5 Echocardiographic Evaluation of Prosthetic Valves
Introduction
Key Points
• Echocardiography is the definitive technique for the noninvasive evaluation of prosthetic valve function, both bioprosthetic and mechanical.
• The echocardiographer should be most familiar with the prosthetic valves used at his or her institution; however, patients will present with different prostheses from other institutions, so that sources of reference (such as the tables in this chapter) must be readily available.
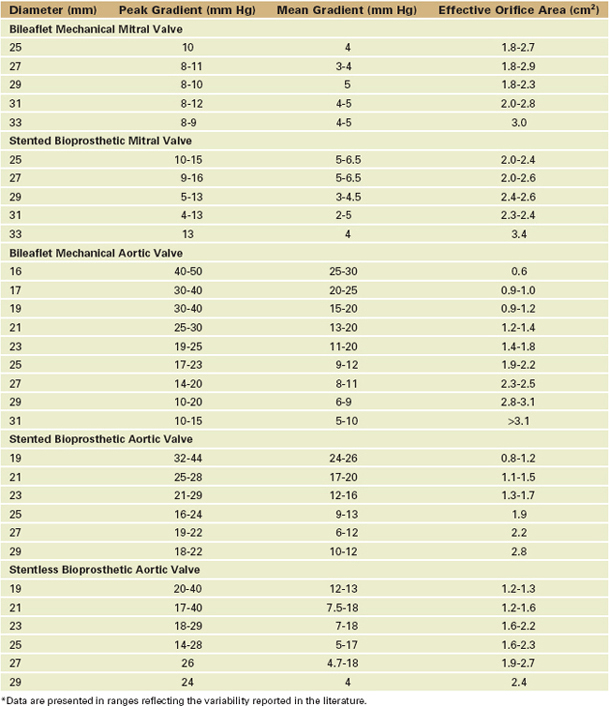
Because there are so many available prosthetic valves, each with very distinctive two-dimensional (2D) and color flow (CF) Doppler acoustic profiles (Table 5-1), the echocardiographer should have access to the type and size of the in situ prosthetic valve and the reason the study has been ordered to focus the study and facilitate image interpretation.
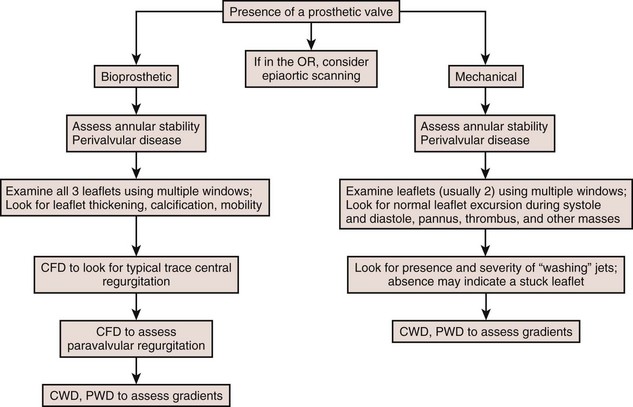
General Considerations With Prosthetic Valves (Figure 5-1)
Types of Prosthetic Valves
Prosthetic valves are usually broadly grouped as biologic or mechanical.
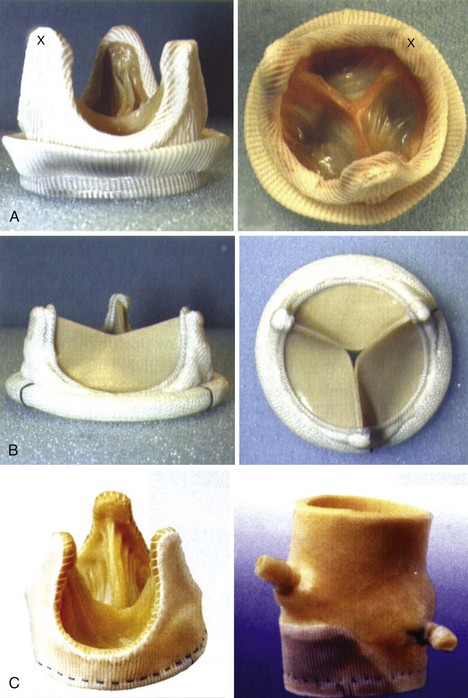
Bioprosthetic Valves (Figure 5-2)
• Tissue valves are composed of three biologic cusps with an anatomic structure similar to that of the native aortic valve (AV). For imaging purposes, it is useful to know whether the valve is stented or stentless.
