17 Echocardiographic Assessment After Heart Transplantation
Background
• Surgical technique involves left atrial anastomosis to avoid pulmonary vein (PV) stenosis as a consequence of PV anastomosis.
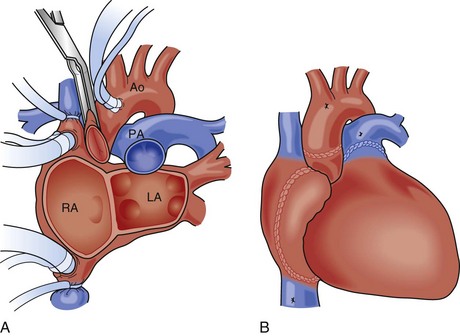
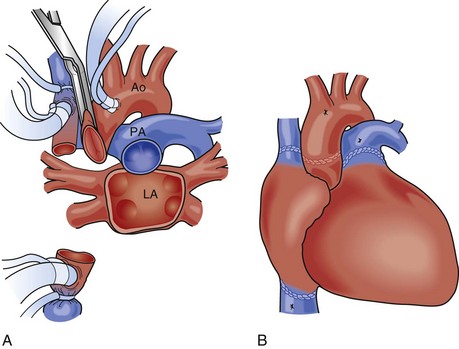
• Systemic venous connections are performed through a right atrial anastomosis in young children (Fig. 17-1) or a bicaval anastomosis in older children and adults (Fig. 17-2).
• Arterial connections are generally created in the ascending aorta (Ao) and main pulmonary artery (MPA).
Overview of Echocardiographic Approach
• The focus of the echocardiographic exam shifts depending on the time since transplantation (Table 17-1).
• In the immediate post-transplantation period, all surgical connections should be carefully interrogated. In addition, acute graft dysfunction, pulmonary hypertension (PHTN), and pericardial effusions are major concerns.
• Surgical connections and graft function will need to be monitored indefinitely after transplantation.
• Other centers monitor for rejection using cardiac biopsies, and echo can be used to guide the bioptome and screen for complications afterward.
TABLE 17-1 USE OF ECHOCARDIOGRAPHIC MODALITIES AFTER TRANSPLANTation
| Immediately After Transplantation | 1 Week to 1 Year After Transplantation | >1 Year After Transplantation |
|---|---|---|
| TEE: acute graft dysfunction (RV, LV) | TTE: RV function | DSE: graft coronary artery disease |
| TEE and TTE: RV pressure | TTE: RV pressure | |
| TEE and TTE: surgical connections | TTE: surgical connections | TTE: surgical connections |
| TTE: acute rejection | TTE: rejection | TTE: rejection |
| TTE: pericardial effusion | TTE: graft dysfunction | TTE: graft dysfunction |
Key Points
Postoperative concerns after heart transplantation that should be evaluated by echo include:
Anatomic Imaging
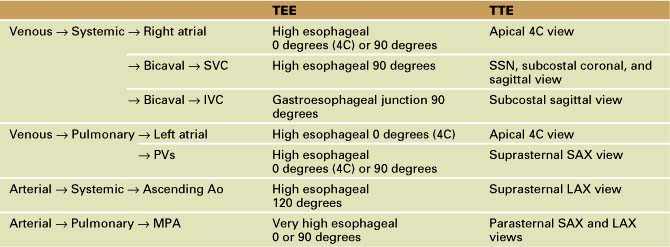
• All anastomoses should be interrogated in the appropriate views, either with transesophageal echo (TEE) or transthoracic echo (TTE) (Table 17-2).
TABLE 17-2 Transesophageal and transthoracic echocardiographic views to assess the anastomoses between the donor heart and recipient
Venous Anastomoses
• Pulmonary side:
• Left atrial anastomosis of the donor left atrium to recipient residual left atrial cuff is performed to avoid PV anastomosis.
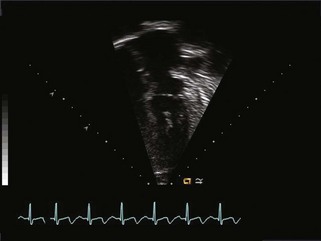
• This produces an echocardiographic image of gross atrial enlargement with an echodense suture line in the four-chamber (4C) view, which should not be mistaken for thrombus (Fig. 17-3).
• Systemic side:
• Right atrial anastomosis is performed in younger (smaller) children and bicaval anastomoses in older children and adults.
• Right atrial anastomosis also creates an image of an enlarged right atrium with echodense suture line.
• Superior vena cava (SVC) flow velocity can be recorded from the suprasternal notch (SSN) or subcostal images. Normal SVC flow is biphasic with two distinct waves (S and D waves). A loss of this biphasic pattern or an increase in flow velocity of more than 1 m/s indicates obstruction.
• Occasionally, abnormal congenital pulmonary and systemic connections in the native heart warrant construction of atrial baffles, which should be interrogated for obstruction.
Arterial Anastomoses
• Pulmonary artery (PA):
• MPA anastomosis should be interrogated for stenosis in the parasternal short axis and long axis views on TTE.
• Occasionally, when native central PAs are abnormal, donor PAs are used, and the anastomosis with native PA tissue is made in the branch PA. These distal anastomoses will be more prone to stenosis but are sometimes poorly seen by echo, especially on TEE. When poorly seen, the presence of PA flow can be confirmed indirectly by presence of pulmonary venous flow.
Valve Regurgitation
• There is an increased frequency of tricuspid valve (TV) regurgitation in the transplant recipient population due to multiple factors:
Pericardial Effusion
• Pericardial effusion is relatively common after heart transplantation and has a different differential diagnosis than in the nontransplant recipient (Box 17-1).
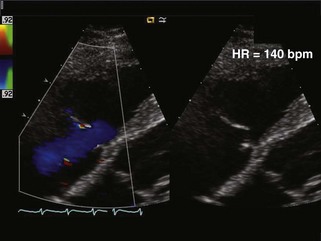
• An effusion in the immediate postoperative period is most likely due to a surgical hematoma, but rejection is the most common cause of a new pericardial effusion at any other time after heart transplantation (Fig. 17-5).
• Pericardial effusions should be evaluated for size and signs of tamponade, according to methods described in Chapter 16.
Physiologic Data
Early Post-transplantation
• TEE starts with a transgastric short axis view (probe advanced into stomach in a neutral position with anteflexion) to evaluate left ventricular systolic function (fractional shortening).
• Right ventricular dilation and systolic dysfunction are relatively common in the early post-transplantation period due to graft preservation injury and/or preexisting PHTN.
Systolic Function
• Left ventricular systolic function (ejection fraction, fractional shortening, and posterior wall thickening fraction) is an important part of the TTE exam anytime after transplantation.
Diastolic Function
• LV diastolic function is often abnormal in early post-transplantation period due to perioperative ischemia, reperfusion injury, systemic hypertension, or side effects of immunosuppressive medications.
• Normalizes in the majority of patients within the first couple of months, but can remain abnormal.2