very helpful in detecting the degree of coarctation in the presence of a large PDA.
• Presence of retrograde flow in the transverse arch and ascending aorta by Doppler interrogation in the presence of critical AV stenosis or atresia.
Suprasternal Short Axis View
• Anomalous pulmonary venous return, especially to a vertical vein. In the presence of an intact AS and mitral atresia, the only egress of blood from the LA might be a levoatrial cardinal vein that crosses posterior to the left PA and most commonly drains into the left innominate vein. Other forms of anomalous pulmonary venous drainage are also seen in HLHS (6%).
Double-Inlet Left Ventricle
Key Points
• Both atria connect through separate right and left atrioventricular valves (AVVs) to a ventricle of LV morphology.
• GVs are most commonly L-transposed, as seen from subcostal sagittal or apical sweep with the PA arising from the LV and the aorta arising from a bulboventricular foramen (BVF) located posteroinferiorly to the dominant ventricle seen.