• The normal flow pattern is similar to that of the native valve, specifically laminar flow with relatively low blood flow velocities.
Stented Bioprosthesis
• Commercially manufactured valves are composed of porcine AV cusps that are sewn into a fabric-covered metal support or cusps made from bovine pericardium using a template and sewn inside of stent supports.
• For stented and mechanical valves, the manufacturer’s valve size refers to the external diameter of the sewing ring, not the actual diameter of the valve orifice.
Stentless Bioprosthesis
In this category, we take liberty by including all replacement tissues without a prosthetic stent. These include the better known stentless valves by St. Jude Medical and Medtronic (see Figure 5-2) as well as autograft and homograft tissues.
• Stentless valves differ based on their origin. They are considered xenografts consisting of either a preparation of porcine aorta or a sculpted bovine pericardium without any added strut support.
• Xenografts differ in method of preservation of valve cusps, anticalcification regimens, and composition and designs of stents and sewing rings.
• Homografts are cadaveric human aortic or pulmonary valves (PVs) that are cryopreserved shortly after being harvested.
• Typically, the valve is harvested along with some of the respective ventricular outflow tract and great vessel, preserved as a block, and trimmed at surgery before implantation.
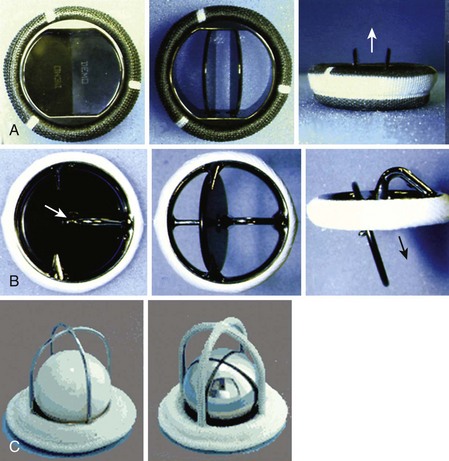
Mechanical Valves (Figure 5-3)
• A wide variety of mechanical valves are currently available. Although this is the case, they all share commonalities.
• The most commonly implanted is a bileaflet valve in which two semicircular disks rotate around struts that are attached to the valve housing. These open to form two large lateral orifices and a smaller central orifice.
• Several other types of mechanical valves were implanted in the past and will be encountered in patients.
• The ball-cage valve houses a spherical occluder contained within a metallic cage. This occluder fills the cage orifice in the closed position but rides above the orifice during antegrade flow.
• Single tilting-disk valves contain a single circular disk controlled by a metal strut that opens at an angle to the annulus plane.
Basic Principles Of The Echocardiographic Examination
Two-Dimensional
• Prosthetic valves should be imaged from multiple windows and angles to overcome the problem of acoustic shadowing that occurs owing to the highly reflective components inherent in many of these valves.
• Nonstandard windows and angles are often required to avoid imaging artifacts. Transesophageal echocardiography (TEE) becomes especially useful in evaluation of prosthetic valves in atrioventricular positions because it provides acoustic access from the atrial side of the valve.
• Prosthetic AV assessment:
• TG windows provide another view of the AV. Although farther from the transducer, these windows could be useful when TE imaging is limited possibly as a result of artifacts. Otherwise, TG imaging provides an opportunity to quantitatively interrogate the valve using pulsed wave (PW) and continuous wave (CW) Doppler.
• Prosthetic PV
• TE imaging is weaker than for other valves. Nonstandard windows may provide a more complete analysis.
• General points of 2D imaging of prosthetic valves
• Failure of a disk to open will significantly reduce the prosthetic valve’s EOA and thus result in increased pressure gradients across that valve.
• Mechanisms of prosthetic valve dysfunction are both similar to and different from those of the native valves. Knowledge of these mechanisms is important to guide the echocardiographer during the assessment.
• The presence of cusp thickening is usually an early sign of primary failure of a bioprosthetic valve.
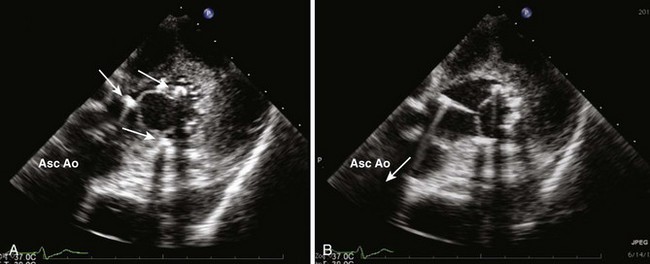
• Increased echo-dense lesions attached to a prosthetic valve sewing ring, stents, disks or occluder, and/or calcifications of bioprosthetic leaflets are signs of possible prosthetic valve pathology and possible failure.
• Incomplete closure of prosthetic valve leaflets can be due to pannus growth, infection, thrombus, or suture materials around the sewing ring or the leaflets.
• Increased distance or separation of the prosthetic valve sewing ring from the native annulus is always pathologic and may appear as an echolucent space, a thickening, or a “rocking” motion of the valve during the cardiac cycle. These abnormal findings suggest a dehiscence of the prosthetic valve.
Doppler Echocardiography
• The Doppler examination includes CF, PW, and CW Doppler examinations. Each method contributes toward qualifying and quantifying flow patterns of both normal and abnormally functioning prosthetic valves. The principles and rationale in utilizing Doppler techniques to qualify, measure, and quantify blood flow velocities, pressure gradients, and effective valve orifice areas of prosthetic valves are similar to that of native valves. However, the “normal” flow profiles of prosthetic valve are NOT assumed to be equal to that of normal functioning native valves.
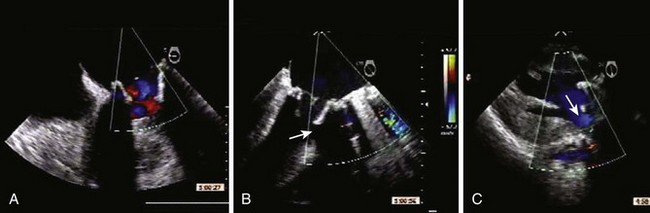
• Given the variety of prosthetic valves available, different systolic and diastolic flow patterns across the valves exist. Although this is the case, assessment of severity of abnormal flows follow similar guidelines. For example, all perivalvular regurgitant leaks are considered abnormal. Those with a vena contracta width of greater than 3 mm have a greater potential to persist and/or worsen regardless of the prosthetic valve type.
Color Flow Doppler
Mechanical Valves
• All mechanical valves display “normal” regurgitant jets, sometimes referred to as “washing jets.” These flows are thought to prevent the formation of thrombi at sites of blood flow stasis. These jets are typically small (vena contracta < 3 mm), have a low velocity and a uniform color pattern (minimal aliasing at most), and do not extend far from the valve plane.
• The “normal” degree of regurgitation of prosthetic valves, detected by CF Doppler, is greater than the trivial amounts seen in normal native valves. The patterns of regurgitation detected by CF Doppler are distinct (“signature patterns”) for each mechanical valve type, corresponding to their fluid dynamics. While casting an identifiable “signature” pattern of regurgitant plumes, the associated regurgitant fraction is less than 10% to 15%.
• Valve types
• Single tilting disk valve
• Antegrade blood flow across a single tilting disk prosthetic valve is characterized by a CF Doppler signal across a major and a minor orifice. CF Doppler will indicate nonlaminar and asymmetrical flow as blood accelerates along the tilted surface of the open disk.
• In the closed position, a single tilting disk normally demonstrates a regurgitation jet directed away from the sewing ring starting at the edge of the major orifice. Surgical preference on implantation determines the open disk position and, hence, the direction of the regurgitant jet normally seen on disk closure.
• Bileaflet valve
• This valve has a complex blood flow profile when interrogated by CF Doppler. In the open position, CF Doppler will demonstrate antegrade flow through two larger lateral orifices and a small central orifice.
• When a bileaflet mechanical valve is imaged in the closed position, multiple “washing” jets of regurgitation are normally seen in the plane parallel to the leaflet-opening plane. All the regurgitant jets are located inside the sewing ring, with two jets originating from where the leaflets meet the housing and a third, central jet originating where the leaflets meet each other.
Bioprosthetic Valves
• Stented bioprosthetic valves display antegrade flow patterns closer to that of a normal native valve through a single orifice.
• “Normal” retrograde or regurgitant jets are centrally directed and do not extend far from the closed valve.
General Points Regarding Color Doppler Assessment
• Pathologic regurgitant jets have higher velocities such that a color-mosaic pattern occurs from aliasing and create significant regurgitant momentum resulting in larger jet areas on CF Doppler imaging.
• The severity of prosthetic valve regurgitation is graded by criteria similar to that used for the native valve. The extent of the regurgitant jet into the receiving chamber as measured by CF Doppler (either the width of the vena contracta or the ratio of the CF Doppler jet area to the area of the atrium or the ratio of the width of the aortic insufficiency [AI] jet to the width of the left ventricular outflow tract [LVOT]) is often utilized.
• CF Doppler-detected regurgitant jets that originate outside of the prosthetic sewing ring (paravalvular) are always pathologic.
• Although paravalvular regurgitation is always abnormal, small jets are often imaged on CF Doppler immediately after valve implantation in the operating room. To be clinically and hemodynamically insignificant, these jets should be small in comparison with the total circumference of the sewing ring they originate from. Many frequently resolve shortly after reversal of heparinization.
• Paravalvular regurgitation is not uncommon and results from a combination of surgical technique and the condition of the native annulus. A heavily calcified annulus complicates the placement of a prosthetic valve and may require extensive surgical débridement and repair before placement. These variables may increase the occurrence and severity of paravalvular regurgitation.
• For prosthetic valves in the mitral and tricuspid positions, it may be very difficult to detect pathologic regurgitation on transthoracic imaging. If suspected, it is an indication for TEE imaging. With TEE, CF Doppler imaging of a prosthetic valve in the mitral position is optimal because the ultrasound beam has access to the chamber receiving the regurgitant flow without intervening acoustic shadowing from crossing the prosthesis.
Pulsed Wave and Continuous Wave Doppler
• PW and CW Doppler modes provide quantitative evaluation of the prosthetic valve. Assessments regularly performed include peak transvalvular velocity (Vmax), velocity time integral (VTI), peak and mean transvalvular pressure gradients, calculation of prosthetic valve area, and measurement of a dimensionless index in stenotic valves.
• These assessments are based on basic principles of physics including
• The simplified Bernoulli equation, ΔP = 4 × (V2 )2, forms the basis of much of the quantitative analysis including subvalvular and valvular velocities and gradients.
• For sites in which flow velocity proximal to the site of interest is high (>1.4 m/s), the simplified Bernoulli equation is not applicable and the proximal velocity must be included:
• The angle of interrogation (i.e., the angle between the Doppler beam and blood flow) should be less than 20 degrees to allow acceptable accuracy of blood flow velocities.
• For lower velocity flows (i.e., no aliasing), PW Doppler can be employed. The aliasing velocity is, in part, determined by the distance of the area of interest from the ultrasound probe. For higher velocity flows (i.e., exceeds the aliasing velocity), CW Doppler should be employed to allow assessment of high velocity flows.
• Conservation of mass/continuity equation
• This principle states that mass, flow, or volume (or stroke volume) measured at one site is equal to another provided that there are no intervening channels (inputs or outputs).
• The basis of this assumes that volume can be measured by the equation VTI × Area (πr2; r = radius of the site of interest). This equation assumes a circular and non-changing orifice.
• If the volume or mass can be measured at a reference site, and the VTI across the valve can be obtained, then the EOA of the valve can be calculated using the continuity equation:
• Although the peak velocities of VTI for the reference are typically obtained using PW Doppler to target the same site at which the radius is measured, the respective Doppler values of the prosthetic valve are obtained using CW Doppler in order to measure flows across the vena contracta.
General Points
• Compared with a normal native valve, prosthetic valves have a smaller EOA. Antegrade velocities and pressure gradients across a normally functioning prosthetic valve are higher than a normal native valve.
• Smaller prosthetic valves may have hemodynamic profiles similar to that of mild stenosis for the given valve position (e.g., a 19 mm-prosthetic valve has an EOA ranging from 1.0-1.1 cm2).
• Clinical application of Doppler-derived pressure gradients across mechanical valves may not be straightforward because a number of variables contribute to its value
• Manufacturers publish data on the flow characteristics of each specific prosthetic valve and its various sizes. Published in vivo data vary more than in vitro data owing to variability in hemodynamic functions. Given the wide range of pressure gradients across any specific prosthetic valve, it may be best to determine the valve EOA or measure a dimensionless index across the valve and its outflow tract (described later).
• Doppler-derived peak and mean pressure gradients across bioprosthetic valves correlate closely with directly measured pressure gradients. For these valves, there is a single orifice.
• Doppler-derived pressure gradients across mechanical valves present a more complex clinical scenario. This has been best studied for the bileaflet valve where two hemicircular disks hinge open to form two larger semicircular lateral orifices and a smaller slitlike central orifice. Within the narrow central flow stream, higher blood velocities occur owing to local acceleration forces. Whether or not CW Doppler overestimates the transvalvular velocities by recording flow across the central smaller orifice is an issue. Theoretically, the pressure gradient across a narrower orifice of this valve will be identical to the peripheral ones because blood flow through the orifices is directly related to the orifice size.
• Utilizing pressure gradients across prosthetic valves as the sole indicator of functionality is limited because transvalvular gradients will vary directly with patient’s cardiac output. Therefore, when valve patency is in question, it is important to determine the EOA of the prosthetic valve.
• PPM refers to an implanted prosthetic valve whose EOA is small relative to the patient’s desired functional level. Implanted prosthetic valves have the unique possibility of functioning normally but still performing in a clinically detrimental manner through “PPM.”
• This has been measured by comparing the EOA with the patient’s body surface area (BSA) to obtain an indexed valve area: iEOA. The undersized valve’s EOA results in
• Decreased improvement of proximal chamber function or, in the case of aortic stenosis, a reduced regression of ventricular hypertrophy.
• Although indexing of EOA to a patient’s BSA may not be appropriate in morbidly obese patients, it must still be considered because the patient will still need to function with the same body mass. For similar BSAs, obese patients have lower cardiac output requirements because fat is a vessel-poor tissue.
• A recent study found that PPM did not correlate with adverse clinical outcomes in patients with a body mass index greater than 30 kg/m2. PPM may not have clinical importance in the elderly (≥75 years old) or the smaller patient (≤1.7 m2).
• PPM can occur at any site at which prosthetic valves are implanted, but most clinical work has focused on prosthetic valves in the aortic position. Pressure gradients across prosthetic valves in the aortic position increase exponentially when the iEOA is 0.8 to 0.9 cm2/m2 or less. Based on these clinical data, PPM is considered to be hemodynamically insignificant if the EOA is 0.85 cm2/m2 or greater, moderate if the iEOA is between 0.65 and 0.85 cm2/m2, and severe if iEOA is less than 0.65 cm2/m2.
• The reported prevalence of moderate and severe PPM in aortic prosthetic valves varies considerably but should be deceasing as the surgical community gains awareness of the impact of PPM on clinical outcomes.
• PPM results in reduced short- and long-term survival, especially when associated with preexisting left ventricular dysfunction. The severity of the PPM also correlates with reduced patient survival.
• PPM is best avoided by the preimplantation calculation of a valve’s functional EOA against the patient’s BSA and the choice of an appropriate sized valve.
• PPM has been reported for prosthetic valves implanted in the mitral position. Limited clinical data suggest that the iEOA on mitral prostheses should be greater than 1.2 to 1.3 cm2/m2 to avoid deleterious pressure gradients across the valve. PPM of mitral prosthetic valves has been reported to result in persistent pulmonary hypertension and reduced long-term survival.
Key Points
• The opening and closing of the mechanical valve disks or bioprosthetic cusps must be evaluated before decannulation so that abnormalities (see Cases on companion website) may be corrected before the patient leaves the operating room.
• Color Doppler in bioprosthetic valves often shows a small central jet of regurgitation; with mechanical prostheses, intravalvular washing jets are normally seen (see Cases on companion website).
• A small degree of paravalvular regurgitation, although abnormal, often resolves after the administration of protamine.
• PW and CF Doppler are used to assess transvalvular gradients. Although the accuracy in bioprosthetic valves seems intuitive, the complex flow characteristics of mechanical valves may be problematic.
• Evaluation of the functionality of a patient’s particular valvular prosthesis must be made in light of the manufacturer’s published data on the particular valves characteristics and, of course, on the patient’s clinical context.
• Valve gradients are often higher than expected in the immediate post-bypass period and usually relate to the high flow state that exists; however, extremely high valvular gradients are unusual and should prompt close echocardiographic examination using TEE or alternative techniques such as epicardial echocardiography.
Prosthetic Mitral Valve
Key Points
• The severity of regurgitant flow is quantitated in a fashion similar to that of native valves. Special attention must be paid to the seating of the valve and the presence of pannus, thrombus, calcification or vegetation, and coexistent prosthetic stenosis.
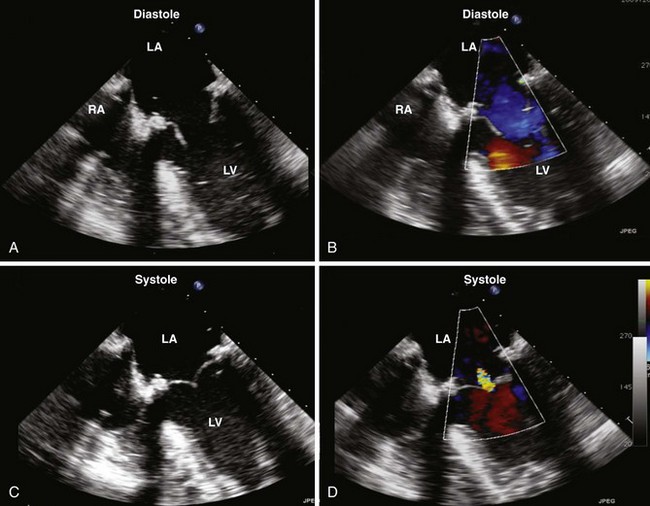
Step-by-Step Examination (Figure 5-4)
• The 2D examination of the prosthetic MV is accomplished from a number of echocardiographic windows with particular emphasis on
• Midesophageal (ME) windows from 0 to 150 degrees including but not limited to the standard ME windows.
• The CF, PW, and CW Doppler examinations of the prosthetic MV can be performed from the ME windows because the Doppler beam can be aligned with the direction of blood flow.
Step 1: Two-Dimensional Examination (Figure 5-7; see also Figure 5-4)
• The stability of the valve should be determined and whether or not the prosthesis is rocking. As a rule, the prosthetic valve should sit firmly within its surrounding tissue.
• For mechanical valves, imaging perpendicular to the leaflets will allow one to see the opening and closing by noting the leaflet edges. Imaging parallel to the valve leaflets is not likely to visualize the leaflet edges opening and closing. If the valve is bileaflet and placed anatomically, optimal imaging is done at or close to a four-chamber orientation; if placed antianatomically, optimal imaging is done at approximately 50 to 80 degrees.